Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Assessing the effect of culturally specific audiovisual educational interventions on attaining self-management skills for chronic obstructive pulmonary disease in Mandarin- and Cantonese-speaking patients: a randomized controlled trial
Authors Poureslami I, Kwan S, Lam S, Khan N, FitzGerald JM
Received 30 January 2016
Accepted for publication 4 April 2016
Published 3 August 2016 Volume 2016:11(1) Pages 1811—1822
DOI https://doi.org/10.2147/COPD.S105408
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Iraj Poureslami,1,2 Susan Kwan,3 Stephen Lam,4,5 Nadia A Khan,6,7 John Mark FitzGerald 8,9
1Respiratory Division, Department of Medicine, Faculty of Medicine, University of British Columbia, Vancouver, Canada; 2Department of Graduate Studies, Centre for Clinical Epidemiology and Evaluation, Vancouver Coastal Health Research Institute, Vancouver, Canada; 3Respiratory Department, Burnaby Hospital, University of British Columbia, Burnaby, Canada; 4Respiratory Division, University of British Columbia, Vancouver, Canada; 5Department of Integrative Oncology, BC Cancer Research Centre, Vancouver, Canada; 6Department of Internal Medicine, Faculty of Medicine, University of British Columbia, Vancouver, Canada; 7Department of Internal Medicine, Providence Health Care Authority, Vancouver, Canada; 8VGH Divisions of Respiratory Medicine, University of British Columbia, Vancouver, Canada; 9Respiratory Medicine, Vancouver Coastal Health Authority, Vancouver Coastal Health Research Institute, Institute for Heart and Lung Health, The Lung Centre, Gordon and Leslie Diamond Health Care Centre, Vancouver, Canada
Background: Patient education is a key component in the management of chronic obstructive pulmonary disease (COPD). Delivering effective education to ethnic groups with COPD is a challenge. The objective of this study was to develop and assess the effectiveness of culturally and linguistically specific audiovisual educational materials in supporting self-management practices in Mandarin- and Cantonese-speaking patients.
Methods: Educational materials were developed using participatory approach (patients involved in the development and pilot test of educational materials), followed by a randomized controlled trial that assigned 91 patients to three intervention groups with audiovisual educational interventions and one control group (pamphlet). The patients were recruited from outpatient clinics. The primary outcomes were improved inhaler technique and perceived self-efficacy to manage COPD. The secondary outcome was improved patient understanding of pulmonary rehabilitation procedures.
Results: Subjects in all three intervention groups, compared with control subjects, demonstrated postintervention improvements in inhaler technique (P<0.001), preparedness to manage a COPD exacerbation (P<0.01), ability to achieve goals in managing COPD (P<0.01), and understanding pulmonary rehabilitation procedures (P<0.05).
Conclusion: Culturally appropriate educational interventions designed specifically to meet the needs of Mandarin and Cantonese COPD patients are associated with significantly better understanding of self-management practices. Self-management education led to improved proper use of medications, ability to manage COPD exacerbations, and ability to achieve goals in managing COPD.
Clinical implication: A relatively simple culturally appropriate disease management education intervention improved inhaler techniques and self-management practices. Further research is needed to assess the effectiveness of self-management education on behavioral change and patient empowerment strategies.
Keywords: COPD, educational material, cultural background, self-efficacy, self-management, Chinese community
Introduction
Chronic obstructive pulmonary disease (COPD) continues to be an important cause of morbidity and mortality and a driver of health care costs worldwide.1–5 It is estimated that by 2020, COPD will be the third leading cause of death worldwide.6–8
Successful long-term management of COPD requires active patient involvement in self-management practice.7 Achieving success in self-management has been associated with an increased sense of patient self-efficacy9–11 and high levels of patient confidence in their ability to understand and follow providers’ instructions and recommended action plans.12,13 Despite the importance of teaching patients how to manage their disease, there is inconclusive evidence regarding the effectiveness of educational interventions in supporting skill attainment. Studies have found improvements in COPD self-management using case-managed educational interventions.14–16 Other studies have shown that patient education may increase disease-related knowledge, but does not always ensure that patients gain the necessary self-management skills.17,18 This lack of effect may, in some instances, be a function of patients’ failure to fully master self-management.9,10,19,20 Multiple factors affect patients’ ability to learn and adhere to care plans, including patients’ perception of their disease, type of treatment or medication, quality of patient–provider communication, and impediments to comprehension and uptake posed by language and cultural barriers.5,7,8,21
The mixed results in the literature make it clear there is more to learn about designing and implementing educational interventions to effectively empower patients to self-manage COPD. Research has shown that people learn better when provided with audiovisual materials compared to print handouts.14–16 Our previous research indicates a practical way to reach patients is by developing education videos with direct involvement of community and professionals.18,22–24 Immigrant Chinese patients, for example, sometimes understand better when taught by peer educators,23,25 yet these patients also hold their physicians in high regard, and therefore may be more receptive to instruction from an authority figure.23,25
Immigrant groups especially those with English as a second language – who face barriers accessing and understanding health information provided in English – are at increased risk of having less well-controlled COPD.18,20,25 Chinese immigrants are one of the largest and fastest growing cultural communities in North America.26,27 To date, little research has been done in Canada to evaluate the impact of culturally specific educational interventions on the ability of Chinese patients to learn COPD self-management. The goal of this randomized controlled trial (RCT) was to assess the relative effectiveness of culturally specific and linguistically appropriate educational materials on attainment of self-management skills with COPD patients from Mandarin- and Cantonese-speaking communities in Metro Vancouver. We were interested in understanding what kind of educational sources (video or pamphlet) would work best for immigrant Chinese COPD patients. The research questions were as follows: 1) whether patients exposed to audiovisual materials show better skill attainment in postintervention on COPD self-management skills than those exposed to print handouts and 2) whether skill attainment differs by source of educational videos (clinician-led, peer role-played, or both videos).
Materials and methods
Study design
This was a single-center, RCT. The study participants were randomly assigned to three intervention groups and one control group. The intervention groups were exposed to a peer role-played self-management video (lay video), a clinician-led self-management video (clinician video), or both. The control group was provided with a pictorial self-management pamphlet. Outcomes were measured using direct observation of inhaler technique and validated COPD assessment questions. The study was approved by the University of British Columbia Office of Research Ethics and was registered at ClinicalTrials.gov (NCT01474707). All participants gave written informed consent before enrolling into the study.
Study recruitment
Study participants were recruited from outpatient respiratory clinics. Collaborating physicians identified and referred potential candidates. Bilingual facilitators contacted candidates and explained the study objectives, process, and participants’ rights and risks and obtained signed consent in participants’ native language. To be included, participants were required to fit into the following criteria: confirming a COPD diagnosis by spirometry; being symptomatic; an immigrant to Canada within past 20 years; residing in Vancouver; and speaking Mandarin or Cantonese. Spirometry was performed to determine the severity of COPD according to Global initiative for chronic Obstructive Lung Disease criteria.1,2,21
Randomization
Block randomization was applied to assign patients into the study groups, including three experimental groups and one control group. Because of our previous knowledge regarding the re-effectiveness of educational pamphlets on disease management, we applied an unequal randomization approach to deliberately assign more participants in intervention groups. Our aim was to ensure enrolling adequate numbers of participants in the intervention groups to detect the effect of educational interventions on attainment of self-management skills. It is a helpful approach, particularly when a 2:1 ratio is employed,28,29 and we managed our random allocation close to a 2:1 ratio for each intervention/control pairing.
Intervention process
The culturally specific educational interventions – two videos (one lay and one clinician video) and one pamphlet in each language – were developed by the research team using a community-based participatory approach17,22 that actively involved professionals and patients from Chinese communities in development and testing. To select the format of educational intervention, besides evidence from the literature, our participants in initial focus groups were interested in and requested to watch educational videos performed by both professionals (doctors) and layperson (peer patients). In designing our audiovisual intervention, we created two versions enabling comparison between the effects of instruction provided by a layperson and a clinician. The aim was to explore whether any added video can be an advantage to learn about and understand their chronic disease management by exposure to both sources of information (patient role-played and physician-led videos). The patients received necessary training during a 2-day “popular theater workshop”30,31 to draft the video scripts and role-play in the lay video clips. The collaborating physicians who presented in the clinical videos were culturally and linguistically congruent and had previous experience in developing educational videos.
In the “lay video,” patients role-played a scenario offering opinions and narratives about COPD self-management in a 12-minute video clip. Two lay videos with similar content in Mandarin and Cantonese languages were developed. The “clinician video” was a 20-minute physician-led video, providing clinical information about COPD symptoms and self-management strategies. We applied the same content to develop the clinical videos in the two languages. In addition, in the last scene of both lay and clinician videos, an experienced respiratory educator from the same language group as the patients’ demonstrated the correct use of different inhalers.
The pictorial pamphlet for the control group used the same content from the active intervention in a printed format. To ensure that the content of materials was equivalent for Mandarin and Cantonese languages, we first developed the written materials in English and then asked professional translators to translate the information, as well as back translation, to the two target languages. To create easy-to-read and understandable written materials, the pamphlets were developed at grade 5 literacy level, using the Fry Readability Graph system.32 Also, we used illustrations and photographs in the pamphlets, with concise captions, to provide relevant information regarding the necessary steps for the proper use of inhalers.
The intervention consisted of a single exposure to educational materials. Group 1 (n=22) was assigned the clinical video; Group 2 (n=26) watched the lay video; Group 3 (n=29) watched both videos; and Group 4 (n=14) served as the control group and read the pamphlet. Patients watched their video(s) or read their pamphlet individually at our clinic.
Outcome measurement and data collection
The primary outcomes of interest were change in “inhaler technique” (ability to correctly use an inhaler and differentiate between different inhalers) and “self-efficacy” (patient’s perceptions/beliefs and their confidence to correctly use medication and recognize exacerbations to act properly) from baseline to 3 months postintervention. The secondary outcome was “improved patient understanding of Pulmonary Rehabilitation (PR) program procedures.” All outcomes were measured at baseline, then at 4 weeks and 3 months after intervention; improvement in skills following this time lapse was considered evidence of learning attainment.
Data were collected over a 4-month period through three in-person assessments. The baseline assessment preceded the intervention; the postintervention assessment occurred immediately following the intervention (4 weeks after baseline); a follow-up assessment occurred 3 months following intervention. Data collection was conducted by trained bilingual facilitators, blinded throughout the study, as was the data analyst. An identical questionnaire was used in the three different assessments.
The inhaler technique was measured by assessing two behaviors: 1) correct use of an inhaler, by applying a 10-item-validated inhaler-specific checklist;33 and 2) the ability to correctly distinguish between inhaler types (either reliever or preventer therapy), and participants were given a pass/fail score.34,35 Correct use was determined by direct observation while the participants were asked to demonstrate the use of an inhaler and describe the steps they were taking in doing so. The percentage of correct steps in inhaler use was then analyzed. For participants using multiple inhalers, the success rate was the percentage of correct steps taken across all inhalers.34,36 Participants’ verbal accounts of steps taken (the teach-back technique36) were assessed and recorded by two observers.
Self-efficacy was measured using a short version of validated COPD Self-Efficacy Scale.37,38 These questions aimed to address participants’ self-assessed sense of 1) being informed about COPD and its management, 2) being prepared to manage exacerbations, 3) their ability to remain calm during an exacerbation, 4) their ability to achieve goals in COPD management, and 5) their ability to find solution when facing COPD-related problems. The responses to each item were rated on a five-point scale ranging from “not at all confident” (1) to “totally confident” (5).
Patient understanding of pulmonary rehabilitation (PR) procedures was assessed using the Canadian Thoracic Society COPD assessment guidelines.39 Our team developed a passage of text and then asked participants to answer related questions in the checklist to determine their grasp of PR procedures. Responses were coded as correct (1) or incorrect (0). Given the lack of an existing COPD self-management questionnaire in Chinese language, the study assessment tool also included some questions developed by the research team using the Bristol COPD Knowledge Questionnaire40 regarding disease-related knowledge and actions needed to prevent or treat a COPD exacerbation.
Sample-size calculation
Chinese populations in Canada have been found less likely to participate in clinical trials, specifically conducted by non-Chinese researchers. Therefore, they are considered hard-to-be-enrolled patients in the studies. Besides, COPD is more common among males; therefore, more male samples than females were observed in this study. With a total sample size of 100 subjects for the educational intervention, we estimated that we could identify mean differences between the four experimental groups and two ethnic groups with an effect size of 0.45 in asthma self-management and inhaler techniques with 80% statistical power and a two-sided significance level of 5%. In other words, we predicted that 45% of the improvement observed in the outcomes of interest among the experimental groups would be the result of our intervention. For instance, inhaler technique score or understanding of physician’s instruction score of the average person in the experimental groups would be 0.45 standard deviations above the average person in the control group. In terms of sex selection, we enrolled more male COPD patients, as in Chinese population, males are more likely to suffer from COPD than females (8.3%–18.9% males vs 3.8%–7.1% females).41
Data analysis
At baseline, χ2 tests were used to compare categorical demographic variables, and two independent samples t-tests were used to compare continuous and ordinal variables. The baseline assessments showed no statistically significant differences among the participants in four study groups for the outcomes of interest. In the analysis, we calculated the improvement in mean differences (MD) in outcomes of interest from baseline to follow-up assessment in intervention groups, compared to improvement in the control group. Missing data were imputed in SAS (version 9.3, SAS Institute Inc., Cary, NC, USA) using multiple imputed chained equations.42 Analysis of variance was used to compare the effect of the educational materials on outcomes across the four groups. Analysis of covariance was also used to adjust outcomes for age (≤75≥76), sex (F/M), educational level (LOW [less than high school]/HIGH [high school and higher]), and disease severity (Stages I–IV, based on Global initiative for chronic Obstructive Lung Disease criteria).
Results
Participation
Participants were recruited between December 2011 and August 2013. Initial recruitment included 161 patients, from which 27 participated in focus groups to prioritize educational materials’ topics and content, 15 patients helped in the development of materials and role-play in the videos, 19 patients participated in pilot testing (for clarity, cultural relevance, and acceptability) and finalizing the educational materials, and the remaining 100 patients were invited to participate in the main study (Figure 1). From the enrolled patients, two participants were excluded because of the results of the spirometry test, and seven patients withdrew due to death, left Canada, or were disabled before the randomization. In total, 91 patients were randomized to four study groups (Table 1). The patients who participated in the group sessions, development of the intervention materials, and pilot testing were not involved in the RCT.
  | Figure 1 Patient enrollment and attrition. |
Primary outcomes
Inhaler technique
Within-group changes
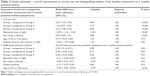
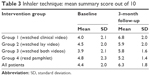
The inhaler technique (maximum score of 10) improved in the three intervention groups compared to the control group, with the greatest improvement in Group 1 who watched the clinician video (MD =2.34; 95% confidence interval [CI] =1.34–3.34; P<0.001), followed by Group 2 who watched the lay video (MD =1.92; 95% CI =0.91–2.93; P<0.001), and then by Group 3 who watched both videos (MD =2.13; 95% CI =1.08–3.18; P<0.001) (Table 2). The mean summary score of proper inhaler use among the four intervention groups from pretest to 3 months postintervention follow-up test can be found in Table 3.
  | Table 3 Inhaler technique: mean summary score out of 10 |
Intervention effects
A comparison of inhaler technique for the entire sample showed an improvement at the postintervention assessment compared to baseline (MD =1.79; 95% CI =1.32–2.26; P<0.001). Improvement was still apparent at the 3-month follow-up (MD =1.68; 95% CI =1.22–2.13; P<0.001) (Table 2). Improvement in the inhaler technique was significantly lower in subjects with low education compared to those with high education (MD =−0.59; 95% CI =−1.16 to −0.03; P<0.05). Males showed a greater improvement than females (MD =0.53; 95% CI =0.04–1.01; P<0.05). There were no significant differences in correct use based on age or disease severity. Furthermore, there was no significant difference in improvement in the ability to differentiate between rescue and preventer inhalers across the four study groups when sex, education, and disease severity were taken into consideration. However, subjects over 75 years of age showed significantly more improvements at differentiating inhalers relative to those aged 75 and younger (MD =−0.35; 95% CI =−0.69 to −0.02; P<0.05).
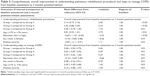
Self-efficacy
Improvements in the self-efficacy of intervention group participants relative to the control group were mixed for the measures (Table 4). For instance, significant improvement in the “ability to manage COPD exacerbations” was observed among the three intervention groups compared to control group, with Group 1 having the greatest improvements (MD =1.20; 95% CI =0.38 to −2.02; P<0.01), followed by Group 2 (MD =0.96; 95% CI =0.09–1.82; P<0.05) and Group 3 (MD =0.87; 95% CI =0.04–1.71; P<0.05). For this question, sex, education level, age, or disease severity did not affect the results. While in terms of the question “being informed about COPD,” only Group 3 showed a significant improvement (MD =0.12; 95% CI =−0.65 to −0.90; P<0.05). Those with lower education levels showed significantly less improvement compared to those with higher education (MD =−0.59; 95% CI =−1.1 to −0.09; P<0.05), and younger subjects (≤75 years) did worse than older ones (MD =−0.42; 95% CI =−0.74 to −0.06; P<0.05). Analyses for sex and disease severity indicated no significant differences. Furthermore, only Group 2 showed a significant improvement in the question about: “remaining calm when facing a COPD worsening” (MD =0.80; 95% CI =−0.02–1.58; P<0.05). Males showed significantly more improvement in response to this question than females (MD =0.33; 95% CI =0.02–0.65; P<0.05); there were no significant differences based on age, education level, or disease severity. Moreover, regarding the question “ability to achieve goals in managing COPD,” both Groups 1 and 3 showed a significant improvement (Group 1: MD =1.28; 95% CI =0.36–2.19; P<0.05; Group 3: MD =1.05; 95% CI =0.08–2.02; P<0.05). Patients with lower education showed significantly less improvement (MD =−0.78; 95% CI =−1.54 to −0.01; P<0.05). Analyses for age, sex, and disease severity showed no significant differences. Finally, in response to question about “ability to self-manage COPD symptoms,” only Group 3 showed a significant improvement (MD =0.38; 95% CI =−1.18 to 0.41; P<0.05). Males showed less improvement in their responses relative to females (MD =−0.44; 95% CI =−0.87 to −0.02; P<0.05). Relationship to age, education level, and disease severity showed no significant differences for this question.
Secondary outcome
Understanding PR procedures
Only Groups 1 and 2 had significantly improved understanding of PR procedures, compared to the control group: Group 1: MD =2.14; 95% CI =0.73–3.16; P<0.05) and Group 2: MD =2.22; 95% CI =0.86–3.30; P<0.05) (Table 5). Subjects aged 75 and younger showed more improvement than older subjects (MD =0.81; 95% CI =0.22–1.41; P<0.01), whereas subjects with low education showed less improvement that those who were more educated (MD =−0.65; 95% CI =−1.32 to −0.02; P<0.05). There were no significant differences in improvement based on sex or disease severity.
Discussion
This RCT assessed the effects of educational interventions on the attainment of inhaler techniques, self-efficacy, and understanding PR procedures in three intervention groups (watched either lay or clinician videos, or both) compared to a control group who received only educational pamphlet. The baseline assessments showed no statistically significant differences among the participants in four study groups for the outcomes of interest. This finding suggests that the observed differences in the follow-up assessment are more likely the result of intervention effects. As anticipated, a greater effect for the audiovisual interventions was observed across and within study outcomes. For inhaler technique, all the intervention groups showed a greater improvement in correct use after watching structured videos compared to the control group. Group 1 (clinician video) showed the greatest improvement – a finding in keeping with previous research.33,34 The majority of our study participants reported trusting the information received from a physician and being confident with inhaler technique after watching structured videos by trained educators and professionals. Interestingly, distinguishing between the inhaler types did not show a significant improvement in either group, which may be because of the lack of sufficient explanation in the videos about the differences between inhalers and the purpose of their use.
To be successful, self-management does require a multifaceted approach that incorporates not only improving disease-related knowledge but also implementing strategies to empower patients to become informed individuals. Self-efficacy is a major predictor of being an informed individual to fully involve in self-care practices.37,43 In our study, we defined self-efficacy as patient’s self-reported beliefs about his/her capabilities to perform COPD management practices and we measured it using standard self-efficacy tool.37,43 Our findings showed considerable variation in self-efficacy subscales. All intervention groups were significantly improved in reported preparedness to “manage exacerbation” – a finding that aligns with previous research indicating that self-management training can result in reduced likelihood of exacerbation and improve health status.33,44 In addition, the effect of audiovisual interventions on patients’ confidence in managing exacerbations supports earlier research that shows improvements in patient self-management practices following video intervention.1,8,34,45 Despite this result, such significant improvements were not observed in other self-efficacy subscales among all intervention groups. For instance, none of the intervention groups had shown a significant improvement in “being informed” to self-manage their COPD. Although potential reasons for the difference in the result are unclear, one possible explanation might be because of the assumption that individual interpretation of “being informed” and “self-efficacy” may differ over time and between Chinese Mandarin and Cantonese patients.37,38 In addition, while the questions used to assess self-efficacy was validated in other studies with English-speaking patients,37,38,46 until now, there is no Chinese version of short COPD self-efficacy assessment in the literature. Therefore, our community facilitators translated the self-efficacy scales into Chinese-written formats. Although forward and backward translation was carried out to confirm accuracy, and translations were reviewed and commented by COPD patients during initial focus groups, having validated translated self-efficacy scales may have generated different results.46 In contrast, the heightened sense of “being able to achieve goals” found in participants who watched either clinician video (Group 1) or both videos (Group 3) may have been a consequence of the emphasis given on steps to achieve self-management goals in the clinician video, which possibly contributed to a greater sense of personal confidence in applying what they had learned into routine practice.47,48 The finding supports research which found that patients reported a significant improvement in self-management of chronic conditions after receiving instruction from clinicians or professionals, particularly in the video format.16,49
On measures related to PR, Groups 1 and 2 showed significantly higher improvement in “understanding PR procedures”; there were, however, no significant differences observed in other groups. The difference in improvements may be a function of the question used to measure this outcome. The questions for PR procedures consist of two sections: general descriptive information to test participants’ comprehension of the given information in the passage and questions to use numeracy skills to quantify hours, days, and procedures. Past studies have indicated that low numeracy influences a patient’s ability to understand and use health-related information to make informed medical decisions.50,51 Such numeracy issue might have influenced some patients, in particular older individuals, to respond incorrectly to the given PR procedure questions.
Patients who watched both lay and clinician videos (Group 3) showed an improvement only in some subscales with marginal statistical significance, indicating that no extra benefit was imparted by seeing both videos. One reason might be the combined length of two videos (32 minutes). Other studies have found that short educational videos, instructed by professionals, have better results on patient outcomes compared to longer videos.18,34 The small sample size of the study might also be another reason in observing the results that, although are statistically significant, may not be of practical importance. Larger sample size can produce meaningful results.
The greater frequency of a heightened impact with the clinician video (Group 1) may speak to community norms. In Asian culture, professionals – including physicians – hold a position of authority,17,18,23–25 and it may be that for some skills, participants paid greater attention to instructions from clinicians and felt more confident in applying the information received. However, the fact that Group 2 (lay video) emerged with the greatest improvement in some self-efficacy measures indicates that lay videos can also be effective.52 We found in our previous studies that information provided by community members (including patients) has a positive impact on patient’s understanding of disease management.17,18,23 Going forward, it will be important to gain a better understanding of whether certain types of information are better provided by clinicians and others by lay community members.
Secondary analyses revealed no statistically significant differences for any outcome across participants’ level of disease severity, indicating that length and severity of disease did not influence skill attainment. Larger sample sizes are likely needed to detect these differences. Differences between the sexes were identified in some aspects of COPD management, a finding that aligns with recent research into COPD self-management.53,54 Although males showed a greater improvement in the correct use of inhalers and the self-assessment of being able to remain calm during a worsening, females showed a greater improvement in their perceived ability to self-manage their condition. Based on the composition of our sample (71% male), however, these results may be limited in their meaning. Age proved a significant explanatory variable in only two instances. Older participants showed a significant improvement only in the ability to distinguish inhalers, which may be a consequence of having dealt with their condition for a longer period of time and having a greater overall awareness of COPD. Younger participants showed a significantly greater improvement in understanding the steps associated with PR, which may be a function of greater cognitive acuity and also better numeracy skills.55,56 Finally, as would be anticipated, participants with higher education showed a greater improvement in the domains where education proved significant (eg, correct use and understanding PR procedures). This finding aligns with other research that found patient education changed medication habits, improved inhaler compliance, and improved patient outcomes, compared with uneducated/low-educated patients.57,58
Limitations
This study was ambitious in its design and its use of three multidimensional outcome measures. The measure for self-efficacy, based on a short version of English scales, may have attempted to cover too broad a scope, making the inconsistent results harder to understand. Single-outcome definitions, more narrowly defined, may have provided more definitive results and direction for future research exploration. It should also be noted that reliance, for the most part, on self-reported assessments of skill levels leaves the results susceptible to response biases, such as social desirability bias. Finally, as indicated previously, the number of subjects is too small to make conclusive judgments on the intervention’s impact on self-management practices and more specifically outcomes such as exacerbations; larger studies are required to address this issue.
Conclusion
It is likely that self-management education in audiovisual format that is culturally and linguistically relevant was associated with an improvement in the proper use of inhalers with no indications for noticeable effects in other outcome parameters. This would in itself already be enough reason for recommending self-management education in COPD for Mandarin- and Cantonese-speaking patients. It is also essential to improve COPD patients’ confidence in their ability to follow physician instruction and self-management practices, for example, by augmenting self-efficacy. Self-efficacy plays a crucial factor in determining which activities or health behaviors a patient will perform or avoid. Because of study populations, follow-up time, and outcome measures, data are still insufficient to formulate clear recommendations regarding the form and contents of self-management education programs for Chinese COPD patients. There is an evident need for more large RCTs with a long-term follow-up, before more conclusions can be drawn.
Clinical implication
Our study shows that a simple culturally and linguistically appropriate disease management education intervention improved inhaler techniques and exacerbation management among Mandarin and Cantonese COPD patients. The findings indicate that rather than just improving patient knowledge on how to live with their disease, they should be taught to self-manage their chronic disease. We recommend that further research should be conducted with a larger sample size to assess the effectiveness of self-management education on behavioral change and patient empowerment. The investigations should focus on self-efficacy outcomes, as incorporating behavioral–clinical models for patient-centered care in COPD requires the use of tailored efficacy building strategies for self-management practices.
Acknowledgments
We thank the community members, facilitators, ethnocultural serving agencies, physicians, and key informants from the Mandarin and Cantonese communities in the Greater Vancouver Area who helped us with all aspects of this research. This project was funded by an operating grant from Canadian Institutes of Health Research (CIHR). The sponsor had no role in the design of the study, in the collection and analysis of the data, or in the preparation of the manuscript. The study was registered by the University of British Columbia Protocol Record Committee and the ClinicalTrials.gov Identifier is: NCT01474707.
Author contributions
All authors contributed to the design of the project. Mark FitzGerald and Iraj Poureslami undertook the review of the literature and prepared the initial draft of the article. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Cri Care Med. 2001;163:1256–1276. | ||
Buist AS, Vollmer WM, McBurnie MA. Worldwide burden of COPD in high- and low-income countries. Part I. The burden of obstructive lung disease (BOLD) initiative. Int J Tuberc Lung Dis. 2008;12:703–708. | ||
Chapman KR, Mannino DM, Soriano JB, et al. Epidemiology and costs of chronic obstructive pulmonary disease. Eur Respir J. 2006;27:188–207. | ||
Almagro P, Castro A. Helping COPD patients change health behavior in order to improve their quality of life. Int J Chron Obstruct Pulmon Dis. 2013;8:335–345. | ||
Effing TW, Bourbeau J, Vercoulen J, et al. Self-management programs for COPD: moving forward. Chronic Respir Dis. 2012;9:27–35. | ||
Worth H, Dhein Y. Does patient education modify behaviour in the management of COPD? Patient Educ Couns. 2004;52:267–270. | ||
Monninkhof E, van der Valk P, van der Palen J, van Herwaarden C, Partridge MR, Zielhuis G. Self-management education for patients with chronic obstructive pulmonary disease: a systematic review. Thorax. 2003;58:394–398. | ||
Effing T, Monninkhof EM, van der Valk P, et al. Self-management education for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2007;17:CD002990. | ||
Bourbeau J, Nault D, Dang-Tan T. Self-management and behaviour modification in COPD. Patient Educ Couns. 2004;52:271–277. | ||
Coulter A, Ellins J. Patient-focused Interventions: A Review of the Evidence. QQUIP and the Quality Enhancing Interventions Project. London, UK: The Health Foundation; 2006. Available from: http://www.health.org.uk/sites/health/files/PatientFocusedInterventions_ReviewOfTheEvidence.pdf. Accessed January 16, 2016. | ||
Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self-management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;19(3):CD002990. | ||
Harris M, Smith BJ, Veale A. Patient education programs: can they improve outcomes in COPD? Int J Chron Obstruct Pulmon Dis. 2008;3:109–112. | ||
Labrecque M, Rabhi K, Laurin C, et al. Can a self-management education program for patients with chronic obstructive pulmonary disease improve quality of life? Can Respi J. 2011;18:e77–e81. | ||
Taylor SJ, Candy B, Bryar RM, et al. Effectiveness of innovations in nurse led chronic disease management for patients with chronic obstructive pulmonary disease: systematic review of evidence. BMJ. 2005;331:335. | ||
Crow S, Ondrusek A. Video as a format in health information. Med Ref Serv Q. 2002;21:21–34. | ||
Rubens AJ. Interactive videodiscs: a new approach to healthcare education. Comput Healthc. 1992;13:42–46. | ||
Murphy D, Balka E, Poureslami I. Communicating health information: the community engagement model for video production. Can J Commun. 2007;32:121–134. | ||
Poureslami I, Nimmon L, Doyle-Waters M, et al. Effectiveness of video-based versus written educational interventions on asthma self-management and inhaler technique in Punjabi and Chinese asthma patients: a randomized controlled trial. J Asthma. 2012;49:542–551. | ||
Hill K, Goldstein RS, Guyatt GH, et al. Prevalence and underdiagnosis of chronic obstructive pulmonary disease among patients at risk in primary care. CMAJ. 2010;182:673–678. | ||
Tran N, Siu S, Iribarren C, et al. Ethnicity and risk of hospitalization for asthma and chronic obstructive pulmonary disease. Ann Epidemiol. 2011;21:615–622. | ||
Rodriguez-Rosin R, Anzueto A, Bourbeau JS, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Revised 2011. Global Initiative for Chronic Obstructive Lung Disease. Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2011_Feb21.pdf2011. Accessed December 18, 2015. | ||
Poureslami I, Nimmon L, Doyle-Waters M, FitzGerald JM. Using community-based participatory research (CBPR) with ethno-cultural groups as a tool to develop culturally and linguistically appropriate asthma educational materials. J Divers Health Care. 2012;8:203–215. | ||
Shum J, Poureslami I, Cheng N, FitzGerald JM. Responsibility for COPD self-management in ethno-cultural communities: the role of patient, family member, care provider, and system. Divers Equal Health Care. 2014;11:201–213. | ||
Poureslami I, Shum J, FitzGerald JM. Why do Chinese people with COPD continue smoking: the attitudes and beliefs of Chinese residents of Vancouver, Canada? Divers Equal Health Care. 2015;12:1–10. | ||
Poureslami I, Nimmon L, Doyle-Waters M, Shum J, FitzGerald JM. Hearing community voice: methodological issues in developing asthma self-management educational materials for immigrant communities. In: Agyemang C, Airhihenbuwa CO, de-Graft Aikins A, editors. Ethnicity: Theories, International Perspectives and Challenges. New York, NY: Nova Science Publishers, Inc.; 2013:59–84. | ||
BC Statistics. Population Estimates – Total Populations 2010. Victoria, BC: BC Statistics; 2010. Available from: http://www.bcstats.gov.bc.ca/StatisticsBySubject/Demography/PopulationEstimates.aspx. Accessed January 8, 2016. | ||
Statistics Canada. Ethnic diversity and immigration. 2011 National Household Survey. Statistics Canada. Available from: http://www.statcan.gc.ca/daily-quotidien/130508/dq130508b-eng.pdf 2013. Accessed December 17, 2015. | ||
Dumville JC, Hahn S, Miles JN, Torgerson DJ. The use of unequal randomization ratios in clinical trials: a review. Contemp Clin Trials. 2006;27:1–12. | ||
Schulz KF, Grimes DA. Unequal group sizes in randomised trials: guarding against guessing. Lancet. 2002;359:966–970. | ||
Bates RA. Popular theater: a useful process for adult educators. Adult Educ Q. 1996;46:224–236. | ||
Conrad D. Exploring risky youth experiences: popular theatre as a participatory, performative research method. Int J Qual Method. 2004;3:1–24. | ||
Wang LW, Miller MJ, Schmitt MR, Wen FK. Assessing readability formula differences with written health information materials: application, results, and recommendations. Res Social Adm Pharm. 2013;9:503–516. | ||
Rootmensen GN, van Keimpema N, Jansen HM, de Haan RJ. Predictors of incorrect inhalation technique in patients with asthma or COPD: a study using a validated videotaped scoring method. J Aerosol Med Pulm Drug Deliv. 2010;23:323–328. | ||
Verver S, Poelman M, Bogels A, Chisholm SL, Dekker FW. Effects of instruction by practice assistants on inhaler technique and respiratory symptoms of patients. A controlled randomized videotaped intervention study. Fam Pract. 1996;13:35–40. | ||
Batterink J, Dahri K, Aulakh A, Rempel C. Evaluation of the use of inhaled medications by hospital in-patients with chronic obstructive pulmonary disease. Can J Hosp Pharm. 2012;65:111–118. | ||
Xu P. Using teach-back for patient education and self-management. Am Nurs Today. 2012;7:1–9. | ||
Zhang C, Wang W, Li J, et al. Development and validation of a COPD self-management scale. Respir Care. 2013;58(11):1931–1936. | ||
Huanhuan Hu, Gang Li, Takashi Arao. Validation of a Chinese version of the self-efficacy for managing chronic disease 6-Item scale in patients with Hypertension in Primary Care. ISRN Public Health. 2013;2013:1–6. | ||
O’Donnell DE, Aaron S, Bourbeau J, et al. State of the Art Compendium: Canadian Thoracic Society recommendations for the management of chronic obstructive pulmonary disease. Cann Respir J. 2004;11:7B–59B. | ||
White R, Walker P, Roberts S, Kalisky S, White P. Bristol COPD Knowledge Questionnaire (BCKQ): testing what we teach patients about COPD. Chron Respir Dis. 2006;3:123–131. | ||
Fang X, Wang X, Bai C. COPD in China: the burden and importance of proper management. Chest. 2011;139:920–929. | ||
Statistical analysis system. SAS Guidelines-Editorial Guidelines. Cary, NC: SAS Institute Inc.; 2015. Available from: http://www.sas.com/en_us/legal/editorial-guidelines.html. Accessed Noverber 20, 2015. | ||
Wigal JK, Creer TL, Kotses H. The COPD self-efficacy scale. Chest. 1991;99:1193–1196. | ||
FitzGerald JM, Haddon J, Bradley-Kennedy C, Kuramoto L, Ford GT. Resource use study in COPD (RUSIC): a prospective study to quantify the effects of COPD exacerbations on health care resource use among COPD patients. Can Respir J. 2007;14:145–152. | ||
Liu F, Cai F, Tang Q, et al. Effects of an animated diagram and video-based online breathing program for dyspnea in patients with stable COPD. Patient Prefer Adherence. 2013;7:905–913. | ||
Garrod R, Marshall J, Jones F. Self-efficacy measurement and goal attainment after pulmonary rehabilitation. Int J Chron Obstruct Pulmon Dis. 2008;3:791–796. | ||
Bourbeau J, Julien M, Maltais F, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med. 2003;163:585–591. | ||
Fan VS, Gaziano JM, Lew R, et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med. 2012;156:673–683. | ||
Saleh S, Larsen JP, Bergsåker-Aspøy J, Grundt H. Re-admissions to hospital and patient satisfaction among patients with chronic obstructive pulmonary disease after telemedicine video consultation – a retrospective pilot study. Multidiscip Respir Med. 2014;9:6–16. | ||
Reyna VF, Nelson WL, Han PK, Dieckmann NF. How numeracy influences risk comprehension and medical decision making. Psychol Bull. 2009;135:943–973. | ||
Lag T, Bauger L, Lindberg M, Friborg O. The role of numeracy and intelligence in health-risk estimation and medical data interpretation. J Behav Decis Making. 2014;27:95–108. | ||
McCabe C, Dinsmore J, Brady AM, Mckee G, O’Donnell S, Prendergast D. Using action research and peer perspectives to develop technology that facilitates behavioral change and self-management in COPD. Int J Telemed Appl. 2014;2014:380919. | ||
Watson L, Vestbo J, Postma DS, et al. Gender differences in the management and experience of Chronic Obstructive Pulmonary Disease. Resp Med. 2004;98:1207–1213. | ||
Han MK, Postma D, Mannino DM, et al. Gender and chronic obstructive pulmonary disease: why it matters. Am J Respir Crit Care Med. 2007; 176:1179–1184. | ||
Yohannes AM. Cognitive impairment and risk for disability in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2014;11:1445–1446. | ||
Cleland JA, Lee AJ, Hall S. Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Fam Pract. 2007;24:217–223. | ||
Williams MV, Baker DW, Honig EG, Lee TD, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–1015. | ||
Kiser K, Jonas D, Warner Z, Scanlon K, Bryant Shilliday B, DeWalt DA. A randomized controlled trial of a literacy-sensitive self-management intervention for chronic obstructive pulmonary disease patients. J Gen Intern Med. 2012;27:190–195. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.