Back to Journals » Patient Preference and Adherence » Volume 15
Antihypertensive Medication Adherence and Associated Factors: A Cross-Sectional Analysis of Patients Attending a National Referral Hospital in Asmara, Eritrea
Authors Mebrahtu G, M Moleki M, Okoth Achila O , Seyoum Y, Adnoy ET, Ovberedjo M
Received 7 June 2021
Accepted for publication 28 October 2021
Published 23 November 2021 Volume 2021:15 Pages 2619—2632
DOI https://doi.org/10.2147/PPA.S319987
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Johnny Chen
Goitom Mebrahtu,1 Mary M Moleki,2 Oliver Okoth Achila,3 Yemane Seyoum,4 Elias T Adnoy,5 Martin Ovberedjo6
1Division of Clinical Services, Ministry of Health, Asmara, Eritrea; 2Department of Health Studies, University of South Africa (UNISA), Pretoria, South Africa; 3Department of Clinical Laboratory Services, Orotta School of Medicine and Health Sciences, Asmara, Eritrea; 4Department of Internal Medicine, Orotta School of Medicine and Health Sciences, Asmara, Eritrea; 5Public Health Unit, Orotta School of Medicine and Health Science, Asmara, Eritrea; 6Eritrea Country Office, World Health Organisation (WHO), Asmara, Eritrea
Correspondence: Oliver Okoth Achila Email [email protected]
Background: Recent research suggests that poor adherence to antihypertensive medication (AHM) is a major problem in the management of hypertension. This study was therefore designed to evaluate the frequency of AHM and associated risk factors in patients attending a national referral hospital in Asmara, Eritrea.
Methods: A total of 335 respondents (females: 222 (66.3%) participated in this cross-sectional study. Adherence to Medication was evaluated using a modified version of the Medication Adherence Report Scale (MARS). Additional data were abstracted from patients’ medical records and a WHO STEPwise questionnaire.
Results: The mean (±SD) age of the study participants was 59.65 (± 12.20) years (females: 56.82 (± 9.95) vs males: 57.17 (± 9.60) years, p-value=0.001). Similarly, the median (IQR) for diastolic blood pressure (DBP) and systolic blood pressure (SBP) were 85.00 mmHg (IQR: 80.00– 90.00 mmHg) and 145.00 mmHg (IQR: 130.00– 160.00 mmHg), respectively. Overall, 246 (73.4%) and 244 (72.8%) participants had poor knowledge and poor adherence to AHM, respectively. In the multivariate analysis, factors associated with increased odds of poor adherence to AHM included sex (females: adjusted odds ratio (aOR): 4.95; 95% CI: 1.52– 16.11, p value=0.008); employment status (Ref: employed/NGO) (self-employed: aOR: 1.95; 95% CI: 0.45– 8.48, p-value=0.373) (housewife: aOR: 0.13; 95% CI: 0.04– 0.413, p-value=0.001) (unemployed: aOR: 1.38; 95% CI:0.32– 5.98; p-value=0.670); lack of attendance of health talk at the clinic (aOR: 2.33; 95% CI: 1.17– 4.63; p-value=0.016); high cost of transportation (yes: aOR: 6.87; 95% CI: 3.25– 14.52; p-value< 0.001); knowledge (poor: aOR: 6.23; 95% CI: 2.36– 18.05, p-value< 0.001) and hypertension stage (Stage 3: aOR: 5.55; 95% CI, 1.44– 21.37, p-value=0.013). Low level of knowledge regarding hypertension-related complications or associated risk factors was also noted.
Conclusion: The high level of poor adherence to anti-hypertension medications and low level of knowledge on hypertension should raise concern. Overall, decentralization of health care services and educational support are vital intervention pathways in this population.
Keywords: Eritrea, knowledge, hypertension, medication adherence
Background
Hypertension (HTN) (Systolic blood pressure (SBP) ≥140 millimeters of mercury (mmHg) and/or Diastolic blood pressure (DBP) ≥90 mmHg) is a global public health problem. A recent Bayesian hierarchical modeling study - the NCD Risk Factor Collaboration (NCD-RisC) study group in 2015; reported that the global age-standardized prevalence of hypertension was 24.1% (95% CI: 21.4–27.1) in men and 20.1 (95% CI: 17.8–22.5) in women.1 Reports on trends have also noted a sharp uptick in the incidence; hence, the prevalence of hypertension in low- and middle-income countries (LMICs) in East and South Asia, Oceania, and sub-Saharan Africa (SSA).1 Corroborating these reports, a relatively recent systematic analysis of the frequency of hypertension in SSA estimated that the overall pooled prevalence of hypertension was about 54.6 million (19.7%) in 1990, 92.3 million (27.4%) in 2000, and 130.2 million in 2010 (33.7%).2 The reports of a rapid, continent-wide, epidemiological transition (shift from infectious diseases to non-infectious diseases (NCDs)) in SSA are well documented3,4 and this informs the current posture on hypertension in the continent.
The observed increase in the prevalence of hypertension has been linked to multiple drivers including population growth, increasing life expectancy (longevity), rural–urban migration, and rapid urbanization, among others. Attention to the rapidly evolving epidemic of hypertension and its implications for health systems in SSA was previously highlighted by two large-scale epidemiological studies (The INTERHEART and INTERSTROKE). In their submission, the investigators noted that hypertension is part of a cluster of modifiable risk factors that account for multiple composite events in cardiovascular clinics (acute myocardial infarction (MI), stroke, heart failure, end-stage kidney disease (ESKD), among others).5,6 The high frequency of hypertension-related complications was attributed to the high number of patients with poorly controlled hypertension. Interestingly, poorly controlled hypertension in SSA has been linked to multiple barriers existing at government/health-system, health care provider, and patient levels.7,8
Despite the large body of data showing that hypertension is major public health concern in SSA, cost-analysis demonstrates that most countries in the region have scant resources for acute care and rehabilitation, hence cannot offer the same quality of care and treatment as high-income countries (HIC).4 The crisis is amplified by several patient-related factors – health literacy, and poor adherence.9 Regarding the latter, studies of dosing histories of patients with chronic diseases have repeatedly demonstrated that drug utilization is frequently irregular – spanning a wide spectrum of deviations – and is skewed heavily towards under-dosing. More importantly, research on pharmacy-led interventions have demonstrated that besides physician inertia and deficiencies of health care systems, undiagnosed or undeclared non-adherence/or poor adherence to anti-hypertensive medications (AHM) (particularly multiple or sequential omissions) is associated with adverse cardiovascular (CVD) events or other hard endpoints6,9–11 such as cerebrovascular accidents, myocardial infarction (MI), end-stage renal disease (ESRD), among others.11 Moreover, it has the potential to influence BP variability, particularly visit-to-visit indices, trigger hazardous rebound or recurrent first-dose effects, promote pseudo-resistance or frank resistance, trigger inappropriate escalation of treatment and excess use of healthcare system resources.11 For resource-poor countries in SSA, the excess costs incurred by states due to poor adherence to AHM can have anegative impact on healthcare expenditure. On the whole, these findings have largely strengthened adated (2003) WHO assertion that increasing the effectiveness of interventions targeting adherence to treatment may have agreater impact on outcome than any improvement in specific medical treatments.10
Although the importance of adherence to pharmacological and non-pharmacological interventions for hypertension is well documented; reports have noted a glaring discrepancy between the well-documented importance of adherence to medications and the limited focus on the domain in clinical research and practice. Instructively, limited literature exists on adherence to AHM and associated factors among patients with hypertension in SSA. The lack of literature is particularly acute in Eritrea – we could not locate any publication (in any language) on this subject in international or local repositories. On a more general ground, a comprehensive understanding of modifiable factors associated with poor adherence to AHM in settings across SSA can guide the development of interventions that may ultimately improve overall outcome. In turn, this has the potential to reduce the economic burden of hypertension particularly in resource-poor regions where accessibility to AHM and delivery of health care services is largely suboptimal. This study was therefore designed to evaluate the level of AHM adherence and associated factors in hypertensive patients attending the largest follow-up facility in Eritrea. Hypertension-related knowledge was also investigated.
Participants and Methods
Study Design, Background and Setting
This cross-sectional study was conducted at the Halibet Referral Hospital in Asmara, Eritrea. The hospital is located in the Zoba-Maekel region – one of the geopolitical zones in the country. Established in 1992 as a regional referral hospital, the facility was upgraded to tertiary-level facility in 2010 – national referral hospital. The decision to domicile this study at the Halibet National Referral hospital was informed by multiple considerations. Foremost was the fact that Eritrea has a highly centralized health system. The system has three tiers (primary level – health centers and health stations, secondary level – zonal and sub-zonal hospitals, and tertiary level – regional and national referral hospitals). Private sector involvement is marginal – limited (severely) to specific services, eg, dental care and pharmacy. More importantly, the treatment and management of chronic diseases is centered in specific facilities. For example, in Asmara, the capital City of Eritrea, a majority of patients with hypertension are referred for enrolment at Halibet Referral Hospital (2673 enrollees in 2016). However, a small proportion of patients are enrolled at Haz-Haz hospital.
Sample Size Estimation and Participant’s Recruitment
The single proportion formula was used to estimate sample size (N). The frequency of poor adherence was set at 64.4% per the recent findings from a cross-sectional study from 12 SSA countries.12 Additional standard inputs included a margin error of 5%, and 95% confidence interval (CI). After adjustments, we generated a minimum sample size of 341. To recruit participants, out patient’s attending the hypertension care clinic within a pre-set period of time (August – December 2019) were recruited. Consideration for inclusion included history of hypertension, ability to grant written consent, age ≥20 years, and patients who had been on medication for a period ≥12 months. Exclusion was based on the following criteria: pregnancy, inpatients or severe illness, and inability to grant consent.
Data Collection
Data on demographic characteristics, lifestyle factors, knowledge, and adherence were collected using standard instruments – WHO Stepwise Questionnaire.13 Alcohol consumption and tobacco/cigarette smoking were defined as follows: smokers were categorized as (a) non-smokers (individuals with no history of smoking (b) smokers (current use of at least one cigarette a day). Alcohol consumption was defined as self-reported consumption of any alcoholic brew, at least twice weekly. Data collection was conducted by the authors and trained research assistants. Blood pressure was measured with an Omron electronic BP machine, after at least 10 minutes rest, in the dominant arm of seated patients on three occasions at an interval of 1 minute. The average of the last two readings was recorded for both systolic BP (SBP) and diastolic BP (DBP). To ensure quality, completed questionnaires were carefully checked by quality supervisors after the interviews each day. Additional information (comorbidities among others) was abstracted from outpatient department (OPD) medical records.
Adherence and Perceived Knowledge
A validated self-report questionnaire (a modified version of the Medication Adherence Rating Scale (MARS)) originally developed by Thompson et al14 was used to evaluate adherence (see Table 1). Cronbach’s alpha measurement of internal consistency for the questions in this rating scale was >7.5. The 10-item MARS questionnaire requires Yes/No responses and incorporates a range of questions on behavior and attitude towards medication. The modified MARS scale was interpreted as follows: correct answers include “NO” to questions 1–10. Participants providing correct answers to 8 out of the 10 questions were considered to be adherent. Knowledge about high BP, complications, benefits of treatments, risk factors were assessed using a modified 14-point – WHO stepwise questionnaire.13 Accordingly, the scores were as follows: correct=1 and incorrect = 0. The scoring range of the questionnaire was 0 (minimum) - 14 (maximum). A cut-off level of <10 correct answers was considered as poor knowledge about hypertension.
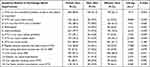 |
Table 1 Knowledge About Hypertension (n=335) |
Definitions
Body mass index (BMI) stratifications were as follows: underweight = BMI ≤ 18:5 kg/m2; normal weight = BMI: 18.6–24.9 kg/m2; overweight = BMI: 25–29.9 kg/m2; obese ≥30 kg/m2. The International Diabetes Federation (IDF) specifications were used to stratify abdominal obesity: waist circumference (WC) >94 cm in males and WC >80 cm in females. The European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension guidelines was used to define uncontrolled hypertension: <60 years old – SBP ≥140 mmHg and/or a DBP ≥90 mmHg; >60 years old – <150/90 mmHg.7,15 Accordingly, hypertension was graded as follows: Grade 1 hypertension (SBP 140 −159 mmHg and/or DBP 90–99 mmHg); Grade 2 hypertension (DBP 160−179 mmHg and/or DBP 100–109 mmHg); and Grade 3 hypertension (severe) (SBP ≥180 mmHg and/or DBP ≥110 mmHg).7
Data Analysis
The data were analysed using Statistical Package for Social Sciences (SPSS Inc.) (Version 20.0; IBM, Chicago, IL, USA). Data normality was evaluated using Shapiro–Wilk or Kolmogorov–Smirnov tests. Depending on data distribution, mean ± standard deviation (SD) or median ± interquartile range (IQR) were computed for selected continuous variables. Relevant comparisons of differences in mean or median values were evaluated using appropriate parametric and nonparametric statistics. The relationship between specific categorical variables was tested using Chi-square (χ2) test/or Fischer’s exact test. A separate logistic regression model was fitted for medication adherence. To ensure the robustness of the regression models, we checked for the absence of multicollinearity. Crude and adjusted odds ratios (OR) and 95% confidence interval (CI) were subsequently reported. All p-values were 2-sided, and statistical significance was set at <0.05. Missing values or refusals to answer questions were handled by exclusion from analysis. Tables were used to report the data.
Ethical Approval and Consent to Participate
Ethical approval for the study was obtained from the Eritrean Ministry of Health (MOH) research ethics committee. In addition, requisite permission was obtained from the hospitals’ director and local administration. Participants were recruited voluntarily after signing a consent form. This was only undertaken after the participants were provided with information on the study objective, study procedures, possible adverse effects, and the right to refuse or terminate their participation in the study at any time/stage. Information on the maintenance of data confidentiality and integrity was also provided. To ensure data confidentiality and privacy, personal identifiers such as names were not collected. Finally, all the procedures were conducted as per the Declaration of Helsinki.
Result
Characteristics of Patients
A total of 335 respondents participated in this study. Of these, 222 (66.3%) were females; 102 (30.4%) had no formal education; 140 (41.8%) had primary-level education; 93 (27.8%) secondary level and above. Additionally, 149 (44.5%) indicated that they were separated, divorced, widowed or never married. In terms of employment, 41 (12.2%) were unemployed; 122 (36.4%) were employed (either by the government or an NGO); 31 (9.3%) were self-employed, and 141 (42.1%) were housewives. Further, 94 (41.6%) were on 1 AHM and 94 (28.1) presented with hypertension-related complication. The mean (±SD) age of the study participants was 59.65 (± 12.20) years (females: 56.82 (±9.95) vs males: 57.17 (±9.60) kg/m2, p value = 0.001). The averages (±SD) for BMI and waist circumference (WC) were 25.31 (±4.10) kg/m2 (females: 25.71 (±4.42) vs males: 24.70 (±3.6) kg/m2, p value = 0.117) and 90.43 (±14.49) cm (females: 88.83 (±10.37) vs males: 91.81 (±17.67) kg/m2, p value = 0.321), respectively. Similarly, the median (IQR) for DBP and SBP were 85.00 mmHg (IQR: 80.00–90.00 mmHg) and 145.00 mmHg (IQR: 130.00–160.00 mmHg), respectively. In terms of hypertension grades: 143 (42.7) had Grade 1 hypertension; 83 (24.8%) had Grade 2 hypertension and 33 (9.9%) Grade 3 hypertension. Overall, 76 (22.7%) had well-controlled hypertension. Lastly, 9 (2.7%) of the study participants indicated that they have consulted a traditional healer over their condition and 4 (1.2%) noted that they were currently taking herbal or traditional remedies for raised BP. See Table 2 for additional information.
 |
Table 2 Patients Characteristics |
Knowledge About Hypertension
We evaluated knowledge regarding hypertension and associated risk factors. The results were pooled and subsequently stratified with respect to gender. According to our computations 246 (73.4%) of the respondents had poor knowledge. Importantly, 287 (84.8%) of respondents demonstrated awareness of the fact that hypertension can be controlled by adherence to treatment. The items most often answered incorrectly were the following (in order of decreasing frequency): association between hypertension and retinopathy, 132 (39.4%); kidney problems, 131 (39.1%); and heart attack, 122 (36.4%), respectively. The number of participants who noted that heavy alcohol consumption, obesity, cigarette smoking, and salty food; can cause hypertension were 118 (35.3%), 100 (29.9%), 96 (28.7%), 92 (27.5%), respectively. Finally, only 110 (32.8%) noted that regular exercise may help control hypertension. Significant differences were observed in several items between males and females. See Table 1.
Adherence to Medication
Medication adherence was evaluated using a modified version of MARS – reliability assessment for the subscales used demonstrated good reliability. Table 3 summarizes the obtained result. Accordingly, 244 (72.8%) had poor adherence to AHM. The median (IQR) age for poor adherers was significantly lower (58.75 years: IQR [49.0–68.0 years]) vs (64.0 years: IQR [53.00–74 years]), p-value = 0.026. Further, the median DBP and SBP were higher for poor adherers (85.00 mmHg: IQR [80.0–90.0 mmHg]) vs (80.00 mmHg: IQR [80.0–90.0 mmHg]), p value = 0.034; and (150 mmHg: IQR [140–160 mmHg]) vs (140 mmHg: IQR [130–160 mmHg]), p-value= 0.004, respectively. By absolute percentages, 187 (55.83%), 155 (45.9%) and 186 (55.5) affirmed that forgetfulness, carelessness and stopping medication when symptoms were under control was an issue. A large number of participants, 174 (51.9%) also noted that the fear of side effects was a concern.
 |
Table 3 Responses to MARS Scale Questions |
Adherence and Associated Factors
Bivariate analyses of the relationship between specific factors and medication adherence are shown in Table 4. In this analysis, sex, age, educational status, employment status, duration of hypertension, attendance of health talk at the clinic, serious hypertension complication (stroke), knowledge, and BP control. Further, multivariate logistic regression (Backward: conditional) was employed to identify factors that were associated with poor adherence. In this model, Hosmer–Lemeshow test for the final iteration demonstrated a good fit to the data (P-value = 0.532).
 |
Table 4 Factors Associated with Adherence to Antihypertensive Medications (N=335) |
Overall, we demonstrated that increased likelihood of poor adherence to AHM was independently associated with sex (Ref: female) (males: adjusted odds ratio (aOR): 4.95; 95% CI: 1.52–16.11, p-value=0.008); employment status (Ref: employed/NGO) (self-employed: aOR: 1.95; 95% CI: 0.45–8.48, p-value=0.373) (housewife: aOR: 0.13; 95% CI: 0.04–0.413, p-value=0.001) (unemployed: aOR: 1.38; 95% CI:0.32–5.98; p-value= 0.670); attendance of health talk at the clinic (no: aOR: 2.33; 95% CI: 1.17–4.63; p-value=0.016); cost of transportation is high (yes: aOR: 6.87; 95% CI: 3.25–14.52; p-value<0.001); knowledge (poor: aOR: 6.23; 95% CI: 2.36–18.05, p value <0.001) and classes of raised BP (hypertension stage 3: aOR: 5.55 (1.44–21.37), p-value = 0.013.
Discussion
Hypertension is currently ranked as a leading cause of morbidity and mortality in SSA.1 This notwithstanding, public health responses to the epidemic are largely suboptimal.7,9 Many governments across the region are lagging in the implementation of population-wide high blood pressure (BP) awareness and control programs even to high-risk groups.7,9,16 Recent information from Eritrea, for example, demonstrates a growing burden of hypertension; high frequency of hypertension-related complications; low level of awareness; and severely limited research activity on multiple aspects of hypertension.17 In this study, we restricted our analysis to poor adherence to AHM.
On the whole, the mean age (±SD) of the study participants was high 59.65 (± 12.20) years with a small, albeit significant (p-value = 0.001) variation in the age gap between the sexes (females: 56.82 (±9.95) vs males: 57.17 (±9.60) kg/m2). Comparable results of age profiles were recently reported in a multi-country investigation of adherence in the region (females: 57.7 (± 12.0) years’ vs males: 59.2 (± 11.4) years for men).18 Unlike other jurisdictions in SSA (12; 19), the use of traditional or herbal medicines for management of BP was minimal 9 (2.7%) and only 4 (1.2%) indicated that they were currently taking herbal medicines. Therefore, the need to involve traditional healers or herbalists on this issue is not an urgent imperative. Further, we noted that a relatively large number of patients had uncontrolled BP 259 (77.3%). In the Macquart de Terline et al study,18 77.4% of the study participants had uncontrolled BP. In a study conducted in Ghana and Nigeria, poor BP control was noted in 69.7% of the study participants.20
The large number of patients with poor adherence to treatment 244 (72.8%) was another striking discovery. Compared to multiple studies in the region, our findings are on the high end of the spectrum. In a recent systematic review, the authors uncovered a wide variation in adherence to AHM in SSA – Ethiopia 35.4% to Ghana 93.3%.21 Other investigators have reported equally high numbers: 64% in Addis Ethiopia22; 69.7% in a multi-country (Nigeria and Ghana) study.20 In general, emerging data from SSA paints a highly complex and dynamic picture with significant variation between and within countries in SSA.18,20–26 Others have described significant regional disparities – 62.4% (African patients); 43.5% (Asian patients) and 36.6% (American patients).27
Methodological differences (heterogeneity of methods and definitional breakpoints) may partially account for the observed variation.27 For example, some investigators have noted that some studies from SSA, which utilized the Morisky Medication- Adherence Scale (MMAS-8) reported relatively high percentages of poor adherence 92.5% in Nigeria and 93.3% in Ghana.19,20 By and large, these comments highlight a widely held notion that the performance of self-report questionnaires or scales is rather circumscribed. For this reason, the use of more sophisticated and expensive approaches such as biochemical analysis based on high-performance liquid chromatography-tandem mass spectrometry (LC-MS/MS) is projected to grow.
As expected, we observed a strong association between BP control and adherence. In addition, a significant relationship (p-value=0.006) between poor adherence and uncontrolled hypertension was observed. In addition, a relationship between stage of hypertension and poor adherence was also noted with stage 3 showing the strongest relationship in the multivariate analysis (5.55[95% CI: 1.44–21.37]). These findings are largely in keeping with recent reports from the region. In their analysis, Marquart de Terline et al noted that hypertension Grades 1–3 were associated with a 1.52-fold, 1.8-fold and 3.08-fold increased likelihood of poor adherence, respectively.12 There are multiple ways to interpret the observed result. First, poor adherence to ADH can be the cause of high BP. Another reasonable speculation is that clinicians often respond to extremely high BP (SBP ≥ 180 mmHg and/or DBP ≥ 110 mmHg) by increasing the number of prescribed AHM (according the 8th Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC-8) guidelines, patients whose SBP/DBP is >20/10 mmHg above target can start their treatment on a combination of two drugs – two classes of medications). Dose escalation, can, in turn, increase the likelihood of maladherence. Indeed, some studies suggest that a unit increase in the number of prescribed AHM increases the likelihood of maladherence by ~80%.28
On components of adherence using MARS questionnaire, we demonstrated that forgetfulness; stopping medication when one feels better; stopping medication when one feels worse after taking medication; and stopping medication without informing the doctor were key drivers of maladherence. On the whole, these findings complement previous reports that suggested that forgetfulness is one of the most important drivers of maladherence in most patients.25,29 Admittedly, forgetfulness is a descriptor with multiple meanings. It can be unintentional non-adherence (a type of non-adherence that may be influenced by beliefs or with factors such as cognitive decline) or intentional forgetting.10,11,26 Unfortunately, an in-depth exploration of the nature of forgetting was not undertaken. Further, the propensity to stop medication in the absence of symptoms is well documented. For example, a study conducted in Palestine30 reported that approximately one-third of patients stopped taking drugs after feeling better, 3 months after beginning treatment. Apart from emerging technological interventions such as electronic pill monitors, electronic reminders – mobile phone apps; automated short messaging services (SMS), a commonly prescribed intervention to forgetfulness or unhealthy dispositions (eg the tendency to stop medication when one feels better) is adherence counseling and family support (particularly in elderly patients with cognitive decline). However, disappointing data indicate that the simultaneous presence of family support and poor adherence was relatively common in this setting. This can only lead us to question the quality of support provided by family members. Unfortunately, an in-depth analysis of the nature of support was not attempted.
In a separate analysis, we evaluated factors associated with poor adherence. On the whole, published literature has documented multiple determinants of poor adherence to long-term therapies. In a dated 2003 report, WHO highlighted five interacting dimensions that can influence the adherence process (eg, from initiation, implementation to persistence).10 Components of the schema included patients understanding and perception; patient-related factors; disease-related factors; socio-economic factors; health system influences; and therapy-related factors. We believe that this multidimensional model offers a good framework for discussion of additional results.
Among demographic factors, sex, age groups, education, employment status, duration of hypertension were associated with poor adherence in the cross-tabulation procedure. Regarding sex, we have to note that the results are high variables in most studies.11 However, and similar to this study, the evidence demonstrates that women tend to be more adherent. For example, a systematic meta-analysis of 28 studies from Europe and a retrospective HPLC-MS/MS)-based study in the UK and Czech reported a higher likelihood of non-adherence in males.21,28 These results are largely in keeping with our findings which demonstrated a higher likelihood of poor adherence in males (4.95: 95% CI: 1.52–16.11). In contrast, a study in Nigeria and Ghana reported a null relationship.20
Concerning the impact of age, our study demonstrated an inverse relationship between age and poor adherence. However, the association was attenuated in the multivariate analysis. The relationship observed in this study is not novel and has been uncovered by other investigators. For example, the previously highlighted HPLC-MS/MS-based study in the UK and Czech reported a > 30% attenuation in odds of poor adherence per 10-year increase in age.28 The observed difference has been linked to disparate somatic, psychosocial, and behavioral influences between the sexes. Altogether, experts agree that the relationship between sex, age and adherence is inconsistent.11 Moreover, some authors have noted that the non-modifiable nature of these variables has undermined research interest in recent years.11
Further, our study demonstrated a relationship between level of education and poor adherence – individuals with ≥ secondary education recorded the poorest results (80%). In most part, this finding is counterintuitive. Conventional wisdom suggests that higher level of education can lead to a better appreciation of the risks associated with non-compliant behavior. This proposition was prominently endorsed in a study conducted in Ethiopia.22 Consistent with our findings, a study from West Africa indicated that educated patients were less-adherent to treatment.28 A plausible explanation of this outcome may involve a higher incidence of self-medication among the better-educated participant. We evaluated this possibility and established that this was indeed the case. A plausible explanation of this phenomenon is the possibility that unlettered patients are more likely to comply with the directives from health professionals. Compliant behavior may also explain the finding associating women with a higher likelihood of medication adherence. Interestingly, we uncovered a strong relationship between employment status and poor adherence – adherence was higher in housewives. A separate analysis found an association between educational level and employment status, and demonstrated that most housewives had no formal education.
Among socio-economic factors, current literature suggests that cost of treatment or limited access to care-providers can compromise adherence. According to most experts in SSA, lack of health insurance; exorbitant co-payments or out-of-pocket payments spent on AHMs; drug stock outs, and limited social resources, among others, can constrain adherence.7,11,31 In our study, the potential influence of some of these factors was detected: high cost of transport to the hospital was associated with a 6.87 (95% CI: 3.25–14.52) likelihood of poor adherence, p < 0.001). Furthermore, high cost of drugs was also linked to poor adherence. Multiple factors, unique to Eritrea, may be invoked to explain the observed relationship. Foremost is the fact that Eritrea has a highly centralized health system with extremely marginal private sector involvement. Under this system, select government-funded facilities offer the necessary care services to hypertensive patients at subsidized costs. Predictably, some patients may incur high transport costs to the follow-up facilities and the out-of-pocket costs can also be burdensome to some patients.
Another significant finding in our study was the connection between the belief that complication of hypertension are dangerous and poor adherence. This finding adds credence to the presumption that the perceived seriousness of a chronic condition (eg, hypertension) may increase adherence. This presumption is a cornerstone of the health belief model (HBM). However, one unexpected finding in adherence literature is that life-threatening diseases do not, ipso facto, prompt strict adherence to prescribed regimen(s)32 – even patients on cancer chemotherapy are known to skip doses.33 In our study, participants with documented incidences of serious hypertension-related complications had poor adherence, p-value <0.001. Much of this outcome can be explained by reference to the fact that the intensity and complexity of treatment typically required for patients with multiple chronic complications might require polypharmacy and multiple daily dosing – this may reduce compliance.23 Overall, the possibility that patience’s with serious hypertension-related complications (stroke, MI, kidney problems) are registering poor adherence is concerning.
Last but not least, studies have demonstrated the importance of patient’s knowledge about multiple aspects of hypertension. To illustrate, cross-sectional studies conducted in Ethiopia and Congo reported that lack of knowledge about hypertension was significantly associated with non-adherence.23,30,31,34–35 Our study supports these findings by showing that patients with poor knowledge had a higher likelihood of poor adherence, 6.23 (95% CI: 2.36–18.05). Separately, poor knowledge was reflected in the high proportion of participants with insufficient knowledge on the connection between hypertension and multiple complications (heart problems, retinopathy, and nephropathy) and/or risk factors (high salt consumption; obesity, cigarette smoking, and insufficient exercise). The basic connection between poor knowledge and non-adherence was further demonstrated by the data showing that lack of participation in the clinics’ health information sessions was associated with poor adherence, 2.33 (95% CI: 1.17–4.63). On the whole, evidence suggests that the most effective modality for improving health literacy is formal educational interventions provided by clinicians or other healthcare providers.15 On the basis of this, our data support the fact that provision of knowledge represents a major pathway of intervention in this population.
Limitation of the Study
This study, the first of its kind in Eritrea, adopted a cross-sectional design to recruit hypertensive patients in the largest hypertension follow-up facility in Asmara, Eritrea. However, the study had several limitations. First is the use of a self-reported questionnaire to assess adherence or knowledge levels. In general, reports indicate that these questionnaires may overestimate adherence. In addition, self-reported questionnaires may suffer from recall and social desirability biases. Nonetheless, we have to emphasize that self-reported questionnaires are generally simple, cost-effect, and can be implemented easily in clinical workflows. They are also useful in the assessment of barriers. As a consequence, they have real utility in resource-poor settings. Importantly, the use of sophisticated technologies such as HPLC-MS/MS in adherence studies is impractical in most jurisdictions in SSA. Second, a cross-sectional design was employed in this study. Therefore, the inability to dissect causality is a major limitation. Consequently, longitudinal studies with a long follow-up duration are needed. Such studies can also incorporate more objective methods of measuring adherence. In addition, an expanded range of variables can be incorporated in such studies.
Conclusions
Hypertension in SSA was recently described as a massive and increasing health disaster awaiting solution. Non-adherence to AHM, a detectable and manageable condition/problem, is currently regarded as one of the most important problem in the unfolding crisis. In general, experts agree that the multidimensional nature of the barriers associated with poor adherence augments the challenge. In this study, we noted a relatively high prevalence of poor adherence. Further, the level of knowledge was particularly low with most patients suggesting that they have never received formal educational support. As a consequence, level of knowledge regarding hypertension-related complications (heart problems, retinopathy, nephropathy) or risks factors (high salt consumption; obesity, cigarette smoking and insufficient exercise) was low. Predictably, a strong relationship between poorly controlled BP and poor adherence was observed. In the multivariate analysis, we demonstrated that being male; failure to attend health talks at the clinic; high cost of transportation; low level of knowledge; and hypertension stage 3 were associated with increased likelihood of poor adherence. On the other hand, adherence was also associated with economic status with housewives presenting with higher likelihood of good adherence. By and large, our data demonstrate that decentralization of health care services and educational support, for patients and caregivers, are important intervention pathways in this population. This will require a comprehensive, evidence-based plan that promotes adherence to medication, adequate counseling and follow-up with assigned care teams.
Abbreviations
AOR, adjusted odds ratios; BMI, body mass Index; BP, blood pressure; CI, confidence interval; COR, crude odds ratios; DBP, diastolic blood pressure; EA, enumeration area; HBP, high blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; mmHg, mmHg millimeter mercury; mmol/l, mmol/l millimole per liter; NCDs, non-communicable diseases; OR, odds ratio; SBP, systolic blood pressure; SPSS, Statistical Package for the Social Sciences; WHO, World Health Organization; DASH, Dietary Approaches to Stop Hypertension.
Statement of Human and Animal Rights
All the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Data Sharing Statement
This study is part of a bigger project to assess multiple themes on hypertension in Asmara City, Eritrea. These include factors associated with hypertension, complications, patients’ knowledge, adherence to medications, among others. Further publications are expected from the dataset, which prevents us from making it public right now. However, the dataset supporting the conclusions of this article is available from the corresponding author on reasonable request.
Ethical Approval
The protocol was approved by the Research and Ethics Committee of the University of South Africa (UNISA). In addition, permission was obtained from the National Ethics Committee of the Department of Human Resource Development and Research/Ministry of Health and the Hospital Director, Halibet National Referral Hospital. Ethical approval for the study was obtained from Eritrean Ministry of Health (MOH) research ethics committee. In addition, requisite permission was obtained from the hospital director and local administration. Participants were recruited voluntarily after signing a consent form signed. This was only undertaken after the participants were provided with information on the study objective, study procedures, possible adverse effects, and the right to refuse or terminate their participation in the study at any time/stage. Information on the maintenance of data confidentiality and integrity was also provided. To ensure data confidentiality and privacy, personal identifiers such as names were not collected. Finally, all the procedures were conducted in accordance with the Declaration of Helsinki.
Acknowledgments
The authors would like to thank various personnel who helped in accomplishment of this study directly or indirectly. We would also like to thank the patients too for their consent and patience during data collection.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
There were no external funding sources for this study.
Disclosure
The authors declared no conflicts of interest for this work.
References
1. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in Blood pressure from 1975 to 2015: a pooled analysis of 1479 population – based measurement studies with 19.1 million participants. Lancet. 2017;34:389.
2. Adeloye D, Basquill C. Estimating the prevalence and awareness rates of hypertension in Africa: a systematic analysis. PLoS One. 2014;9(8):e104300. doi:10.1371/journal.pone.0104300
3. Addo J, Smeeth L, Leon DA. Hypertension in Sub-Saharan Africa: a systematic review. Hypertension. 2007;50:1012–1018. doi:10.1161/HYPERTENSIONAHA.107.093336
4. Opie LH, Seedat YK. Hypertension in sub-Saharan African populations. Circulation. 2005;112(23):3562–3568. doi:10.1161/CIRCULATIONAHA.105.539569
5. Steyn K, Sliwa K, Hawken S, et al. Risk factors associated with myocardial infarction in Africa: the INTERHEART Africa study. Circulation. 2005;112:3554–3561. doi:10.1161/CIRCULATIONAHA.105.563452
6. O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376:112–123. doi:10.1016/S0140-6736(10)60834-3
7. Dzudie A, Rayner B, Ojji D, et al. Roadmap to achieve 25% hypertension control in Africa by 2025. Cardiovasc J Afr. 2017;28(4):261–272. doi:10.5830/CVJA-2017-040
8. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. doi:10.1161/CIRCULATIONAHA.115.018912
9. Campbell NRC, Lemogoum D. Hypertension in sub-Saharan Africa: a massive and increasing health disaster awaiting solution. CVJ Africa. 2015;26(4):152–154.
10. World Health Organization. Adherence to long-term therapies. Evidence for action. Geneva, Switz: World Health Organization; 2003. Available from: http://whqlibdoc.who.int/publications/2003/9241545992.pdf.
11. Gosmanova EO, Kovesdy CP. Adherence to antihypertensive medications: is prescribing the right pills enough? Nephrol Dial Transplant. 2015;30:1649–1656. doi:10.1093/ndt/gfu330
12. Marquart de Terline D, Kramoh KE, Diop IB, et al. Poor adherence to medication and salt restriction as a barrier to reaching blood pressure control in patients with hypertension: cross-sectional study from 12 sub-Saharan countries. Arch Cardiovasc Dis. 2020;113:433–442.
13. World Health Organization. WHO STEPwise approach to surveillance (STEPS). Available from: http://www.who.int/chp/steps/en.
14. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (Mars) for the psychoses. Schizophr Res. 2000;42(3):241–247. doi:10.1016/s0920-9964(99)00130-9
15. ESH/ESC Task Force for the Management of Arterial Hypertension. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC task force for the management of arterial hypertension. J Hypertens. 2013;31:1925–1938.
16. Van de Vijner S, Akinyi H, Oti S, et al. Status report on hypertension in Africa - Consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr Med J. 2013;16:38. doi:10.11604/pamj.2013.16.38.3100
17. World Health Organization. Disease burden estimates. Geneva:World Health Organisation; 2009.
18. Macquart de Terline D, Kane A, Kramoh KE, et al. Factors associated with poor adherence to medication among hypertensive patients in twelve low and middle income Sub-Saharan countries. PLoS One. 2019;14(7):e0219266. doi:10.1371/journal.pone.0219266
19. Boima V, Ademola AD, Odusola AO, et al. Factors associated with medication nonadherence among hypertensives in Ghana and Nigeria. Int J Hypertens. 2015;8. doi:10.1155/2015/205716
20. Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA. Nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Medicine. 2017;96(4):e5641. PMID: 28121920. doi:10.1097/MD.0000000000005641
21. Girma F, Emishaw S, Alemseged F, Mekonnen A. Compliance with anti-hypertensive treatment and associated factors among hypertensive patients on follow-up in Jimma University Specialized Hospital, Jimma, South West Ethiopia: a Quantitative Cross-Sectional Study. J Hypertens. 2014;3:174. doi:10.4172/2167-1095.1000174
22. Abere DA, Getahun AA, Zelalem BM, et al. Adherence to antihypertensive treatment and associated factors among patients on follow up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health. 2012;12:282. doi:10.1186/1471-2458-12-282
23. Alsolami F, Correa – Velez I, Hou XY. Factors affecting Antihypertensive medications adherence among hypertensive patients in Saudi Arabia. Am J Med Med Sci. 2015;5(4):181–189. doi:10.5923/j.ajmms.20150504.07
24. Esmaeili R, Matlabi M, Khajavi A, Aliasghari E, Sajjadi M. Factors affecting adherence to antihypertensive medication: results from a rural population study in East of Iran. Glob J Health Sci. 2017;9(5):286–291. doi:10.5539/gjhs.v9n5p286
25. Bramley TJ, Gerbino PP, Nightengale BS, et al. Relationship of blood pressure control to adherence with antihypertensive monotherapy in 13 managed care organizations. J Manag Care Pharm. 2006;12:239–245. doi:10.18553/jmcp.2006.12.3.239
26. Nielsen JO, Shrestha AD, Neupane D, Kallestrup P. Non-adherence to anti-hypertensive medication in low- and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens. 2017;31(1):14–21. PMID: 27306087. doi:10.1038/jhh.2016.31
27. Gupta P, Patel P, Štrauch B, et al. Risk factors for non-adherence to antihypertensive treatment. Hypertension. 2017;69:1113–1120. doi:10.1161/HYPERTENSIONAHA.116.08729
28. Lowry KP, Dudley TK, Oddone EZ, et al. Intentional and unintentional nonadherence to antihypertensive medication. Ann Pharmacother. 2005;39:1198Y1203. doi:10.1345/aph.1E594
29. Al-Ramahi R. Adherence to medications and associated factors: a cross-sectional study among Palestinian hypertensive patients. J Epidemiol Glob Health. 2015;5:125–132. doi:10.1016/j.jegh.2014.05.005
30. Najjuma JN, Breenaman L, Nabirye RC, et al. Adherence to antihypertensive medication: an interview analysis of Southwest Ugandan patients’ perspectives. adherence to antihypertensive medication: an interview analysis of Southwest Ugandan patients’ perspectives. Ann Global Health. 2020;86(1):58, 1–11. doi:10.5334/aogh.2904
31. Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30. doi:10.7326/0003-4819-133-1-200007040-00004
32. Bhatia S, Landier W, Hageman L, et al. Systemic exposure to thiopurines and risk of relapse in children with acute lymphoblastic leukemia: a Children’s Oncology Group Study. JAMA Oncol. 2015;1(3):287–295. doi:10.1001/jamaoncol.2015.0245
33. Lo SHS, Chau JPC, Woo JM, Thompson DR, Choi KC. Adherence to antihypertensive medication in older adults with hypertension. J Cardiovasc Nurs. 2016;31(4):296Y303.
34. Nsitou MB, Ikama MS, Drame B, Kaboru BB. Patients-related predictors of poor adherence to antihypertensive treatment in Congo-Brazzaville: a Cross-Sectional Study. Global J Med Public Health. 2013;2:155.
35. Ayodapo AO, Elegbede OT, Omosanya OE, Monsudi KF. Patient education and medication adherence among hypertensives in a tertiary hospital, South Western Nigeria. Ethiop J Health Sci. 2020;30(2):243. doi:10.4314/ejhs.v30.i2.12
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
