Back to Journals » Patient Preference and Adherence » Volume 16
Antibiotics Self-Medication Practice and Associated Factors Among Residents in Dessie City, Northeast Ethiopia: Community-Based Cross-Sectional Study
Received 15 April 2022
Accepted for publication 9 August 2022
Published 17 August 2022 Volume 2022:16 Pages 2159—2170
DOI https://doi.org/10.2147/PPA.S370925
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Johnny Chen
Wudneh Simegn,1 Getachew Moges2
1Department of Social and Administrative Pharmacy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 2Department of Pharmacy, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Wudneh Simegn, Email [email protected]
Background: Taking antibiotics without prescription would result in the emergency of antibiotics resistance. The aim of this study was to assess antibiotics self-medication practice and associated factors among residents in Dessie City, Ethiopia.
Methods: A community-based cross-sectional was employed from June to July 2021. A total of 407 participants have been selected from each Kebele by stratified and systematic random sampling techniques. The collected data were checked, translated and exported into SPSS version 26. Results were organized using frequency and percentage tables. Bi-variate and multi-variable logistic regressions were used to test the association of independent variables with antibiotics self-medication practice.
Results: Four hundred and seven participants enrolled with a response of 96.7%. One hundred and fifty-two (37.3%) were females, and 115 (28.3%) respondents have taken antibiotics in the last 6 months. The prevalence of antibiotics self-medication practice was 55.3% (95% CI: 50.6– 60.2). Amoxicillin (45%), Ciprofloxacin (36%), and Amoxicillin with clavulanic acid (24%) were commonly used antibiotics. Cough (34.4), fever (30.7), cold and flu (29.0), diarrhea (21.9) and headache (18.7) were the most reported conditions that necessitate antibiotics self-medication. Educational level (8– 10 grade) (AOR = 4.10, 95% CI: 1.28, 13.12), using mass media as a source of information (AOR = 2.23, 95% CI: 1.24, 4.27), relying on previous experience for source of information (AOR = 2.02, 95% CI: 1.23, 3.31), having awareness of antibiotics resistance (AOR = 2.45, 95% CI: 1.34, 4.50) and good knowledge of antimicrobial resistance (AOR = 1.81, 95% CI: 1.11, 2.97) were significantly associated with antibiotics self-medication practice.
Conclusion: Antibiotics self-medication practice among residents was high. Educational status, using mass media and previous experiences as sources of information on antibiotics, having awareness of antibiotics resistance, and knowledge of antimicrobial resistance were significantly associated with self medication of antibiotics. Attention should be given by the stakeholders to reduce self medication practice with antibiotics.
Keywords: antibiotics, self-medication practice, associated factors, residents
Introduction
Antibiotics have been used to treat infectious diseases and are often used as a substitute for basic healthcare.1,2 Self-medication is a common practice in the healthcare system and part of self-care practice.3 The World Health Organization (WHO) has confirmed that antibiotics self-medication practice is an inappropriate method of utilizing these medicines.4 However, antibiotic self-medication is the most rapidly emerging problem and common in low- and middle-income countries.5 As the healthcare facilities do not meet the standard of care and are even quite expensive, self-medication practice has become an easy and necessary medical choice.6
Antibiotics self-medication has been confirmed to be the major cause of facilitating the clinical problem of antimicrobial resistance (AMR).7 AMR is an important threat to international health and the main global health challenge8 predominantly in developing countries9 and is partly related to high levels of antibiotics use.10,11 Globally, AMR causes estimated 700,000 deaths each year12 and can result in reduced efficacy of drugs, difficult to treat infections, costly, or even impossible to achieve therapeutic outcomes and ends up with prolonged illness and mortality.13 The literature emphasized that Ethiopia experiences a serious burden of infectious diseases with a high incidence of disease morbidity and mortality,14 probably due to higher AMR. For that matter, there are signs of irrational use of antibiotics by the society, patients and healthcare providers in the county.15
Several studies have reported the prevalence of antibiotic self-medication among the public in Ethiopia. In Ambo (47.9%), in Gondar Town (36.8%) and in Addis Ababa (67.3%) were reported.16–18 Several contributing factors were described for antibiotics self-medication. Among these, age, educational level, experience, poor knowledge, healthcare costs, income, and inadequate access to health professionals were mainly documented.6,19–22
Assessing the prevalence of antibiotics self-medication practice among the public will help to take immediate measures to prevent the further development of AMR. To the knowledge of the investigators, there were no previous local studies that investigated antibiotics self-medication practice among the residents in Dessie City. Therefore, the current study aimed to assess antibiotics self-medication practice and the associated factors among residents in Dessie City, northeast Ethiopia.
Methods
Study Area, Design, and Period
A community-based cross-sectional study was employed in Dessie City, Northeast Ethiopia. Dessie is a multi-ethnic city located in the South Wollo zone of Amhara Regional State, 401 km away from Addis Ababa, the capital city of Ethiopia. Based on the 2007 national census conducted by the Central Statistical Agency of Ethiopia (CSA), Dessie City had a total population of 151,174, of which 72,932 were male and 78,242 were female.23 The 2007 national census reported 59% of the inhabitants practiced Christianity and 41% of the population practiced Islam. The City administration reported 481,442 people in the 2020/2021 budget year. Recently, the City was reorganized into ten sub-city administrations and six rural kebeles. The study period was from June 30 to July 30, 2021.
Population
All residents living in Dessie City were used as the source population. The study population were residents who were eligible for the study and present at the time of data collection from June 30 to July 30, 2021. Residents who were under 18 years of age; who were health professionals; who were severely ill or unable to speak; and living less than six months in the City were excluded.
Sample Size Calculation and Sampling Technique
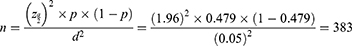
The sample size (n) was 421 which was calculated using a single population proportion formula by using a previous study in Ambo, Ethiopia (47.9%)16 and adding a non-response rate of 10%.
Considering, 10% non-response rate, the final sample became = 421.
Stratified sampling technique was used to proportionally allocate the households to each kebele administration. In Dessie City, there were 20 Kebeles in five sub-city administrations and 6 rural Kebeles. We selected 5 kebeles (Dawudo, Ager Gizat, Robit, Tekuam, and Kelemmeda) from the City and 3 Kebeles from the Rural part (Gerado Tesfanech, Boru Meda and Gerado Kelina) by lottery method (Figure 1). The current number of households was taken from the City administration. A list of households with their respective addresses was taken from each Kebele administrative office. From each stratum, samples were taken proportional to their size by taking the number of the households as the sampling frame. Households from each Kebele of urban stratum and from each kebele of rural stratum were selected using a systematic random sampling technique. The sampling interval for each kebele was determined by dividing the total number of households in each kebele to its proportionally allocated sample size. Then, every Kth value of households were interviewed by selecting the first household using lottery method.
 |
Figure 1 Schematic presentation of sampling procedure. |
Data Collection Instrument and Procedure
The data collection tool was a semi-structured, pretested questionnaire to collect the required data adapted from the previous study.24,25 The questionnaire had three parts. Part one included socio-demographic characteristics such as sex, age, residence, religion, marital status, educational status, occupation, and average monthly income. Part two included questions to assess antibiotics self-medication practice; the source of information about antibiotics; source of antibiotics; awareness of antibiotic resistance; diseases that necessitate antibiotics self-medication; and the commonly used antibiotics for self-medication. The third part included eight true or false questions to measure knowledge of AMR. The questionnaire was prepared by the electronic google-form to reduce the cost of paper duplication and to prevent the transmission of COVID-19. We provided the online-google form and gave access to the data collectors. The data collectors used smartphones by accessing mobile data packages from the local telecommunication center. After the consent was taken to participate, the data collectors opened the google-form and interviewed the head of the household or a member of the household being the next head or responsible person of the household (if the head of the household was not present at the time of data collection) with consent to participate. If the household members were absent (closed house) during the data collection period, or when the households were within the exclusion criteria, the nearby households found next to it were used. While the households did not voluntarily participate or were unable to complete the interview, the authors have considered it for non-response calculation. The questionnaire had been translated to local language (Amharic) and then back translated to English language by experts of the two languages (English and Amharic).
Data Quality Control
Pretest was done among 20 residents outside of the study area (Gondar town) and we amended the questionnaire based on the difficulties we faced during the pretest. The data collectors were trained for the purpose of study and ethical issues in the process of data gathering. There was an active involvement of the first author (Wudneh Simegn, lecturer of pharmacy) in the data collection process.
Statistical Analysis
The collected data were exported to excel and translated to English language then exported to SPSS Version 26 for computing, recording, and statistical analysis. Mean with standard deviation (SD), and frequency with percent were computed to descriptive results of the study. We used logistic regression to explain the relationship between antibiotics self-medication and independent variables. Independent variables with a p-value of <0.2 were selected for multi-variable logistic regression. A variable with a p-value of ≤0.05 with 95% CI was treated as a significant factor for antibiotics self-medication practice.
Operational Definitions and Terminologies
Kebele
It is the smallest administrative unit of the community under the sub-city.
Antibiotics
Antibiotics are a group of medicines derived from certain microorganisms, including fungi and bacteria that combat bacterial infections by killing the bacteria or by making it hard for the bacteria to grow and multiply.
Antibiotics Self-Medication Practice
It is the use of antibiotics without the prescription of healthcare professionals. Those residents who ever took antibiotics without prescription by health professionals are considered as antibiotics self-medication. The measuring technique was the prevalence of antibiotics self-medication as a point estimate with 95% CI, similar to the previous study.26
Awareness of Antibiotics Resistance
Respondents were asked a single self-reported question about whether they know antibiotic resistance or not. Respondents who answered “Yes” were considered to have awareness of antibiotics resistance.
Knowledge of AMR
Respondents were introduced to answer eight true or false questions provided by WHO knowledge assessment criteria for AMR.25 Respondents who scored ≥75% were considered to have good AMR knowledge.
Results
Socio-Demographic Characteristics
In the current study, 407 participants enrolled with a response of 96.7%. About 152 (37.3%) were females. The mean age of the participants was 35.63 ± 8.63 and ranged 20 −68 years. Majority (88.7%) of the participants were from Urban parts of the City and followers of Muslim (43.0%) followed by the Orthodox religion (39.8%). A few of participants (7.4%) were unable to read and write, while most of the participants attended grade 11–12 and (30.2%) college and above (25.3%). About 158 (38.8%) of the study participants are merchants followed by employees (24.3%) and house wife (16.2%) (Table 1).
 |
Table 1 Sociodemographic Characteristics of Study Participants in Dessie City, Northeast Ethiopia, 2021 (n = 407) |
Antibiotics Self-Medication Practice
The present study revealed that self medication practice with antibiotics among residents of Dessie City was 55.3% (95% CI: 50.6–60.2). 115 (28.3%), 114 (28.0%), 94 (23.1%), and 66 (16.2%) of the respondents have taken antibiotics in the last 6 months, in the last year, more than a year ago and in the last month, respectively. 245 (60.2%) of the respondents reported that they got advice from healthcare professionals. Majority (64.9%) of the respondents have got information about antibiotics from healthcare professionals followed by friends/family (46.2%) and from their previous experience (38.3%).
In the current study, most respondents (68.3%) finished their antibiotics as advised by the health professionals (community pharmacists) and considered the time gap advised between doses during antibiotics use (66.6%). On the other hand, respondents reported that they stopped taking antibiotics when they feel better after a few days (41.0%), stopped the drug due to time deviation from the normal schedule (33.2%), and have stopped an antibiotic due to negligence, being fed up, and bored (29.5%). The main source of antibiotics is retail outlet pharmacies (41.8) followed by from friends or family members (28.7). Healthcare professionals (64.9) and friends/family (46.2) were the major source of information about antibiotics (Table 2).
 |
Table 2 Related to Antibiotics Self-Medication Among Study Participants in Dessie City, North East Ethiopia, 2021 (n = 407) |
Diseases for Antibiotics Self-Medication and Commonly Used Antibiotics
Cough (34.4%), fever (30.7%), cold and flu (29.0%) diarrhea (21.9%) and headache (18.7%) were the most reported conditions where antibiotics are used as self-medication (not prescription) (Figure 2). Amoxicillin (45%), followed by Ciprofloxacin (36%), and Amoxicillin with clavulanic acid (24%) were used by the highest number of respondents for self-medication (Figure 3).
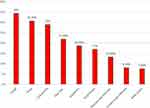 |
Figure 2 Diseases that necessitate antibiotics self-medication among Residents of Dessie City, Northeast Ethiopia, 2021 (n=407). |
 |
Figure 3 Commonly used antibiotics for self-medication among Residents of Dessie City, Northeast Ethiopia, 2021 (n=407). |
Factors Associated with Antibiotic Self-Medication Practice
Gender, age, residence, educational status, area of residence, using health professionals as sources of information on antibiotics, using mass media as source of information on antibiotics, relying on previous experience for source of information on antibiotics, awareness of the term antibiotics resistance, and Knowledge of AMR were candidate variables for multi-variable regression. In the final model, grade 8–10 educational status (AOR = 4.10, 95% CI:1.28, 13.12), using mass media as source of information on antibiotics (AOR = 2.23, 95% CI:1.24, 4.27), relying on previous experience for source of information on antibiotics (AOR = 2.02, 95% CI:1.23, 3.31), awareness of the term antibiotics resistance (AOR = 2.45, 95% CI:1.34, 4.50) and Knowledge of AMR (AOR = 1.81, 95% CI:1.11, 2.97), were significantly associated with self medication with antibiotics (Table 3).
 |
Table 3 Factors Associated with Antibiotics Self-Medication Among Residents of Dessie City, Northeast Ethiopia, 2021 (n = 407) |
Discussion
The current study assessed antibiotics self-medication practice and associated factors among residents in Dessie City, northeast Ethiopia. In this study, over half of the study participants used antibiotics self medication practice (55.3%). This might be due to time taking of medical observation at the health facility; to reduce medical costs for diagnosis; easy availability of antibiotics at the drug retail outlets and poor standard of care provided by health facilities.6 Even though antibiotics are classified as prescription-only medicines that are not allowed to be sold without health practitioners’ prescription in Ethiopia, they are sold in retail pharmacies without prescription.27–29 The reason might be the influence of pharmacy owners to maximize their revenue, weak regulatory mechanism of the health administrator and professional conflicts of interest.28 This practice could increase misuse and overuse of antibiotics, which in turn aiding the clinical problem of AMR and ends up with sustained illness and mortality,7,13,30 which need educating both drug sellers (retail outlets) and the general population. The result is in line with a systematic review and meta analysis conducted in Africa (median prevalence = 55.7%).5 This result was higher than the study conducted in Gondar Town (36.8%), in Ambo (47.9%), in Eritrea (45.1%), in Malaysia (15.1%), Sri Lanka (2.6%) and others conducted elsewhere.15,16,19,24,26,31–38 The result is also lower than the study conducted in Addis Ababa (67.3%) and Harer (65%).18,39 The difference might be the methods used, socio-demographic factors, study setting and the healthcare policy of the country. In this study, most of the respondents (46.2%) reported that their friends/family members were the source of information for antibiotics self-medication. This is a high opportunity for misuse of antibiotics as there may not have any information about the use of the antibiotics beyond the absence of the diagnosis for antibiotics use. This is higher than study in Nigeria (15.1%)40 and lower than in Egypt (67.4%).41
The most commonly used antibiotics were found to be Amoxicillin (45%), Ciprofloxacin (36%), and Amoxicillin with clavulanic acid (24%) for self medication. Other studies in Addis Ababa and South Ethiopia also revealed amoxicillin and ciprofloxacin were the most commonly used antibiotics for self medication.18,42 Prior antibiotic exposure would result in an emergency of antibiotics resistance.43
Cough, which is mainly caused by respiratory infection, usually self-limiting and does not need antibiotic treatment as antibiotics, cannot be used to treat all kinds of infections30 and the majority of these infections are of viral origin. However, it is described in the current study and in several studies for reasons of antibiotics self-medication. In Uyo, Nigeria, cold and cough (33%),30 in England (38%),38 in Tanzania, cough (68.0%), urinary tract infections (53.4%), and diarrhea (48.5%) were the most conditions reported.44 Study conducted in Nigeria, skin/wound infection (77.2%) and bladder infection (68.9%) were majorly described.40 In Namibia, cold and flu was mainly recognized by most respondents.36 The difference might be attributed to the difference in the prevalence of the disease: variation in the study population and the healthcare system in each country. In Ethiopia, it is not allowed by law to take antibiotics without a prescription. However, community pharmacists are selling the antibiotics without prescription due to poor control mechanisms of the drug regulatory authority in the country.
The main source of antibiotics is retail outlet pharmacies (41.8) followed by from friends or family members (28.7). A previous study in Ethiopia reported that more than half of the community pharmacists (58%) sold antibiotics without a prescription.29 This indicated lower regulatory enforcement of the health administrators to control selling of antibiotics without prescription.
In the current study, educational status, using mass media as source of information on antibiotics, using the previous experience as a source of information on antibiotics, awareness of antibiotic resistance, and knowledge of AMR, were significantly associated with antibiotics self medication practice.
Educational status (grade 8–10) had about four odds of higher prevalence of antibiotics – self medication practice – than those uneducated residences. This is supported by a systematic review and meta-analysis of self medication practice with antibiotics in developing countries.19 In contrast to the current study, lower educational level or illiteracy was associated with antibiotics self-medication in the previous studies.21,45
Respondents using mass-media as a source of information for antibiotics use had about two times higher prevalence of antibiotics self-medication. In Pakistan, media advertisements were the most common source of information for self medication practice.46 Mass-media might give clues about the name of antibiotics that initiate users but would provide false information about antibiotics that result in inappropriate use.47
Respondents using their previous experience as a source of information for antibiotics use had more than two odds of higher prevalence of antibiotics self-medication as compared to those respondents who did not use their previous experience. It is also supported by previous research works that past successful experience contributed to antibiotics self-medication.19,21,48
In the current study, awareness of the AMR and good knowledge of AMR were significantly associated with antibiotics self-medication. This might be due to evidence of antibiotics use that would induce antibiotics self-medication practice. The association was supported by the study conducted in Sri Lanka that revealed having good knowledge of antibiotics was significantly associated with antibiotics self-medication.49 Similarly, academic knowledge also contributed to antibiotics self-medication.50 In contrast to the current study, research conducted in East Indonesia revealed that poor knowledge had higher chances of antibiotics self-medication.20 The possible difference might be the study methods, setting and the healthcare system of the country.
This study had several limitations, such as recall bias leading to inability to remember the type of antibiotics used and social desirability leading to misinformation; cause-effect relationship cannot be established as it was a cross-sectional study design. The current study also did not consider the design effect resulting in a smaller sample size.
Conclusions
In the current study, antibiotics self-medication practice among the residents was high. Cough, fever, cold and flu, and diarrhea were the most reported conditions for self-medication practice with antibiotics. Amoxicillin, Ciprofloxacin and Amoxicillin with clavulanic acid were commonly used antibiotics for self-medication. At the educational level, using mass media as a source of information for antibiotics use, using previous experience as a source of information for antibiotics use, having awareness of AMR, and good knowledge of AMR were significantly associated with antibiotics self-medication. Stakeholders should take measures to discourage taking antibiotics without prescription through awareness campaigns to the public and enforcing antibiotics selling laws to the community pharmacy sellers.
Abbreviations
AMR, Antimicrobial Resistance; WHO, World Health Organization; CI, Confidence Interval.
Data Sharing Statement
The data set is available to the corresponding author upon reasonable request.
Ethical Considerations
Ethical approval was obtained from Wollo University College of Medicine and Health Sciences, Department of Pharmacy Ethics Review Committee and a support letter was taken to Dessie City Administration. After we got a permission letter from the City Administration, a copy of the permission letter was given to each Kebel administration office. Participants were informed about their rights and the purpose of the research. Only those who gave consent were interviewed. The required precautions were taken to ensure confidentiality, and no personal identifiers were incorporated in the Declaration of Helsinki.51
Acknowledgment
We would like to acknowledge Mr. Degu Dagnew (Facilitator of Data Collectors), Wollo University, Dessie City Administration and to all study participants.
Author Contributions
Both authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that there are no conflicts of interest.
References
1. Carlet J, Collignon P, Goldmann D, et al. Society’s failure to protect a precious resource: antibiotics. Lancet. 2011;378(9788):369–371. doi:10.1016/S0140-6736(11)60401-7
2. World Health Organization. Antimicrobial Resistance and Primary Health Care. World Health Organization; 2018.
3. Shafie M, Eyasu M, Muzeyin K, Worku Y, Martín-Aragón S. Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLoS One. 2018;13(3):e0194122. doi:10.1371/journal.pone.0194122
4. Shrivastava SR, Shrivastava PS. Antimicrobial resistance: global scenario and its relation with nation’s development. Libyan J Med Sci. 2019;3(1):34. doi:10.4103/LJMS.LJMS_41_18
5. Yeika EV, Ingelbeen B, Kemah BL, Wirsiy FS, Fomengia JN, Van der Sande MA. Comparative assessment of the prevalence, practices and factors associated with self‐medication with antibiotics in Africa. Trop Med Int Health. 2021;26(8):862–881. doi:10.1111/tmi.13600
6. Rather IA, Kim B-C, Bajpai VK, Park Y-H. Self-medication and antibiotic resistance: crisis, current challenges, and prevention. Saudi J Biol Sci. 2017;24(4):808–812. doi:10.1016/j.sjbs.2017.01.004
7. Ramay BM, Lambour P, Cerón A. Comparing antibiotic self-medication in two socio-economic groups in Guatemala City: a descriptive cross-sectional study. BMC Pharmacol Toxicol. 2015;16(1):1–8. doi:10.1186/s40360-015-0011-3
8. Williams PC, Isaacs D, Berkley JA. Antimicrobial resistance among children in sub-Saharan Africa. Lancet Infect Dis. 2018;18(2):e33–e44. doi:10.1016/S1473-3099(17)30467-X
9. Founou RC, Founou LL, Essack SY. Clinical and economic impact of antibiotic resistance in developing countries: a systematic review and meta-analysis. PLoS One. 2017;12(12):e0189621. doi:10.1371/journal.pone.0189621
10. Sakeena M, Bennett AA, Carter SJ, McLachlan AJ. A comparative study regarding antibiotic consumption and knowledge of antimicrobial resistance among pharmacy students in Australia and Sri Lanka. PLoS One. 2019;14(3):e0213520. doi:10.1371/journal.pone.0213520
11. Huttner A, Harbarth S, Carlet J, et al. Antimicrobial resistance: a global view from the 2013 World Healthcare-Associated Infections Forum. Antimicrob Resist Infect Control. 2013;2(1):1–13. doi:10.1186/2047-2994-2-31
12. Varma JK, Oppong-Otoo J, Ondoa P, et al. Africa Centres for Disease Control and Prevention’s framework for antimicrobial resistance control in Africa. African J Lab Med. 2018;7(2):1–4. doi:10.4102/ajlm.v7i2.830
13. Holmberg SD, Solomon SL, Blake PA. Health and economic impacts of antimicrobial resistance. Rev Infect Dis. 1987;9(6):1065–1078. doi:10.1093/clinids/9.6.1065
14. Misganaw A, Haregu TN, Deribe K, et al. National mortality burden due to communicable, non-communicable, and other diseases in Ethiopia, 1990–2015: findings from the Global Burden of Disease Study 2015. Popul Health Metr. 2017;15(1):1–17. doi:10.1186/s12963-016-0118-9
15. Erku DA, Mekuria AB, Belachew SA. Inappropriate use of antibiotics among communities of Gondar town, Ethiopia: a threat to the development of antimicrobial resistance. Antimicrob Resist Infect Control. 2017;6(1):112. doi:10.1186/s13756-017-0272-2
16. Ayana H, Sileshi T, Bule MH, Chaka EE. Non-prescription antibiotics use and associated factors among drug retail outlets in Ambo, Ethiopia: a cross-sectional study. Patient Prefer Adherence. 2021;15:2739. doi:10.2147/PPA.S337364
17. Jember E, Feleke A, Debie A, Asrade G. Self-medication practices and associated factors among households at Gondar town, Northwest Ethiopia: a cross-sectional study. BMC Res Notes. 2019;12(1):1–7. doi:10.1186/s13104-019-4195-2
18. Bogale AA, Amhare AF, Chang J, et al. Knowledge, attitude, and practice of self-medication with antibiotics among community residents in Addis Ababa, Ethiopia. Expert Rev Anti Infect Ther. 2019;17(6):459–466. doi:10.1080/14787210.2019.1620105
19. Pavydė E, Veikutis V, Mačiulienė A, Mačiulis V, Petrikonis K, Stankevičius E. Public knowledge, beliefs and behavior on antibiotic use and self-medication in Lithuania. Int J Environ Res Public Health. 2015;12(6):7002–7016. doi:10.3390/ijerph120607002
20. Kurniawan K, Posangi J, Rampengan N. Association between public knowledge regarding antibiotics and self-medication with antibiotics in Teling Atas Community Health Center, East Indonesia. Med J Indones. 2017;26(1):62–69. doi:10.13181/mji.v26i1.1589
21. Moonajilin MS, Mamun MA, Rahman ME, et al. Prevalence and drivers of self-medication practices among savar residents in Bangladesh: a cross-sectional study. Risk Manag Healthc Policy. 2020;13:743. doi:10.2147/RMHP.S256272
22. Ali I, Khan AU. Self-medication of antibiotics: a perspective on alarming situation in Peshawar, Khyber Pakhtunkhwa, Pakistan. Arch Pharm Pract. 2015;6(3):68. doi:10.4103/2045-080X.160993
23. Woldie SH. Women in the informal sector: retrospect’s and socioeconomic response in Dessie town, Ethiopia: the case of parallel trading. Int J Dev Soc. 2015;4(2):85–94.
24. Mengesha Y, Manaye B, Moges G. Assessment of public awareness, attitude, and practice regarding antibiotic resistance in Kemissie Town, Northeast Ethiopia: community-based cross-sectional study. Infect Drug Resist. 2020;13:3783. doi:10.2147/IDR.S280036
25. World Health Organization. Antibiotic Resistance: Multi-Country Public Awareness Survey. World Health Organization; 2015.
26. Rathish D, Wickramasinghe ND. Prevalence, associated factors and reasons for antibiotic self-medication among dwellers in Anuradhapura: a community-based study. Int J Clin Pharm. 2020;42(4):1139–1144. doi:10.1007/s11096-020-01065-6
27. Damisie G, Hambisa S, Yimam M. Over the counter sale of antibiotics at drug stores found in Mizan-Aman Town, Southwest Ethiopia: a cross-sectional simulated client visit study. J Pharm. 2019;2019:1–6. doi:10.1155/2019/3510659
28. Gebretekle GB, Serbessa MK. Exploration of over the counter sales of antibiotics in community pharmacies of Addis Ababa, Ethiopia: pharmacy professionals’ perspective. Antimicrob Resist Infect Control. 2016;5(1):1–7. doi:10.1186/s13756-016-0101-z
29. Belachew SA, Hall L, Selvey LA. Community drug retail outlet staff’s knowledge, attitudes and practices towards non-prescription antibiotics use and antibiotic resistance in the Amhara region, Ethiopia with a focus on non-urban towns. Antimicrob Resist Infect Control. 2022;11(1):1–14. doi:10.1186/s13756-022-01102-1
30. Asogwa IE, Offor SJ, Mbagwu HOC. Knowledge, attitude and practice towards antibiotics use among non-medical university students in Uyo, Nigeria. J Adv Med Pharm Sci. 2017;15:1–11. doi:10.9734/JAMPS/2017/35671
31. Ateshim Y, Bereket B, Major F, et al. Prevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea: a descriptive cross sectional survey. BMC Public Health. 2019;19(1):1–7. doi:10.1186/s12889-019-7020-x
32. Aslam A, Zin CS, Ab Rahman NS, Gajdács M, Ahmed SI, Jamshed S. Self-medication practices with antibiotics and associated factors among the public of Malaysia: a cross-sectional study. Drug Healthc Patient Saf. 2021;13:171. doi:10.2147/DHPS.S331427
33. Abasaeed A, Vlcek J, Abuelkhair M, Kubena A. Self-medication with antibiotics by the community of Abu Dhabi Emirate, United Arab Emirates. J Infect Dev Countries. 2009;3(07):491–497. doi:10.3855/jidc.466
34. Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One. 2013;8(12):e84177. doi:10.1371/journal.pone.0084177
35. Aldhafar AS, Talat W. Knowledge, attitude, and practice toward the usage of antibiotics among public in Al-Ahsa, Saudi Arabia. Target. 2016. doi:10.17354/ijss/2017/39
36. Pereko DD, Lubbe MS, Essack SY. Public knowledge, attitudes and behaviour towards antibiotic usage in Windhoek, Namibia. South African J Infect Dis. 2015;30(4):27–29. doi:10.1080/23120053.2015.1107290
37. Chen C, Chen Y-M, Hwang K-L, et al. Behavior, attitudes and knowledge about antibiotic usage among residents of Changhua, Taiwan. J Microbiol Immunol Infect. 2005;38(1):53–59.
38. McNulty CA, Collin SM, Cooper E, Lecky DM, Butler CC. Public understanding and use of antibiotics in England: findings from a household survey in 2017. BMJ open. 2019;9(10):e030845. doi:10.1136/bmjopen-2019-030845
39. Jifar A, Ayele Y. Assessment of knowledge, attitude, and practice toward antibiotic use among Harar City and its surrounding community, Eastern Ethiopia. Interdiscip Perspect Infect Dis. 2018;2018:1–6. doi:10.1155/2018/8492740
40. Chukwu EE, Oladele DA, Awoderu OB, et al. A national survey of public awareness of antimicrobial resistance in Nigeria. Antimicrob Resist Infect Control. 2020;9:1–10. doi:10.1186/s13756-020-00739-0
41. Refaei SA, Emam SA. The Concept of Antibiotic Resistance Among the Rural Population. Google Scholar; 2019.
42. Mossa DA, Wabe NT, Angamo MT. Self-medication with antibiotics and antimalarials in the community of Silte zone, South Ethiopia. TAF Prev Med Bull. 2012;11(5):529–536. doi:10.5455/pmb.1-1314892446
43. Martínez-Casanova J, Gómez-Zorrilla S, Prim N, et al. Risk factors for amoxicillin-clavulanate resistance in community-onset urinary tract infections caused by Escherichia coli or Klebsiella pneumoniae: the role of prior exposure to fluoroquinolones. Antibiotics. 2021;10(5):582. doi:10.3390/antibiotics10050582
44. Sindato C, Mboera LE, Katale BZ, et al. Knowledge, attitudes and practices regarding antimicrobial use and resistance among communities of Ilala, Kilosa and Kibaha districts of Tanzania. Antimicrob Resist Infect Control. 2020;9(1):1–17. doi:10.1186/s13756-020-00862-y
45. Jamhour A, El-Kheir A, Salameh P, Abi Hanna P, Mansour H. Antibiotic knowledge and self-medication practices in a developing country: a cross-sectional study. Am J Infect Control. 2017;45(4):384–388. doi:10.1016/j.ajic.2016.11.026
46. Aziz MM, Masood I, Yousaf M, Saleem H, Ye D, Fang Y. Pattern of medication selling and self-medication practices: a study from Punjab, Pakistan. PLoS One. 2018;13(3):e0194240. doi:10.1371/journal.pone.0194240
47. Im H, Huh J. Does health information in mass media help or hurt patients? Investigation of potential negative influence of mass media health information on patients’ beliefs and medication regimen adherence. J Health Commun. 2017;22(3):214–222. doi:10.1080/10810730.2016.1261970
48. Nazir S, Azim M. Assessment of antibiotic self-medication practice among public in the northwestern region of Pakistan. Eur J Hosp Pharm. 2017;24(4):200–203. doi:10.1136/ejhpharm-2015-000733
49. Zawahir S, Lekamwasam S, Halvorsen KH, Rose G, Aslani P. Self-medication Behavior with antibiotics: a national cross-sectional survey in Sri Lanka. Expert Rev Anti Infect Ther. 2021;19(10):1341–1352. doi:10.1080/14787210.2021.1911647
50. Khalid S, Ali Q, Hafeez M, Malik A. Perception regarding self-medication of antibiotics in general public sector university of Southern Punjab: a comparison between medical and non-medical students. Biol Clin Sci Res J. 2021;2021(1). doi:10.54112/bcsrj.v2021i1.51
51. General Assembly of the World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81(3):14–18.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.