Back to Journals » OncoTargets and Therapy » Volume 9
Analgesic effectiveness and tolerability of oral oxycodone/naloxone and pregabalin in patients with lung cancer and neuropathic pain: an observational analysis
Authors De Santis S , Borghesi C, Ricciardi S, Giovannoni D, Fulvi A, Migliorino MR, Marcassa C
Received 10 March 2016
Accepted for publication 12 May 2016
Published 4 July 2016 Volume 2016:9 Pages 4043—4052
DOI https://doi.org/10.2147/OTT.S108144
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Min Li
Stefano De Santis,1 Cristina Borghesi,1 Serena Ricciardi,2 Daniele Giovannoni,1 Alberto Fulvi,2 Maria Rita Migliorino,2 Claudio Marcassa3
1Palliative Care and Cancer Pain Service, Oncological Pulmonary Unit, 2Oncological Pulmonary Unit, San Camillo-Forlanini Hospitals, Rome, 3Cardiologia Fondazione Maugeri IRCCS, Novara, Italy
Introduction: Cancer-related pain has a severe negative impact on quality of life. Combination analgesic therapy with oxycodone and pregabalin is effective for treating neuropathic cancer pain. We investigated the efficacy and tolerability of a dose-escalation combination therapy with prolonged-release oxycodone/naloxone (OXN-PR) and pregabalin in patients with non-small-cell lung cancer and severe neuropathic pain.
Methods: This was a 4-week, open-label, observational study. Patients were treated with OXN-PR and pregabalin. Average pain intensity ([API] measured on a 0–10 numerical rating scale) and neuropathic pain (Douleur Neuropathique 4) were assessed at study entry and at follow-up visits. The primary endpoint was response to treatment, defined as a reduction of API at T28 ≥30% from baseline. Secondary endpoints included other efficacy measures, as well as patient satisfaction and quality of life (Brief Pain Inventory Short Form), Hospital Anxiety and Depression Scale, and Symptom Distress Scale; bowel function was also assessed.
Results: A total of 56 patients were enrolled. API at baseline was 8.0±0.9, and decreased after 4 weeks by 48% (4.2±1.9; P<0.0001 vs baseline); 46 (82.1%) patients responded to treatment. Significant improvements were also reported in number/severity of breakthrough cancer pain episodes (P=0.001), Brief Pain Inventory Short Form (P=0.0002), Symptom Distress Scale (P<0.0001), Hospital Anxiety and Depression Scale depression (P=0.0006) and anxiety (P<0.0001) subscales, and bowel function (P=0.0003). At study end, 37 (66.0%) patients were satisfied/very satisfied with the new analgesic treatment. Combination therapy had a good safety profile.
Conclusion: OXN-PR and pregabalin were safe and highly effective in a real-world setting of severe neuropathic cancer pain, with a high rate of satisfaction, without interference on bowel function.
Keywords: oxycodone/naloxone, opioids, pregabalin, neuropathic cancer pain, non-small-cell lung cancer, breakthrough cancer pain
Introduction
Severe chronic pain affects most patients with advanced cancer; current guidelines recommend strong around-the-clock opioids as first-line therapy to achieve adequate control of moderate-to-severe chronic pain.1,2
Treatment of cancer-related neuropathic pain includes antidepressants, anticonvulsant agents, topical lidocaine, and oral opioids. Although alleviated by opioids, chronic neuropathic pain seems less responsive than nociceptive pain to opioids, and so these drugs are considered second- or third-line analgesics in this setting.3–5 Given the multifactorial pathogenesis of neuropathic pain, current guidelines recommend combination pharmacotherapy in the management of this heterogeneous and complex condition.1,2 The combination of gabapentin and alpha-lipoic acid has been shown to be effective in neuropathic pain.6 The combination of controlled-release oxycodone and pregabalin was found as an effective long-term option for non-cancer pain treatment, and this combination significantly reduced oxycodone dosages.7
Nevertheless, many cancer patients still do not receive adequate pain control.8,9 The poor gastrointestinal (GI) tolerability of opioids is one of the causes of their limited compliance and inadequate analgesia.10 Opioids exert their analgesic effect primarily interacting with the μ-receptors in the central nervous system; their activation of μ-receptors in the GI tract also causes opioid-induced bowel dysfunction (OIBD), with constipation, abdominal cramps, nausea and vomiting: all these symptoms often interfere with the analgesic efficacy of opioids, causing substantial distress, impairing treatment adherence and quality of life (QoL).10,11
The oral prolonged-release oxycodone/naloxone (OXN-PR) combination in a fixed 1:2 ratio has been shown to be associated with superior GI tolerability.12,13 The powerful μ-opioid receptor antagonist naloxone is added to counteract OIBD by blocking the oxycodone action at opioid receptors locally in the gut; the extensive first-pass hepatic metabolism of naloxone and its low (<3%) systemic bioavailability after oral administration ensure the lack of antagonistic effects on oxycodone central analgesic action. The OXN-PR formulation has been found to be analgesically effective, while improving OIBD and decreasing the use of rescue medications and laxatives.12,14,15 However, a few prospective studies on OXN-PR in cancer patients are available;14,16 moreover, the value of OXN-PR in combination with pregabalin in the treatment of severe neuropathic cancer pain has never been tested.
Our study was aimed at evaluating the efficacy, tolerability, and effect on GI function of OXN-PR in association with pregabalin in patients with lung cancer and severe malignant pain in a real-world clinical setting.
Methods
This 28-day, single-center, prospective observational study was conducted at the Palliative Care and Cancer Pain Service, San Camillo-Forlanini Hospital, Rome, Italy. The study was approved by the Ethics Committee of San Camillo-Forlanini Hospital, and all patients gave written informed consent for the collection and analysis of their anonymous demographic and clinical data.
Design of the study
From January 2013 to May 2014, males and females >18 years of age with non-small-cell lung cancer (NSCLC) referred to our specialist Pain Unit were screened and considered for this study if they had a history of debilitating pain that required continued around-the-clock opioid therapy. Patients previously untreated with pregabalin and with uncontrolled pain despite other opioid treatment, or with side effects contraindicating further dosage increase and requiring switch to another opioid, were also considered.
The inclusion criteria for our study were: 1) presence of severe pain at baseline, defined as average pain intensity (API) score ≥7 on a 0–10 numerical rating scale (NRS; where 0 indicates no pain and 10 the worst imaginable pain) that occurred within the 24 hours preceding the screening visit and requiring WHO step III analgesics (strong opioids) and 2) a clear neuropathic component of pain, caused either from primary or metastatic compression of nervous structures, or from invasive procedures or cancer treatments including surgery, radiation, and chemotherapy. The “definite” neuropathic component was established according to pain description (eg, shooting, burning, tingling sensation with numbness, painful cold, pins and needles, localization to specific dermatomes, or nerve distributions), physical evaluation, and a ≥4 score at the Douleur Neuropathique 4 (DN4) Inventory, a questionnaire used for the diagnosis of neuropathic pain based on pain descriptors and bedside sensory examination.17,18 The inclusion criteria also included Eastern Cooperative Oncology Group Performance Status score <3 and an estimated survival expectancy ≥2 months.
Patients were excluded from the study if changes of chemotherapy occurred, or patients underwent radiotherapy on the lesion that caused the neuropathic pain in 3 weeks before enrollment or throughout the study; diagnosis of neuropathy prior to the diagnosis of cancer, as well as neuropathy considered unrelated to cancer; cognitive impairment or dementia not allowing correct pain assessment; symptomatic cerebral metastases or known psychiatric disease; severe respiratory disease with hypoxemia and/or hypercapnia; moderate or severe liver (total bilirubin ≥1.5 mg/dL) and or renal insufficiency (glomerular filtration rate <30 mL/min); paralytic ileus; history of alcohol and drug abuse; inability to take oral medication; and known hypersensitivity to the study medications.
Regular visits were scheduled at baseline (prior to the start of the treatment, T0), after 14 days (T14) and 28 days (T28), and the end of the observation. Additional visits were possible at all times according to individual patient needs (eg, if patients had inadequate pain control, difficult analgesics titration, and/or adverse events [AEs]).
Study drugs
At the T0 visit, in the absence of contraindications, all patients were prescribed oral OXN-PR (Targin® tablets, Mundipharma Pharmaceuticals, Milan, Italy) and pregabalin (Lyrica® tablets, Pfizer Limited, Sandwich, UK), and were instructed to interrupt other analgesics and/or anticonvulsants. Ongoing acetaminophen and/or adjunctive therapy with steroids were confirmed with no further dose increase for the observation period. Other treatments for any other underlying medical condition were continued unchanged, including laxatives.
The starting OXN-PR dose was determined individually according to the age, health status, previous analgesic therapy, and patient’s needs: in patients naïve to opioids, OXN-PR was started at 5/2.5 or 10/5 mg, twice daily (bid), and the first tablet was administered at 8 pm. In previously opioid-treated patients, starting OXN-PR doses were chosen equivalent to morphine dosage, according to traditional conversion tables. Patients not achieving acceptable pain control were instructed to increase their OXN-PR doses in the following week, with daily increments of 5/2.5–10/5 mg, until patient reported satisfied with pain relief, or emergence of poor tolerability, and/or a maximum daily dose of 60/30 mg (patients naïve to opioids) or 80/40 mg of OXN-PR (patients opioid-pretreated). After 7 days, the study investigator or a palliative care-certified nurse made telephone calls to the patients to ensure that the patients were taking proper doses of OXN-PR. At the subsequent T14 visit, the OXN-PR-titrated dose was confirmed or changed by the visiting pain clinician according to the patients’ needs, side effects, or other inconveniences related to OXN-PR, and the daily OXN-PR dose for the following 2-week period was adjusted accordingly.
The starting pregabalin dose was 25 mg bid, or 75 mg bid if patients were pretreated with gabapentin. If API was still >4 after the first 7-day treatment, and no side effects were reported, patients uptitrated their pregabalin daily dose every 3 days by 50 mg increments, up to a maximum dose of 300 mg daily until the achievement of appropriate pain relief and in the absence of side effects.19
At the T0 visit, oral immediate-release morphine sulfate 10 mg was also prescribed as rescue medication, up to a maximum of three doses per day; patients were also instructed to contact our center in advance of their scheduled control in case of rescue morphine daily dosing more than twice. Sublingual or transmucosal fentanyl as rapid onset opioid was prescribed for the management of episodes of breakthrough cancer pain (BTCP), ie, the transitory exacerbation of pain, with a rapid onset and severe in intensity, with a specific unpredictable or predictable trigger or occurring spontaneously, despite an adequately controlled background pain.2
Assessment
At the T0 visit, demographic and clinical data were recorded, as well as details on pain, ongoing treatments, and constipation. At every visit, API related to the preceding 24 hours was rated on an 11-point NRS. Patients were also required to record the daily number of BTCP, the intensity of this later on an 11-point NRS, as well as the use of rescue analgesics for its treatment.
T0 and T28 evaluation also included the following:
- Interference of pain in the patient’s life, evaluated by a validated Brief Pain Inventory Short Form (BPI-SF) national version;20 BPI-SF 7-item composite pain interference includes general activity, walking ability, normal work, mood, enjoyment of life, sleep, and relations with other people, with a 11-point scale for each item, ranging from 0= no impairment to 10= most severe impairment.
- Symptoms of anxiety and depression, assessed using a validated Hospital Anxiety and Depression Scale (HADS) questionnaire for outpatients: it detect states of anxiety and depression on two 7-item scales, one for anxiety and one for depression, each ranging from 0= absent or normal to 3= most severe impairment (sum score 1–7= normal, 8–10= mildly affected, 11–21= moderately to severely affected).21,22
- Health-related QoL, assessed using the four items on emotional functioning of the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30).23 EORTC QLQ-C30 is a cancer-specific questionnaire composed of both multi-item scales and single-item measures. Patients reported their symptom extent based on the descriptors: 1 (not at all), 2 (a little), 3 (quite a bit), and 4 (very much), thus higher scores indicating a worse level of functioning.24
- Distress due to cancer-related symptoms assessed with the Symptom Distress Scale (SDS):25,26 patients scaled the intensity and frequency of nausea, anorexia, insomnia, bowel pattern, respiration, coughing, fatigue, concentration, appearance, and mood from 1 to 5, with items rated 3 or higher indicating serious distress (a summed score ≥25 indicates moderate distress, scores ≥33 indicate severe distress).27
- Bowel function, in particular symptoms of constipation, which was considered as clinically significant if patients reported less than three complete spontaneous bowel movements, with difficulty passing stools despite laxatives and/or appropriate dietary modifications. Bowel function in the last 7 days was also evaluated by the Bowel Function Index (BFI): scores range from 0 (free from symptoms) to 100 (most severe symptoms); in patients with chronic pain, a BFI value of 29 is set as upper normal limit.28
At the T28 visit, patients’ satisfaction with the efficacy and tolerability of the new analgesic treatment was rated as very satisfied, satisfied, moderately satisfied, or dissatisfied.
Safety
At each time point, any new AE that occurred or worsened in intensity and/or frequency after the intake of OXN-PR and pregabalin was recorded; the potential correlation between the AE and the new antalgic treatment was judged by the pain therapist. This safety evaluation considered only AEs of severe intensity (ie, those persistent despite treatment and requiring discontinuation of the treatment) and/ or moderate AEs (ie, those requiring treatment and/or not permitting a dose escalation of the treatment, or requiring its down-tapering).
Statistical analysis
As in other studies assessing analgesic efficacy in cancer patients, the primary endpoint of the trial was the proportion of patients who achieved a substantial reduction in their pain intensity after the new analgesic combination: “Responders” were those patients who achieved at T28 a reduction of API ≥30% from baseline.29–31
Secondary endpoints were: mean percentage change in API from baseline; the percentage of patients achieving an API <5, as well as the percentage reporting satisfaction with pain relief; changes in the number and intensity of BTCP episodes from baseline; changes in neuropathic pain from baseline (DN4 evaluation); and interference of pain in the patient’s life (BPI), distress (SDS), anxiety and depression (HADS), QoL (EORTC QLQ-C30 evaluation), and bowel function (BFI).
According to the given definition, based on a Fleming design with 80% power and 5% type 1 error, the study design required 39 patients to test the null hypothesis that the true confirmed response rate was at most 50%, versus the alternative hypothesis that it was >70%. Considering the short duration planned for this observation, to allow for dropouts and incomplete data (~25%), at least 49 patients were required. Missing data were treated with the “last observation carried forward” method.
Data are reported as mean ± standard deviation or median and range. Changes over time in categorical variables were compared using the Cochran’s Q test, and differences between pairs of continuous variables were evaluated by Student’s t-test or Wilcoxon test. Continuous variables over time were assessed by analysis of variance or Kruskal–Wallis analysis. Normality distribution of continuous variables was assessed by the Shapiro–Wilk test. A P-value <0.05 was considered statistically significant (STATISTICA software, version 8.0, StatSoft® Inc., Tulsa, OK, USA).
Results
From January 2013 to May 2014, 60 patients with advanced NSCLC and severe pain despite analgesic treatment were screened: two patients were not included (terminal illness; cognitive limitation), two others were excluded (logistic impediments to completing the 4-week observation; no informed consent). The remaining 56 patients (93.3% of the screened population) were included in the final analysis (mean age 64±10, 77% males). Patient flow throughout the study is shown in Figure 1. Their demographic and baseline clinical characteristics are shown in Table 1. All the patients were at tumor, node, metastasis classification (TNM, seventh edition) stage IV; mean Karnofsky Performance Scale Index was 66±10. In more than two-thirds of the patients, bone metastases were present. Chemotherapy was the main cancer treatment in 38/56 (67.9%) of the patients, and 30/56 (53.6%) received also radiation therapy.
Before enrollment, 45 patients (80.4%) were taking nonsteroidal anti-inflammatory drugs, and 36 (64.2%) were already on opioids (WHO step III drugs in 50% of patients). At baseline, all the patients were taking some adjuvant therapy; the majority of the patients were taking alpha-lipoic acid, two-thirds were treated with steroids, one-third with bisphosphonates, and one-fifth were on anticonvulsants (gabapentin in all cases).
According to the reported API value at baseline (median 8, range 7–10), the enrolled population was suffering from very severe pain. At enrollment, pain duration was >30 days in 29 (51.8%) patients.
At enrollment, the majority of the patients reported BTCP episodes (n=51, 91.1%; median, three episodes daily); this was of severe intensity (mean NRS, 8.3±2.7). All the patients completed the 28-day study observation.
The mean OXN-PR starting dose was 22.1±8.9 mg daily (range 10–60 mg). Subsequently, OXN-PR daily dose increased to 36.3+15.7 mg at the T28 visit (P<0.0001).
Mean pregabalin starting dose was 70.5±39.6 mg daily (range 25–150); at the T28 visit, all the patients were still on pregabalin, with a mean daily dose slightly increased versus baseline (115.0±69.6 mg, range 25–300 mg; P<0.0001).
Analgesic response
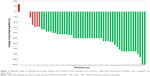
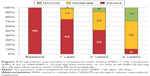
A substantial decrease in reported pain intensity was documented with the OXN-PR and pregabalin combination (API at T28=4.2±1.9, P<0.0001 vs baseline); a significant reduction in pain severity was already reported after 14 days (Figure 2). Mean pain intensity decrease at T28 was 47.6%±24.3%, and the “waterfall” graph in Figure 3 shows the individual changes of pain intensity from baseline to T28. At T28, there were 46 (82.1%) responders (ie, those with a reduction in daily pain intensity ≥30% of the corresponding baseline value). Among the remaining ten (17.9%) patients with unsatisfactory analgesic response at T28 visit, six patients (10.7%) were still complaining of severe pain (API ≥7). On the contrary, 16 patients (28.5%) reported a complete or near-complete analgesic benefit (API 0–3) at T28 (Figure 4). Likewise, the DN4 score was markedly reduced at T28 visit (4.5+1.8 vs 6.75+0.86, P<0.001).
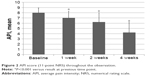  | Figure 2 API score (11-point NRS) throughout the observation. |
At the end of the observation, fewer patients still reported episodes of BTCP (n=39, 69.6%; P<0.005 vs baseline). The number of daily episodes also decreased at T28 (2.1±2.3; median 2, range 2–12; P=0.001), also of reduced severity (NRS 5.7±3.9, P<0.001 vs baseline).
Other efficacy results
At study end, all secondary efficacy measures showed substantial improvement. Daily need of additional acetaminophen decreased from 86.8% to 40.4% at T28 (P<0.001). Pain-related functional impairment also declined (BPI-SF composite pain interference score: from 6.9±1.6 to 5.5±1.8; P=0.0002). All individual domain scores except quality of sleep decreased from baseline to T28, suggesting less interference of pain in daily life (Table 2).
In agreement with the favorable BPI-SF finding, health-related QoL substantially improved at T28 (P<0.001, Table 2); conversely, distress due to cancer-related symptoms decreased substantially over the observation (Table 2): both physical and emotional dimensions of SDS scales were significantly reduced (P<0.0001).
After the new analgesic treatment, a substantial improvement in anxiety and depression symptoms was also recorded, as reflected by the significant decrease of HADS subscales scores (P<0.05 for both) (Table 2).
Tolerability and safety
Although at baseline only one-third (35.7%) of the patients reported constipation (Table 1), almost all (83.3%,) showed abnormal BFI values (ie, >29); indeed, the median baseline BFI value recorded at T0 (48) indicates that half of the patients suffered moderate-to severe bowel dysfunction at baseline. After OXN-PR and pregabalin, of relevance, none reported subjective worsening of their constipation symptoms, or constipation of new occurrence. The number of patients still complaining of constipation at the end of the study nearly reduced to half (n=13, 23.2%; P<0.01 in Cochran’s Q test). In fact, a significant reduction in the BFI value was found after the administration of OXN-PR and pregabalin, thus indicating an improvement in bowel function (mean value at T28, 28.9±21.7, P<0.001 vs baseline).
At the end of the study, 37 (66.0%) patients rated the new analgesic treatment positively; 14 (25.0%) and 23 (41.0%) said they were either very satisfied or satisfied, respectively. Only four patients (7.1%) rated themselves as dissatisfied after the administration of the OXN-PR and pregabalin combination.
Overall, the OXN-PR and pregabalin combination therapy was well tolerated in the 28-day observation. Side effects were documented in 26 patients. The most common AEs are summarized in Table 3. No severe AEs leading to premature discontinuation were recorded. Most AEs were mild, without new or unexpected safety signals. The most frequent treatment-related AEs were somnolence, confusion, asthenia, loss of appetite, and nausea.
Discussion
In cancer patients, pain is often associated with exacerbation of other symptoms, and affects mood, job performance, personal relationships, and the overall QoL.32 In the last two decades, despite the improvements in quality of pharmacologic treatment, one-third of cancer patients are still not receiving adequate pain management.9 The integration of early palliative intervention with anticancer treatment can reduce anxiety and depression, improving the QoL and prolonging survival.33 According to a recent statement of the American Society of Clinical Oncology, “combined standard oncology care and palliative care should be considered early in the course of illness for any patient with metastatic cancer and/or high symptom burden”.34
Pain may be the first sign of lung cancer, and its prevalence in patients with lung cancer is one of the highest (>85%) among different cancer types.8 Extremely few data, however, are available on pain management in patients with lung cancer; in a small trial conducted in patients with NSCLC, subjects randomly assigned to an oral pain treatment protocol encompassing recommendations from existing cancer pain guidelines performed significantly better than patients managed according to physician preference.35
A neuropathic pain component of pain is present in 30% to 50% of patients with lung cancer.36–38 Chemotherapy or radiotherapy, combined with general comorbidities and impaired functional status, makes neuropathic pain difficult to correct, and often adjuvants are added to target specific pathways of neuropathic pain.39 Oxycodone plus pregabalin has been found to be effective in controlling neuropathic pain both in non-cancer and cancer patients.7,40 However, response to opioids is often inadequate, requiring higher dosages;19 and side effects of opioids are common: OIBD, in particular constipation, is common and persists, causing considerable distress and reduced QoL.11,41
The oral fixed-dose OXN-PR combination has been shown to provide analgesic efficacy while improving OIBD in cancer patients.14–16,42 A small, open-label study showed relevant improvement in pain and bowel function after OXN-PR.16 In a randomized controlled trial comparing efficacy and safety of oxycodone PR and OXN-PR in opioid-pretreated patients with controlled pain and constipation at baseline, the switch to OXN was associated with a similar analgesic effect compared to oxycodone PR, however, with a clinically relevant improvement in bowel function.14 A retrospective study in 206 patients with uncontrolled pain showed OXN to be highly effective and well tolerated in both opioid-naïve and -pretreated patients, as well as in younger and older patients, without adverse effects on bowel function;42 patients previously treated with OXY were not included in that study. Kang et al reported pain exacerbation and opioid withdrawal symptoms in a patient with gastric cancer and portal vein thrombosis after receiving OXN-PR; hepatic and renal function data were not described in the case report.43 In a recent study comparing OXN-PR and oxycodone-PR in cancer patients naïve to strong opioids, the analgesic efficacy was found to be comparable, with an overall incidence of drug-related AEs remarkably lower after OXN-PR: nausea and vomiting were significantly less frequent, with greater improvement in QoL following OXN-PR.15
Different from the aforementioned studies, our study is the first prospective clinical trial to evaluate the efficacy and safety of OXN-PR and pregabalin in cancer patients with neuropathic pain. The target population had severe pain despite other non-opioid and opioid analgesic treatment. The majority of patients (82%) achieved the primary endpoint after 4 weeks of OXN-PR and pregabalin treatment. Pain relief was achieved even in patients previously treated with WHO step III opioids; the severity of neuropathic pain also declined after 28 days, as indicated by the significantly reduced DN4 values. All secondary efficacy measures improved substantially, with less interference of pain in the patient’s life, less distress due to cancer-related symptoms, and improved QoL. The reduced bowel discomfort likely improved the adherence to the new treatment, contributing to the observed superior analgesic effects of the new treatment in comparison with previous painkillers. More recently, in a large randomized trial, OXN-PR was associated with a significantly better analgesic efficacy, lower risk of OIBD, and superior tolerability compared with oxycodone or morphine.44 Of note, ultra-low dosages of naloxone could enhance, rather than attenuate, the analgesic effects of oxycodone within the central nervous system.45,46 The improved QoL and GI tolerability of OXN-PR explain its lower cost-utility estimates compared with oxycodone.47
In the present study, the OXN-PR and pregabalin combination was well tolerated, and there were no serious drug-related AEs. Of note, central nervous system side effects, and in particular dizziness and drowsiness, were limited. The observed improvement in QoL and patient’s satisfaction is in agreement with previous results, showing that attenuation of neuropathic pain after opioids improves mood and sleep.48,49
This study had several limitations, including the open-label observational design, short treatment duration, small sample size, and lack of a control group. However, the results of the present study provide a solid basis for the design of a larger investigation to further assess the efficacy and tolerability of the OXN-PR and pregabalin combination for the management of severe neuropathic pain in patients with lung cancer.
Conclusion
The opioid agonist–antagonist OXN-PR combination in conjunction with pregabalin effectively controlled severe neuropathic pain in patients with lung cancer. This drug combination did not worsen the bowel function, and also resulted in a significant improvement in QoL and patient’s satisfaction. Thus, it could represent a valuable option in daily clinical practice for the management of severe neuropathic cancer pain.
Acknowledgments
The authors thank Ray Hill, an independent medical writer, who performed language editing in English and journal styling prior to submission on behalf of Health Publishing & Services Srl. This assistance was funded by Mundipharma Pharmaceuticals.
Disclosure
The authors report no conflicts of interest in this work.
References
Ripamonti CI, Santini D, Maranzano E, Berti M, Roila F. Management of cancer pain: ESMO Clinical Practice Guidelines. Ann Oncol. 2012;23(Suppl 7):vii139–vii154. | ||
Caraceni A, Hanks G, Kaasa S, et al. Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol. 2012;13(2):e58–e68. | ||
Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17(9):e1113–e1188. | ||
Dworkin RH, O’Connor AB, Kent J, et al. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain. 2013;154(11):2249–2261. | ||
Moulin DE, Boulanger A, Clark AJ, et al. Pharmacological management of chronic neuropathic pain: revised consensus statement from the Canadian Pain Society. Pain Res Manag. 2014;19(6):328–335. | ||
Chaparro LE, Wiffen PJ, Moore RA, Gilron I. Combination pharmacotherapy for the treatment of neuropathic pain in adults. Cochrane Database Syst Rev. 2012;7:CD008943. | ||
Gatti A, Longo G, Sabato E, Sabato AF. Long-term controlled-release oxycodone and pregabalin in the treatment of non-cancer pain: an observational study. Eur Neurol. 2011;65(6):317–322. | ||
Breivik H, Cherny N, Collett B, et al. Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol. 2009;20(8):1420–1433. | ||
Greco MT, Roberto A, Corli O, et al. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. 2014;32(36):4149–4154. | ||
Candy B, Jones L, Goodman ML, Drake R, Tookman A. Laxatives or methylnaltrexone for the management of constipation in palliative care patients. Cochrane Database Syst Rev. 2011(1):CD003448. | ||
Camilleri M. Opioid-induced constipation: challenges and therapeutic opportunities. Am J Gastroenterol. 2011;106(5):835–842. quiz 843. | ||
Mercadante S, Giarratano A. Combined oral prolonged-release oxycodone and naloxone in chronic pain management. Expert Opin Investig Drugs. 2013;22(1):161–166. | ||
Reimer K, Hopp M, Zenz M, et al. Meeting the challenges of opioid-induced constipation in chronic pain management – a novel approach. Pharmacology. 2009;83(1):10–17. | ||
Ahmedzai SH, Nauck F, Bar-Sela G, Bosse B, Leyendecker P, Hopp M. A randomized, double-blind, active-controlled, double-dummy, parallel-group study to determine the safety and efficacy of oxycodone/naloxone prolonged-release tablets in patients with moderate/severe, chronic cancer pain. Palliat Med. 2012;26(1):50–60. | ||
Lazzari M, Greco MT, Marcassa C, Finocchi S, Caldarulo C, Corli O. Efficacy and tolerability of oral oxycodone and oxycodone/naloxone combination in opioid-naive cancer patients: a propensity analysis. Drug Des Devel Ther. 2015;9:5863–5872. | ||
Clemens KE, Quednau I, Klaschik E. Bowel function during pain therapy with oxycodone/naloxone prolonged-release tablets in patients with advanced cancer. Int J Clin Pract. 2011;65(4):472–478. | ||
Bouhassira D, Attal N. Diagnosis and assessment of neuropathic pain: the saga of clinical tools. Pain. 2011;152(3 Suppl):S74–S83. | ||
Haanpaa M, Attal N, Backonja M, et al. NeuPSIG guidelines on neuropathic pain assessment. Pain. 2011;152(1):14–27. | ||
Raptis E, Vadalouca A, Stavropoulou E, Argyra E, Melemeni A, Siafaka I. Pregabalin vs opioids for the treatment of neuropathic cancer pain: a prospective, head-to-head, randomized, open-label study. Pain Pract. 2014;14(1):32–42. | ||
Bonezzi C, Nava A, Barbieri M, et al. Validazione della versione italiana del Brief Pain Inventory nei pazienti con dolore cronico [Validation of an Italian version of the Brief Pain Inventory in patients with chronic pain]. Minerva Anestesiol. 2002;68(7–8):607–611. Italian. | ||
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. | ||
Costantini M, Musso M, Viterbori P, et al. Detecting psychological distress in cancer patients: validity of the Italian version of the Hospital Anxiety and Depression Scale. Support Care Cancer. 1999;7(3):121–127. | ||
American Thoracic Society. European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30). 1999. Available from: http://qol.thoracic.org/sections/instruments/pt/pages/sds.html. Accessed October 14, 2015. | ||
Montazeri A, Milroy R, Hole D, McEwen J, Gillis CR. Anxiety and depression in patients with lung cancer before and after diagnosis: findings from a population in Glasgow, Scotland. J Epidemiol Community Health. 1998;52(3):203–204. | ||
McCorkle R, Young K. Development of a symptom distress scale. Cancer Nurs. 1978;1(5):373–378. | ||
Tamburini M. Health-related quality of life measures in cancer. Ann Oncol. 2001;12(Suppl 3):S7–S10. | ||
American Thoracic Society. Symptom Distress Scale. 1999. Available from: http://qol.thoracic.org/sections/instruments/pt/pages/sds.html. Accessed October 14, 2015. | ||
Rentz AM, Yu R, Muller-Lissner S, Leyendecker P. Validation of the Bowel Function Index to detect clinically meaningful changes in opioid-induced constipation. J Med Econ. 2009;12(4):371–383. | ||
Bandieri E, Romero M, Ripamonti CI, et al. Randomized trial of low-dose morphine versus weak opioids in moderate cancer pain. J Clin Oncol. 2016;34(5):436–442. | ||
Corli O, Roberto A, Greco MT, Montanari M. Assessing the response to opioids in cancer patients: a methodological proposal and the results. Support Care Cancer. 2015;23(7):1867–1873. | ||
Farrar JT, Portenoy RK, Berlin JA, Kinman JL, Strom BL. Defining the clinically important difference in pain outcome measures. Pain. 2000;88(3):287–294. | ||
Laird BJ, Scott AC, Colvin LA, et al. Pain, depression, and fatigue as a symptom cluster in advanced cancer. J Pain Symptom Manage. 2011;42(1):1–11. | ||
Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–742. | ||
Smith TJ, Temin S, Alesi ER, et al. American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol. 2012;30(8):880–887. | ||
Cleeland CS, Portenoy RK, Rue M, et al. Does an oral analgesic protocol improve pain control for patients with cancer? An intergroup study coordinated by the Eastern Cooperative Oncology Group. Ann Oncol. 2005;16(6):972–980. | ||
Bennett MI, Rayment C, Hjermstad M, Aass N, Caraceni A, Kaasa S. Prevalence and aetiology of neuropathic pain in cancer patients: a systematic review. Pain. 2012;153(2):359–365. | ||
Garcia de Paredes ML, del Moral Gonzalez F, Martinez del Prado P, et al. First evidence of oncologic neuropathic pain prevalence after screening 8615 cancer patients. Results of the On study. Ann Oncol. 2011;22(4):924–930. | ||
Bennett DL. Informed drug choices for neuropathic pain. Lancet Neurol. 2015;14(2):129–130. | ||
Mañas A, Ciria JP, Fernández MC, et al. Post hoc analysis of pregabalin vs non-pregabalin treatment in patients with cancer-related neuropathic pain: better pain relief, sleep and physical health. Clin Transl Oncol. 2011;13(9):656–663. | ||
Garassino MC, Piva S, La Verde N, et al. Randomised phase II trial (NCT00637975) evaluating activity and toxicity of two different escalating strategies for pregabalin and oxycodone combination therapy for neuropathic pain in cancer patients. PLoS One. 2013;8(4):e59981. | ||
Pappagallo M. Incidence, prevalence, and management of opioid bowel dysfunction. Am J Surg. 2001;182(5A Suppl):11S–18S. | ||
Cuomo A, Russo G, Esposito G, Forte CA, Connola M, Marcassa C. Efficacy and gastrointestinal tolerability of oral oxycodone/naloxone combination for chronic pain in outpatients with cancer: an observational study. Am J Hosp Palliat Care. 2014;31(8):867–876. | ||
Kang JH, Lee GW, Shin SH, Bruera E. Opioid withdrawal syndrome after treatment with low-dose extended-release oxycodone and naloxone in a gastric cancer patient with portal vein thrombosis. J Pain Symptom Manage. 2013;46(2):e15–e17. | ||
Ueberall MA, Mueller-Schwefe GH. Safety and efficacy of oxycodone/naloxone vs oxycodone vs morphine for the treatment of chronic low back pain: results of a 12 week prospective, randomized, open-label blinded endpoint streamlined study with prolonged-release preparations. Curr Med Res Opin. 2015;31(7):1413–1429. | ||
Burns LH, Wang H-Y. Ultra-low-dose naloxone or naltrexone to improve opioid analgesia: the history, the mystery and a novel approach. Clin Med Insights Ther. 2010;2:857. | ||
Wang HY, Friedman E, Olmstead MC, Burns LH. Ultra-low-dose naloxone suppresses opioid tolerance, dependence and associated changes in mu opioid receptor-G protein coupling and Gβγ signaling. Neuroscience. 2005;135(1):247–261. | ||
Dunlop W, Uhl R, Khan I, Taylor A, Barton G. Quality of life benefits and cost impact of prolonged release oxycodone/naloxone versus prolonged release oxycodone in patients with moderate-to-severe non-malignant pain and opioid-induced constipation: a UK cost-utility analysis. J Med Econ. 2012;15(3):564–575. | ||
Lazzari M, Sabato AF, Caldarulo C, et al. Effectiveness and tolerability of low-dose oral oxycodone/naloxone added to anticonvulsant therapy for noncancer neuropathic pain: an observational analysis. Curr Med Res Opin. 2014;30(4):555–564. | ||
O’Connor AB. Neuropathic pain: quality-of-life impact, costs and cost effectiveness of therapy. Pharmacoeconomics. 2009;27(2):95–112. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.