Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 14
An Open-Label, Randomized, Double-Arm Clinical Trial to Compare the Effectiveness and Safety of Super Bioavailable Itraconazole Capsules and Itraconazole Capsules in the Management of Dermatophytosis in India
Authors Shenoy M, Dhoot D , Mahajan H, Barkate H
Received 26 June 2021
Accepted for publication 5 August 2021
Published 27 September 2021 Volume 2021:14 Pages 1367—1376
DOI https://doi.org/10.2147/CCID.S326642
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Manjunath Shenoy,1,2 Dhiraj Dhoot,3 Harshal Mahajan,3 Hanmant Barkate3
1Department of Dermatology, Yenepoya Medical College, Deralakatte, Mangalore, India; 2Omega Hospital, Mangalore, Karnataka, India; 3Global Medical Affairs, Glenmark Pharmaceuticals Ltd, Mumbai, Maharashtra, India
Correspondence: Dhiraj Dhoot
Global Medical Affairs, Glenmark Pharmaceuticals Ltd, B D Sawant Marg, Andheri (E), Mumbai, Maharashtra, 400099, India
Tel +91 9619811219
Email [email protected]
Purpose: A new oral formulation of itraconazole, called super bioavailable itraconazole (SBITZ), has been launched in India, exhibiting greater bioavailability than conventional itraconazole (CITZ). No clinical studies on its effectiveness and safety in dermatophytosis in comparison with CITZ have been conducted in India. Hence, the aim of this clinical study was to compare the effectiveness and safety of SBITZ capsules and CITZ capsules in dermatophytosis.
Patients and Methods: This was an open-label, randomized, double-arm clinical study in which 70 patients (≥ 18 years of age) of either gender and diagnosed with tinea cruris, tinea corporis, and/or tinea faciei were included. The study was divided into two parts, the first part comprising a treatment period of 4 weeks and the second part an observation period for recurrence, comprised of another 4 weeks, thus making an entire study duration of 8 weeks.
Results: Of the 70 patients enrolled in this study, 59 (33 patients in the CITZ group and 26 patients in the SBITZ group) were included in the final analysis. In both groups, most patients were diagnosed with tinea cruris et corporis, with five or more lesions. At week 4, 11 patients (33.33%) and 17 patients (65.38%) had achieved complete cure (p< 0.05), whereas 22 patients (66.67%) and 22 patients (84.61%) had achieved mycological cure (p=0.14), in the CITZ and SBITZ groups, respectively. During the observation period, recurrence was seen in 1/11 and 4/17 completely cured patients in the CITZ and SBITZ groups, respectively (p=0.15). A significant difference was noted in resolution of symptoms as well as lesions of dermatophytosis in the SBITZ group (p< 0.05). Both treatments were found to be safe and well tolerated.
Conclusion: In the light of real-world evidence on effectiveness and safety, SBITZ should be considered as a potent therapeutic choice to effectively control the current menace of dermatophytosis in India.
Keywords: dermatophytosis, super bioavailable itraconazole, conventional itraconazole, India
Introduction
In recent times, dermatologists across India have been deluged with cases of dermatophytosis presenting with multiple-site lesions, extensive skin lesions, unusually large lesions, involvement of uncommon sites such as the face and genitals, ring-within-ring lesions, and other corticosteroid-modified lesions, making its diagnosis and treatment challenge. In addition, chronic and frequent recurrences of the disease have plagued patients, in contrast to many other dermatological conditions.1 Because of this changing face of dermatophytosis, standard treatment recommendations from the western and Indian literature may not adequately address the current scenario.2 Hence, dermatologists in India are relying on multiple experience-based treatment strategies, such as longer duration of treatment, using higher doses of antifungals, and using other therapies that have not been approved for the routine management of dermatophytosis.2,3
Itraconazole (ITZ) is a systemic antifungal drug used in the treatment of dermatophytosis owing to its excellent potency compared to other systemic antifungal drugs.4 ITZ is an orally available triazole antifungal drug and is considered to be a first-line drug for the treatment of tinea corporis and cruris.5,6
However, because of its inherent pharmacokinetic characteristics, ITZ shows unpredictable absorption patterns. Being a weak base molecule, it requires an acidic pH for its dissolution; therefore, it is recommended to be taken with acidic beverages. Since its absorption is lower in the fasting state, ITZ has to be taken with meals, especially fatty meals, to achieve optimal absorption and bioavailability. Concomitant use of gastric acid-lowering agents such as proton pump inhibitors (PPIs) reduces its absorption, leading to a further reduction in bioavailability.7 In a real-world setting, it is difficult to ensure all of these factors to obtain the optimum bioavailability of ITZ.
Moreover, even under ideal conditions, the optimal level of gastric acid secretion cannot be guaranteed as it is dependent on various factors, such as the circadian rhythm, stress levels, and eating and sleeping patterns.8 Because of these factors, the bioavailability of conventional itraconazole (CITZ) is only up to 55%, and this, too, fluctuates widely depending on the amount of gastric acid secretion, which leads to wide interpatient variability7,9 and variations in the clinical response in patients. In this scenario, the intrinsic pharmacokinetic properties of ITZ may play a major role in its increased dose and duration in the treatment of dermatophytosis.
Recently, a new oral formulation of ITZ, called super bioavailable itraconazole (SBITZ), was launched in 2020 in India as a 50 mg capsule, which is bioequivalent to CITZ 100 mg. It has been approved in many countries for invasive mycoses, including aspergillosis and candidiasis.10 It contains a solid dispersion of ITZ in a uniform non-pellet formulation containing a pH-dependent polymeric matrix, hydroxypropyl methylcellulose phthalate (HPMCP), which enhances its dissolution and intestinal absorption,11 giving it greater bioavailability than CITZ.
SBITZ has been well studied in other indications10 but clinical data on its use in superficial fungal infections are lacking. Currently, there are no Indian clinical trials related to its effectiveness and safety in dermatophytosis, in comparison with CITZ. Hence, the present clinical trial was planned to evaluate the effectiveness and safety of SBITZ in comparison with CITZ in patients with dermatophytosis.
Patients and Methods
Study Participants
A total of 70 adult patients (≥18 years of age) of either gender attending the dermatology outpatients department at a tertiary hospital in Mangalore, India, during November 2020 to March 2021, and diagnosed with tinea cruris and/or tinea corporis and/or tinea faciei, were included in the study. Patients with any significant medical illness, such as diabetes, cardiac disease, or immunocompromised conditions, that would have affected clinical outcomes, and female patients who were pregnant or lactating, were excluded from the study according to the investigators’ discretion.
The study was conducted in compliance with the protocol approved by the Omega Ethics Committee, Mangalore. Written informed consent was obtained from all patients prior to their participation in the study. This study was registered with the Clinical Trial Registry – India as CTRI/2020/10/028565. This clinical trial was performed in accordance with Good Clinical Practices and the Declaration of Helsinki 1996.
Study Design and Treatment
This was an open-label, randomized, double-arm clinical trial, conducted to compare the effectiveness and safety of SBITZ capsules and CITZ capsules in the management of tinea corporis, tinea cruris, and tinea faciei. Eligible patients were randomized into two groups to receive either itraconazole, 100 mg twice a day (CITZ), or super bioavailable itraconazole, 50 mg twice a day (SBITZ), at the discretion of the treating physician and at approved dosages. Both drugs were supplied by Glenmark Pharmaceuticals Ltd, India. Patients were not allowed to take any other antifungal medications during the study period, as per the protocol. Both groups received a topical emollient containing light liquid paraffin and white soft paraffin.
Eligible patients’ demographics and baseline clinical characteristics, including site of lesion, extent of lesion, duration of current illness, clinical symptoms and signs score, treatment history, and number of previous episodes, were recorded at baseline (day 0). All patients’ diagnoses were confirmed on direct microscopy under 10% potassium hydroxide examination (KOH mount), which was repeated at the end of the treatment period (4 weeks). Upon confirmation by KOH mount, on visit 2 (day 1), all of the patients were either prescribed CITZ or SBITZ. The study was divided into two parts, the first part comprising the treatment period, of 4 weeks, and the second part an observation period comprising another 4 weeks, thus making an entire study duration of 8 weeks. During the treatment period, patients were followed up as per routine protocol, and clinical assessment data were collected on visit 2 (day 1), visit 3 (day 15±2), and visit 4 (day 29±2). Following this treatment period, patients with complete cure were not prescribed any antifungal medication, while the rest of the patients with improvement were allowed to take antifungal medication at the discretion of the treating physician. All the patients with complete cure were contacted by telephone regarding any recurrence of disease at day 57±2. The complete study design is shown in Figure 1.
 |
Figure 1 Study design. |
The patients were categorized as naïve, chronic, or recurrent, depending upon the history of clinical presentation. Naïve cases were defined as patients who had not been previously exposed to a particular infection with a given disease or treatment for that disease. Chronic cases were patients who had suffered from the disease for more than 6 months to 1 year, with or without recurrence, in spite of being adequately treated. Recurrent cases were defined as patients who encountered reoccurrence of the disease (lesions) within a few weeks (<6 weeks) after completion of the treatment.1
Outcome Assessments
The primary endpoint of the study was the comparison of the percentage of patients achieving a complete cure (clinical cure plus mycological cure) at the end of treatment period from baseline. Clinical cure was defined as a combination of the absence of any signs and symptoms (total symptom score of 0) and the absence of the extent of lesions in terms of the body surface area (BSA). The total symptom score (TSS) comprised four symptoms: scaling, pruritus, erythema, margin continuity and elevation of the representative lesion. Each symptom was scored on a four-point Likert scale of 0–3, where 0 denotes the absence of a symptom and 3 denotes the maximum intensity of an individual symptom. The TSS was obtained by the summation of the individual signs and symptoms score at each time point (range 0–12). The extent of lesions in terms of BSA ranged from 0 to 3, where 0 corresponds to the absence of lesions, 1 to BSA involvement of <3%, 2 to BSA involvement of 3–10%, and 3 corresponds to BSA involvement of >10%. In addition, the investigator’s global assessment of effectiveness and safety (IGA) was graded on a four-point scale (0=poor, 1=satisfactory, 2=good, and 3=excellent) at visits 2, 3, and 4.
KOH Mount
Mycological cure was defined as a negative report on the KOH mount at week 4. A scraping of the skin was directly collected on to the slide. Potassium hydroxide 10% was added to the material, covered by a coverslip of fragile glass, and gently preheated before examination. Microscopic examination was performed with a direct light microscope to detect fungal spores or hyphae. The initial examination was carried out at low-power magnification (×10) and later at higher magnification (×40).
The secondary outcome measures included percentage change in mean TSS, BSA, and IGA from baseline to subsequent visits. The safety assessment was based on spontaneous adverse events (AEs) reported by patients and clinicians throughout the study period (8 weeks).
Analysis Set
All of the effectiveness analyses were performed on the full analysis set (FAS) (ie, those patients who received at least one dose of medication and completed at least one post-baseline follow-up visit). Safety analysis was performed on all patients included in the FAS.
Statistical Analysis
Baseline demographic and clinical characteristics were presented as numbers and percentages, and as means with standard deviations (SDs). The primary and secondary effectiveness endpoints were summarized using descriptive statistics; frequencies were reported for categorical variables and means with SD. The difference in the proportion of patients with total signs and symptom scores (based on improvement criteria) was analyzed using the chi-squared test with a significance level of 0.05. The two groups were compared by Fisher’s exact test. All statistical analyses were performed using SPSS version 15 (SPSS, Chicago, IL, USA).
Results
Baseline Clinical Characteristics
Of the 70 patients enrolled in this study, 59 were included in the FAS. There were 33 patients in the CITZ group and 26 patients in the SBITZ group. A male predominance was seen in both groups, at 75.8% and 57.7% in the CITZ and SBITZ groups, respectively, with a mean±SD age of 37.11±10.93 vs 34.60±11.38 years, respectively (Table 1). All of the baseline characteristics are presented in Table 1. The patient distribution was homogeneous in both groups. In both groups, most patients were diagnosed with tinea cruris et corporis, with at least five lesions. About 38% of the patients in both groups had already obtained treatment from the chemist, and topical steroid usage was seen in 24.2% and 23.1% of the patients in the CITZ and SBITZ groups, respectively.
 |
Table 1 Baseline Demographic Characteristics |
Treatment Response
Effectiveness
At week 4, 11 patients (33.33%) (five patients with chronic, six patients with recurrent, and no patients with naïve dermatophytosis) and 17 patients (65.38%) (nine patients with chronic, five patients with recurrent, and three patients with naïve dermatophytosis) achieved complete cure, whereas 22 patients (66.67%) and 22 patients (84.61%) achieved mycological cure in the CITZ and SBITZ groups, respectively. Clinical improvement in patients in the SBITZ and CITZ groups is shown in Figures 2 and 3 respectively. There was a statistically significant difference between the two groups in completely cured patients (p<0.05), whereas in mycologically cleared patients, no statistically significant difference was found (p=0.14). During the observation period, recurrence was seen in one out of 11 and four out of 17 completely cured patients in the CITZ and SBITZ groups, respectively (p=0.15). On subgroup analysis, similar results were obtained for chronic dermatophytosis: in the CITZ group, five out of 19 patients (26.31%) and in the SBITZ group nine out of 15 patients (60%) achieved complete cure (p=0.08), whereas 11 (57.89%) and 14 (93.33%) patients, respectively, achieved mycological cure (p<0.05). Recurrence was seen in these groups of patients only, as shown in Table 2. The number of patients with improvement, for recurrent and naïve patients, is also shown in Table 2.
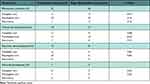 |
Table 2 Effectiveness Evaluation in Chronic, Recurrent and Naïve Patients |
 |
Figure 2 Clinical improvement in SBITZ group: (A) before SBITZ and (B) after SBITZ treatment; (C) before SBITZ and (D) after SBITZ treatment. |
 |
Figure 3 Clinical improvement in CITZ group: (A) before CITZ and (B) after CITZ treatment. |
Improvement in Mean Scores
At week 2, the mean TSS of 9.73±1.59 was reduced to 4.06±1.77 (58.2% reduction) in the CITZ group, while it was reduced from 9.35±1.32 to 3.15±1.35 (66.3% reduction) in the SBITZ group. At week 4, a further reduction was seen in mean TSS to 1.58±1.90 (83.7% reduction) and 0.65±1.09 (93.0% reduction) in the CITZ and SBITZ groups, respectively. Both treatments were statistically significant in reducing TSS at both visits (p<0.05) from baseline. On intergroup comparison, statistically significant differences were seen at both visits (p<0.05), as noted in Table 3 and Figure 4.
 |
Table 3 Mean Scores at Baseline, Week 2, and Week 4 in Both Treatment Groups |
 |
Figure 4 Percent reduction in mean scores. |
Significant lesion clearance was also seen in both groups at both visits. At week 2, the mean BSA score of 2.23±0.55 was reduced to 1.27±0.63 (43.0% reduction) in the CITZ group, whereas it was reduced from 1.94±0.68 to 0.88±0.59 (54.6% reduction) in the SBITZ group. At week 4, the mean BSA score further reduced to 0.48±0.63 (78.4% reduction) in the CITZ group, compared to 0.15±0.37 (92.2% reduction) in the SBITZ group. There were statistically significant differences in intergroup as well as intragroup comparisons (p<0.05). Similar results were obtained for mean IGA score (Table 3).
Adverse Events
A total of five AEs were reported from five patients: four in the CITZ group and one in the SBITZ group. Three patients in the CITZ group and one patient in the SBITZ group had temporary, self-resolving gastrointestinal disturbances. One patient in the CITZ group complained of swelling on the feet and hence he discontinued treatment after 2 weeks. No patient in the SBITZ group discontinued the treatment as a result of AEs. All of the AEs were mild to moderate in nature. In general, all of the patients tolerated therapy very well.
Discussion
In the current era of dermatophytosis, ITZ remains a useful antifungal agent, along with topical treatments, but its usefulness is hampered by its inherent pharmacokinetic shortcomings, leading to inconsistent therapeutic concentrations.12 In real-world clinical practice, all of these factors are often overlooked. A newer formulation of SBITZ has shown more reliable attainment of therapeutic concentration compared with older formulations of CITZ.13,14 There are a few clinical data available on SBITZ use in different indications, but clinical evidence on dermatophytosis is lacking.
The results of this study demonstrated that SBITZ was associated with more rapid improvement and higher complete cure rate than CITZ. In the SBITZ group, 65.38% of patients achieved a complete cure, whereas the same was achieved by only 33.33% of the patients in the CITZ group. In a retrospective study by Mahajan et al published in 2021, 56% of the patients achieved complete clearance of their symptoms in the SBITZ group, whereas 34% achieved the same in the CITZ group (p<0.05).15 From their results, the authors concluded that SBITZ was more effective than CITZ, with a similar safety profile, in the treatment of dermatophytosis. In addition, a retrospective cohort study by Ghate et al on SBITZ concluded that patients treated with SBITZ showed greater improvement in the clearance of symptoms as well as lesions in just 4 weeks.16 In the same study, 51% of the patients achieved a complete cure. In the CLEAR (Clinical Assessment of Itraconazole in Dermatophytosis) study17 on the effectiveness and safety of CITZ, about 70% of patients achieved clinical cure with CITZ. But in all of the above studies, along with ITZ, a topical antifungal was also prescribed. In our study, we have reported better and significant results with SBITZ than with CITZ without the use of a topical antifungal; however, an emollient was used. Emollient use may improve barrier dysfunction and help to achieve better symptom resolution.
In our study, the mycological cure rate (based on KOH mount) was not statistically significant, with 84.61% of patients in the SBITZ group and 66.67% of patients in the CITZ group achieving a mycological cure. These results are not in line with other clinical trials comparing the efficacy and safety of SBITZ and CITZ in patients with onychomycosis.10 Recurrence was seen in both groups, with no statistically significant difference. On subgroup analysis, similar results were obtained for chronic dermatophytosis, where patients in the SBITZ group showed better improvement. In a report published in 2021, SBITZ was found to be effective in the management of naïve, recurrent, and chronic dermatophytosis.16 Moreover, SBITZ continued to be associated with a decrease in TSS during the treatment period, as well as with an improvement in overall disease severity, as measured by BSA involvement. In terms of IGA, as well, SBITZ demonstrated remarkably better results.
Apart from a complete cure, significant percentage reductions were seen in all mean TSS, BSA, and IGA scores at weeks 2 and 4 for SBITZ. This indicates that SBITZ can improve the lesions and symptoms in as little as 2 weeks. In the SBITZ group, a TSS reduction was seen in 93% of patients at the end of 4 weeks. Similar results were also seen in another study,16 where 89.8% of patients achieved a reduction in TSS. We also noticed a reduction in BSA involvement in 92.26% of the patients in the SBITZ group, which is similar to the previous study, where 81% of patients achieved such a reduction.16 This indicates that SBITZ is effective in relieving the symptoms as well as the lesions of dermatophytosis.
These better cure rates in SBITZ can be attributed to its pharmacokinetic advantages compared to CITZ. ITZ is a weak base molecule with a highly variable absorption pattern, leading to wide fluctuations in its blood concentration,18 and hence the bioavailability of CITZ is only around 55%.9,19 For any drug to produce an optimal clinical effect, its absorption and therefore its bioavailability should be high, with minimal intraindividual and interindividual variability. SBITZ contains a solid dispersion of ITZ in a uniform non-pellet formulation containing a pH-dependent polymeric matrix (HPMCP), which enhances its dissolution and intestinal absorption.11 Therefore, SBITZ is consistently released and available for absorption throughout the small intestine, which is the main site of absorption of ITZ,11,20 ensuring increased bioavailability and less intraindividual and interindividual variability.21
One of the most important predictors of the outcome of any antifungal drug in the treatment of dermatophytosis is its concentration in sebum. ITZ is a lipophilic drug, and therefore its excretion in sebum and the concentration achieved in the stratum corneum are important, particularly in patients with dermatophytosis. In an unpublished Indian study, the sebum concentration of SBITZ and CITZ was compared in healthy volunteers and it was found that the sebum concentration of SBITZ was 11.6% greater than that of CITZ in just 7 days (p=0.01).22 Thus, a higher drug concentration achieved at the target site can aid in extensive eradication of fungus from the lesions, as was evident from the higher mycological cure rate in the SBITZ group in our study. Thus, the high concentration achieved in sebum may be responsible for the better improvement in many assessed parameters in the SBITZ group in our study.
All patients in both groups tolerated the therapy very well and there were no serious AEs. Both therapies were found to be safe and well tolerated. A total of five AEs were reported, all of which were mild in nature. Only one patient in the CITZ group discontinued the therapy owing to AEs.
This is the first clinical trial of the comparison of SBITZ with CITZ in dermatophytosis, in Indian patients. In this clinical trial, the treatment period was only 4 weeks, and a longer duration of therapy may be required in view of further prevention of recurrence. The main limitation of this study is the relatively small sample size. Hence, long-term clinical trials with a larger population are warranted to validate the results of the present study.
Conclusion
Patients treated with SBITZ showed greater improvement in the clearance of lesions compared with those treated with CITZ. In addition, SBITZ led to significant improvements in naïve, recurrent, and chronic patients, enabling its placement in the armamentarium of the management of all types of dermatophytosis. It is safe and well tolerated. In the light of real-world evidence on effectiveness and safety, SBITZ should be considered as a potent therapeutic choice to effectively control the current menace of dermatophytosis in India.
Data Sharing Statement
The datasets are available only on request due to privacy/ethical restrictions, and can be requested from [email protected].
Disclosure
Dr Manjunath Shenoy reports personal fees and non-financial support from Glenmark Pharmaceuticals Ltd, India, outside the submitted work. Dr Dhiraj Dhoot, Dr Harshal Mahajan, and Dr Hanmant Barkate report that they are employees of Glenmark Pharmaceuticals Ltd. The authors report no other conflicts of interest in this work.
References
1. Rajagopalan M, Inamadar A, Mittal A, et al. Expert consensus on the management of dermatophytosis in India (ECTODERM India). BMC Dermatol. 2018;18(1):6. doi:10.1186/s12895-018-0073-1
2. Verma S, Madhu R. The great Indian epidemic of superficial dermatophytosis: an appraisal. Indian J Dermatol. 2017;62(3):227–236.
3. Dogra S, Uprety S. The menace of chronic and recurrent dermatophytosis in India: is the problem deeper than we perceive? Indian Dermatol Online J. 2016;7(2):73–76. doi:10.4103/2229-5178.178100
4. Das S, De A, Saha R, et al. The current Indian epidemic of dermatophytosis: a study on causative agents and sensitivity patterns. Indian J Dermatol. 2020;65(2):118–122. doi:10.4103/ijd.IJD_203_19
5. Boonk W, de Geer D, de Kreek E, Remme J, van Huystee B. Itraconazole in the treatment of tinea corporis and tinea cruris: comparison of two treatment schedules. Mycoses. 1998;41(11–12):509–514. doi:10.1111/j.1439-0507.1998.tb00714.x
6. Rengasamy M, Shenoy MM, Dogra S, et al. Indian Association of Dermatologists, Venereologists and Leprologists (IADVL) Task Force against Recalcitrant Tinea (ITART) Consensus on the Management of Glabrous Tinea (INTACT). Indian Dermatol Online J. 2020;11(4):502–519.
7. Lindsay J, Mudge S, Thompson GR. Effects of food and omeprazole on a novel formulation of super bioavailability itraconazole in healthy subjects. Antimicrob Agents Chemother. 2018;62(12):e01723–18. doi:10.1128/AAC.01723-18
8. Vaughn B, Rotolo S, Roth H. Circadian rhythm and sleep influences on digestive physiology and disorders. Chrono Physiol Ther. 2014;4:67–77. doi:10.2147/CPT.S44806
9. SP0RANOX® (itraconazole) capsule [prescribing information]. Raritan, NJ: Ortho-McNeil-Janssen Pharmaceuticals, Inc; 2018.
10. LOZANOC® (itraconazole 50 mg) capsule [prescribing information]. Salisbury South, SA: Mayne Pharma International Pty Ltd; 2020.
11. Abuhelwa AY, Foster DJ, Mudge S, Hayes D, Upton RN. Population pharmacokinetic modeling of itraconazole and hydroxyitraconazole for oral SUBA-itraconazole and sporanox capsule formulations in healthy subjects in fed and fasted states. Antimicrob Agents Chemother. 2015;59(9):5681–5696. doi:10.1128/AAC.00973-15
12. Prentice AG, Glasmacher A. Making sense of itraconazole pharmacokinetics. J Antimicrob Chemother. 2005;56(Suppl 1):i17–i22. doi:10.1093/jac/dki220
13. Lindsay J, Sandaradura I, Wong K, et al. Serum levels, safety and tolerability of new formulation SUBA-itraconazole prophylaxis in patients with haematological malignancy or undergoing allogeneic stem cell transplantation. J Antimicrob Chemother. 2017;72(12):3414–3419. doi:10.1093/jac/dkx295
14. Nield B, Larsen SR, van Hal SJ. Clinical experience with new formulation SUBA®-itraconazole for prophylaxis in patients undergoing stem cell transplantation or treatment for haematological malignancies. J Antimicrob Chemother. 2019;74(10):3049–3055. doi:10.1093/jac/dkz303
15. Mahajan H, Dhoot D, Deshmukh G, Barkate H. Comparative clinical effectiveness and safety of super bioavailable itraconazole and conventional itraconazole in management of dermatophytosis: a retrospective data analysis. Int J Res Dermatol. 2021;7:388–394. doi:10.18203/issn.2455-4529.IntJResDermatol20211427
16. Ghate S, Dhoot D, Mahajan H, Barkate H. Clinical assessment of super bioavailable Itraconazole 50 mg in dermatophytosis (Clear 50). IP Indian J Clin Exp Dermatol. 2021;7(2):125–129. doi:10.18231/j.ijced.2021.024
17. Mahajan H, Dhoot D, Barkate H. Clinical assessment of itraconazole in dermatophytosis (CLEAR Study): a retrospective evaluation. Int J Sci Stud. 2020;8(2):1–5.
18. Gintjee TJ, Donnelley MA, Thompson GR. Aspiring antifungals: review of current antifungal pipeline developments. J Fungi (Basel). 2020;6(1):28. doi:10.3390/jof6010028
19. Brouwers J, Geboers S, Mols R, Tack J, Augustijns P. Gastrointestinal behavior of itraconazole in humans - Part 1: supersaturation from a solid dispersion and a cyclodextrin-based solution. Int J Pharm. 2017;525(1):211–217. doi:10.1016/j.ijpharm.2017.04.029
20. Abuhelwa AY, Mudge S, Hayes D, Upton RN, Foster DJ. Population in vitro-in vivo correlation model linking gastrointestinal transit time, pH, and pharmacokinetics: itraconazole as a model drug. Pharm Res. 2016;33(7):1782–1794. doi:10.1007/s11095-016-1917-1
21. Cauwenbergh G, Degreef H, Heykants J, Woestenborghs R, Van Rooy P, Haeverans K. Pharmacokinetic profile of orally administered itraconazole in human skin. J Am Acad Dermatol. 1988;18(2):263–268. doi:10.1016/S0190-9622(88)70037-7
22. Harshal M, Gaurav J, Dhiraj D, Gaurav D, Hanmant B. Serum and sebum pharmacokinetics evaluation of a novel formulation of itraconazole in healthy volunteers. Indian J Drugs Dermatol. 2021. In press.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
