Back to Journals » Neuropsychiatric Disease and Treatment » Volume 13
An observational study of duloxetine versus SSRI monotherapy in Japanese patients with major depressive disorder: subgroup analyses of treatment effectiveness for pain, depressive symptoms, and quality of life
Authors Kuga A, Tsuji T , Hayashi S , Fujikoshi S, Tokuoka H , Yoshikawa A, Escobar R , Tanaka K , Azekawa T
Received 8 March 2017
Accepted for publication 10 July 2017
Published 4 August 2017 Volume 2017:13 Pages 2115—2124
DOI https://doi.org/10.2147/NDT.S136448
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Taro Kishi
Atsushi Kuga,1 Toshinaga Tsuji,2 Shinji Hayashi,2 Shinji Fujikoshi,3 Hirofumi Tokuoka,1 Aki Yoshikawa,4 Rodrigo Escobar,5 Kazuhide Tanaka,6 Takaharu Azekawa7
1Bio Medicine, Medicines Development Unit Japan, Eli Lilly Japan K.K., Kobe, 2Medical Affairs Department, Shionogi & Co., Ltd., Osaka, 3Statistical Science, 4Scientific Communications, Medicines Development Unit Japan, Eli Lilly Japan K.K., Kobe, Japan; 5Bio-Medicines, Eli Lilly and Company, Indianapolis, IN, USA; 6Hitsuji Clinic, Kusatsu, Japan; 7Shioiri Mental Clinic, Yokosuka, Japan
Objective: To examine how clinical and demographic patient baseline characteristics influence effectiveness of duloxetine versus selective serotonin reuptake inhibitor (SSRI) treatment, in real-world Japanese clinical settings of patients with major depressive disorder (MDD) and associated painful physical symptoms (PPS).
Methods: This was a multicenter, 12-week, prospective, observational study in patients with MDD (Quick Inventory of Depressive Symptomatology ≥16) and at least moderate PPS (Brief Pain Inventory-Short Form [BPI-SF] average pain ≥3). Patients received duloxetine or SSRIs (escitalopram, sertraline, paroxetine, or fluvoxamine). Assessments were made by using BPI-SF average pain, 17-item Hamilton Rating Scale for Depression (HAM-D17), EuroQol 5-dimension questionnaire, Social Adaptation Self-Evaluation Scale, Global Assessment of Functioning, and ability to work. Predefined subgroups included the number of previous episodes of depression (0 vs ≥1), baseline BPI-SF average pain score (≤6 vs >6), baseline HAM-D17 total score (≤18 vs >18), baseline HAM-D17 retardation (≤7 vs >7) and anxiety somatic subscale scores (≤6 vs >6), and age (<65 vs ≥65 years).
Results: Treatment effectiveness was evaluated in 523 patients (duloxetine N=273, SSRIs N=250). Treatment with duloxetine was superior to SSRIs on most outcome measures in patients experiencing their first depressive episode, those with higher baseline PPS levels, and in patients with more severe baseline depression. This was also the case for older patients. In patients with less severe depression, SSRI treatment tended to show more improvements in depression and quality of life measures versus duloxetine treatment.
Conclusion: These preplanned subgroup analyses of data from a prospective observational study suggest that, for Japanese MDD patients with PPS, duloxetine is more effective than SSRIs in patients with a first episode of MDD, with more severe depression, or more severe PPS.
Keywords: depression, duloxetine, pain, selective serotonin reuptake inhibitors, first episode
Introduction
Major depressive disorder (MDD) is a prevalent disease with a devastating impact on one’s personal life.1 Although there has been some progress, full recovery is still difficult to achieve.2,3 In clinical practice, it is important to personalize the treatment plan for each patient, and to understand the many available treatment options, including pharmacotherapy, cognitive behavioral therapy, and electroconvulsive therapy.4 For treatment optimization, clinical investigators are developing tailored medicine approaches for patients with MDD using genetic, biochemical, and neuroimaging approaches, as well as MDD symptom assessment through clinical interviews.5–8
A large percentage of patients with MDD report painful physical symptoms (PPS; >60%9,10); therefore, it is clinically meaningful to categorize MDD patients with PPS as a major phenotype of this disorder.11 For affected patients, PPS not only seriously impacts their quality of life (QoL),12 but also its presence is associated with the severity of MDD symptoms and lower remission rates.13 In patients with MDD, residual symptoms after treatment are risk factors for relapse.14 Moderate-to-severe PPS is a prevalent residual symptom in patients with MDD after treatment, as Harada et al have demonstrated recently.15 Moreover, PPS improvement is a potential predictor of the clinical course of depression.11 The overall impact of PPS on treatment outcome of MDD underlines the need for more effective, tailored treatment approaches for this patient population.
Duloxetine is a unique serotonin norepinephrine reuptake inhibitor which has been shown to be effective in the treatment of pain in patients with fibromyalgia,16 chronic low back pain,17 or diabetic peripheral neuropathic pain.18 While duloxetine was associated with significantly greater benefit on measures of pain and functioning compared with selective serotonin reuptake inhibitors (SSRIs) in a randomized clinical trial in patients with MDD,19 systematic analysis did not reveal an advantage of duloxetine over SSRIs in the treatment of patients with depression.20 The question remains how the use of antidepressants can be optimized for patients with MDD and associated PPS and which patient subgroup might benefit most from a given treatment approach.
In a recent prospective observational study, we investigated treatment outcome in patients with MDD and PPS residing in Japan who received treatment with either duloxetine or an SSRI for 12 weeks. At 4 weeks post-baseline (the primary endpoint), there was no statistically significant difference between treatment groups for change in Brief Pain Inventory-Short Form (BPI-SF) average pain score.21 Additionally, no statistically significant differences between treatment groups were noted for the 17-item Hamilton Rating Scale for Depression (HAM-D17) total score, the EuroQol 5-dimension questionnaire (EQ-5D), the Global Assessment of Functioning (GAF), or the Social Adaptation Self-Evaluation Scale (SASS). However, patients who received duloxetine presented a higher responder rate and a greater improvement in BPI-SF average pain score over time compared with patients receiving SSRIs.
Based on those results, the objective of the subgroup analyses presented here was to examine how patient baseline characteristics such as symptom severity, number of episodes, and age may influence outcome after treatment with duloxetine or SSRIs in real-world clinical settings. We report the results of predefined subgroup analyses comparing the effectiveness of treatment with duloxetine versus SSRI in patient groups stratified by the number of previous episodes of depression, baseline BPI-SF average pain score, baseline HAM-D17 total score, HAM-D17 retardation and anxiety somatic subscale scores, and age.
Methods
Study design and patients
This was a prospective, observational, 12-week study assessing treatment outcomes in patients with MDD and PPS who received duloxetine or one of the following SSRIs: escitalopram, sertraline, paroxetine, or fluvoxamine. Patients were male or female, ≥20 years old, and resided in Japan. All patients presented with an episode of MDD without psychotic traits, as defined by the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision.22 Patients were diagnosed by the investigator with at least moderate depression (Quick Inventory of Depressive Symptomatology ≥16) and at least moderate PPS (BPI-SF average pain ≥3). Patients with a previous diagnosis of bipolar disorder, schizophrenia, or other psychotic disorder, or a current diagnosis of dysthymic disorder or adjustment disorder were excluded from the study. Patients with PPS that originated from organic disease, aside from MDD, and those being treated with opioids for their PPS were also excluded from the study.
The study was conducted in accordance with good post-marketing study practices23 and applicable laws and regulations of the country in which the study was conducted. The Japanese Ministry of Health, Labour and Welfare reviewed and approved the protocol. Patients provided written informed consent before enrollment. Additional details regarding study design and patient selection are presented in the primary study publication.21
Assessments
Item 5 on the BPI-SF (average pain) was used to quantify PPS. Additional outcome measures included HAM-D17, rated according to the Structured Interview Guide for the HAM-D17 for depressive symptoms, EQ-5D for QoL, SASS, GAF for social functioning, and ability to work. Ability to work was defined as the proportion of patients being able to work according to the investigator’s judgment out of the entire patient population (excluding patients who retired early).
Statistical methods
Prespecified subgroup analyses of all effectiveness outcome measures were based on 1) the presence or absence of a previous depressive episode, 2) BPI-SF average pain score (≤6 vs >6), 3) HAM-D17 total score (≤18 vs >18), 4) HAM-D17 retardation subscale score (≤7 vs >7), 5) HAM-D17 anxiety somatic subscale score (≤6 vs >6), and 6) patient age (<65 vs ≥65). All enrolled patients with baseline and at least one post-baseline score were included in the analyses, excluding patients with non-retrievable case report forms, patients for whom administration of the study drug could not be confirmed, and patients who did not meet entry criteria. For treatment group comparisons, propensity scoring (the probability of treatment assignment conditioned on observed baseline data) was applied to adjust the potential imbalance of baseline data between treatment groups. Logistic regression was used to compute the propensity score, and generally all available baseline data were included in the model. A mixed-effects model with repeated measures analysis was used for comparisons in all subgroups. The model for the fixed effects included treatment (duloxetine/SSRI), propensity score, baseline score (if available), visit, visit-by-treatment interaction, visit-by-propensity score interaction, and visit-by-baseline score interaction (if available). All statistical tests were based on a 2-sided significance level of 0.05 and/or a 2-sided 95% confidence interval. No adjustments for multiplicity were made. All statistical analyses were carried out using SAS version 9.13 or above (SAS Institute, Cary, NC, USA).
Results
Patient disposition, demographics, and baseline characteristics, and information about safety (adverse events, serious adverse events, and discontinuations due to adverse events) are presented in a study by Kuga et al.21
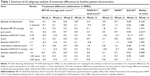
Data from 523 patients were evaluated (duloxetine N=273, SSRIs N=250). In Table 1, all subgroup analyses are summarized. We present treatment differences between duloxetine and SSRIs for the individual outcome measures, with patients stratified by subgroup characteristic. Details for the individual subgroup analyses are provided in Tables 2–4, Figures 1–3, Tables S1–S3, and Figures S1–S3.
Stratification by the number of previous episodes
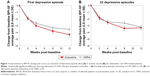
Within the group of patients experiencing their first depressive episodes, treatment with duloxetine tended to be more effective than SSRIs in improving most outcome measures (Table 2). This was especially true for BPI-SF average pain scores at 8 and 12 weeks post-baseline (Table 2; Figure 1A), as well as HAM-D17 total scores, GAF scores, EQ-5D scores, and ability to work at 12 weeks (Table 2).
There was no clear difference observed between treatment groups in patients who experienced at least their second recurrent episode of depression; all patients showed improvement in all measures (Table 2; Figure 1B). In both treatment groups, first-episode patients had generally better outcomes compared with patients with recurrent depressive episodes.
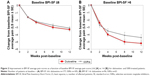
Baseline BPI-SF average pain score
Within the group of patients with BPI-SF average pain scores >6, duloxetine was associated with more overall improvements in most outcome measures (Table 3; Figure 2B). This effect was most apparent in patients’ ability to work at 12 weeks post-baseline, where duloxetine-treated patients were significantly more likely to be judged as being able to work at 12 weeks post-baseline compared with SSRI-treated patients (Table 3).
In the subgroup of patients with BPI-SF average pain scores ≤6, both duloxetine- and SSRI-treated patients showed improvement in all measures, but no clear difference was observed between treatment groups (Table 3; Figure 2A).
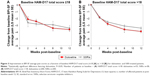
HAM-D17 total score, HAM-D17 retardation subscale score, and HAM-D17 anxiety somatic subscale score
Within the group of patients with baseline HAM-D17 total scores >18, duloxetine-treated patients tended to show overall more improvement in most outcome measures compared with SSRI-treated patients. In this patient subgroup, duloxetine treatment led to significantly better improvements in BPI-SF average pain scores at 8 weeks post-baseline (Figure 3B), as well as GAF and ability to work at 12 weeks post-baseline compared with patients receiving SSRIs (Table 4).
In the subgroup of patients with HAM-D17 total scores ≤18, both duloxetine- and SSRI-treated patients showed improvement in all measures (Table 4; Figure 3A). The only difference observed between treatment groups was in the EQ-5D at 12 weeks post-baseline, where SSRI-treated patients showed more improvements compared with duloxetine (Table 4).
Results observed for HAM-D17 retardation subscale scores and HAM-D17 anxiety somatic subscale scores were similar to those observed with HAM-D17 total scores (Tables S1 and S2; Figures S1A and B, and S2A and B). Within the group of patients with more severe baseline subscale scores (HAM-D17 retardation subscale score >7, HAM-D17 anxiety somatic subscale score >6), duloxetine-treated patients tended to show more improvements on most outcome measures compared with SSRI-treated patients. Also, within the group of patients with lower baseline subscale scores (HAM-D17 retardation subscale score ≤7, HAM-D17 anxiety somatic subscale score ≤6), both duloxetine- and SSRI-treated patients showed improvement on all measures. Although there was no overall clear distinction between treatment groups, SSRI-treated patients experienced more improvement on HAM-D17 total scores compared with those treated with duloxetine. This effect was most pronounced at 2 and 4 weeks post-baseline in patients with baseline HAM-D17 retardation subscale score ≤7.
Patient age
In the subgroup of patients aged ≥65 years, duloxetine treatment led to more improvements in most of the outcome measures compared with SSRI treatment (Table S3). Within the group of patients <65 years old, both duloxetine- and SSRI-treated patients showed improvement in all measures, with no clear difference observed between treatment groups for any outcome measure (Table S3; Figure S3A).
Discussion
In the present study, we examined treatment outcome of patients with MDD and moderate-to-severe PPS in a real-world setting. Based on planned subgroup analyses, we investigated the influence of baseline patient characteristics on treatment outcomes after exposure to duloxetine versus SSRIs. Patients with their first episode of MDD and those with severe PPS, severe MDD, or at least 65 years of age showed better outcome after treatment with duloxetine versus treatment with SSRIs. No apparent outcome differences between duloxetine and SSRIs were observed for patients with other baseline characteristics.
Pain improvements were greater in first-episode patients who received duloxetine than those who received SSRIs. Overall, PPS improvement in first-episode patients treated with either duloxetine or SSRIs was numerically higher than PPS improvement in patients with recurrent depressive episodes. Observed improvements of depression (HAM-D score), function (GAF), and QoL (EQ-5D) in first-episode patients with MDD were greater in patients receiving duloxetine than in those receiving SSRIs. In patients with recurrent MDD episodes, differences in treatment outcome after duloxetine versus SSRI treatment were less clear and of smaller magnitude.
The successful treatment of PPS in patients with MDD should be an important treatment goal. Residual symptoms of MDD are risk factors for symptom recurrence after treatment.29 A previous study demonstrated that remitted patients with residual physical symptoms have a greater risk of relapse.30 Therefore, persistent PPS may predict subsequent episodes of depression. Recently, Novick et al31 have reported the result of a regression model analysis of a prospective observational study in patients with MDD treated with duloxetine or SSRIs for 3 months. They compared 198 patients in the remitted pain group (pain at baseline resolved at 3 months) and 151 patients in the persistent pain group (pain at baseline observed at 3 months) and found that pain persisted more frequently in patients with a previous MDD episode.
These results highlight an interesting difference between first-episode MDD and recurrent MDD from a pharmacotherapy perspective. Notably, treatment outcome seems to be independent of the number of depressive episodes.32,33 However, the number of depressive episodes is a predictor of recurrence of depressive disorder,34 and biological changes could be underlying the recurrence of affective disorders.35 Therefore, optimal treatment of depression in the first episode is particularly important.
Taken together with our results, it appears that the effective treatment of PPS in the first MDD episode may influence overall treatment outcome. Consequently, optimal treatment of severe pain associated with MDD may have a considerable impact on overall treatment outcome. Considering our finding of a treatment advantage with duloxetine versus SSRI in first-episode patients, our data suggest two main conclusions. First, in patients with MDD and PPS, initial treatment of PPS may change the clinical course of MDD due to the potential negative effects of residual symptoms on long-term prognosis. Second, the advantageous effect of duloxetine on PPS can be highlighted in the first episode of MDD.
In our subgroup analysis by baseline PPS severity, mean changes in BPI-SF scores were numerically higher in the subgroup with severe PPS. BPI-SF average pain scores were distinctly different between both treatment groups, although the difference was not statistically significant, possibly due to the small sample size. This trend is similar in a previous report showing superior effect of duloxetine in comparison to SSRIs in pain improvement in the pain-enriched subgroup (baseline BPI-SF score ≥3) compared with all patients.19 Since the number of patients with severe PPS (baseline BPI-SF >6) was limited in the current report, this possible advantage for duloxetine in patients with MDD and severe PPS should be further investigated.
To examine the influence of baseline depression severity on treatment outcome by duloxetine or SSRIs, patients were stratified by their HAM-D17 baseline values. In the subgroup with severe MDD (defined as a baseline HAM-D17 score >18), patients treated with duloxetine presented overall more improvement in BPI-SF scores compared with patients receiving SSRIs. In patients with less severe depression, SSRI treatment tended to show more improvement of depression and QoL versus duloxetine treatment. The current real-world data are consistent with previous findings of Thase et al,36 in which data from six Phase II/III studies comparing duloxetine with SSRI treatment in patients with MDD were analyzed. Thase et al defined moderate-to-severe depression as HAM-D17 score ≥19. In patients with moderate-to-severe depression, remission rates were 35.9% after treatment with duloxetine versus 28.6% after treatment with SSRIs (P=0.046).36
In the Japanese super-aged society, 39.3% of people 61–70 years old are suffering from chronic pain, and this percentage increases with age.37 Since pain itself diminishes QoL and functional ability, pain control in the elderly population is critically important. The data presented here contain a relatively small subgroup of aged patients (≥65 years old). In the aged patient subgroup, treatment with duloxetine was associated with more improvements in PPS at 8 and 12 weeks post-baseline compared to SSRIs. In addition, improvement in the GAF was significantly greater in the duloxetine-treated group versus the SSRI-treated group. Considering the limited sample size, a possible treatment advantage of duloxetine in elderly patients with MDD warrants further exploration before conclusions can be made.
Several limitations need to be considered for the interpretation of the results presented here. Due to the observational study design without treatment randomization, no firm conclusions about cause and effect of outcomes can be drawn. While the analyzed subgroups were prespecified, the analyses were exploratory and no adjustments for multiplicity were made. In addition, even though comparisons between duloxetine and SSRIs were conducted after covariate adjustments were made for the measured confounding factors, potential biases due to unmeasured confounding factors that were not adjusted for in the analyses may have influenced the results. Potential differences due to gender, ethnicity, or cultural considerations (our patient sample was mostly Japanese) may be underrepresented in this sample. Finally, this study was sponsored by Eli Lilly Japan KK and Shionogi & Co, Ltd, manufacturers of duloxetine, and therefore sponsorship bias cannot be excluded.
Conclusion
Targeted use of antidepressants may yield optimized outcomes during treatment of MDD. Duloxetine appears to be more effective for certain subgroups of patients compared with SSRIs. Our preplanned subgroup analyses from a prospective observational study suggest that duloxetine is more effective compared with SSRIs in the treatment of Japanese patients with MDD and accompanying PPS experiencing their first episode of MDD, in patients with a higher baseline severity of pain or depression, or in older patients.
Acknowledgments
This study was sponsored by Eli Lilly Japan K.K., the manufacturer and licensee of Cymbalta®, who were involved in the preparation of the manuscript. The study was also funded by Shionogi & Co., Ltd. The study and the analysis were conducted by CMIC Co, Ltd. Medical writing assistance was provided by Rodney Moore, PhD, inVentiv Health Clinical, LLC, funded by Eli Lilly Japan K.K. and Shionogi & Co., Ltd.
Author contributions
All of the authors contributed to the conception of the study, interpretation of the data, drafting and critical revision of the manuscript, provided final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
AK, SF, HT and AY are full-time employees of Eli Lilly Japan K.K.. RE is a full-time employee of Eli Lilly and Company. TT and SH are full-time employees and stockholders of Shionogi & Co., Ltd. TA received speakers’ honoraria from Eli Lilly Japan, K.K., Takeda Pharmaceutical Co, Ltd., and Otsuka Pharmaceutical Co, Ltd. The authors report no other conflicts of interest in this work.
References
GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1603–1658. | ||
Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905–1917. | ||
Steinert C, Hofmann M, Kruse J, Leichsenring F. The prospective long-term course of adult depression in general practice and the community. A systematic literature review. J Affect Disord. 2014;152–154:65–75. | ||
Saltiel PF, Silvershein DI. Major depressive disorder: mechanism-based prescribing for personalized medicine. Neuropsychiatr Dis Treat. 2015;11:875–888. | ||
Zajkowska ZE, Englund A, Zunszain PA. Towards a personalized treatment in depression: endocannabinoids, inflammation and stress response. Pharmacogenomics. 2014;15(5):687–698. | ||
Thase ME. Using biomarkers to predict treatment response in major depressive disorder: evidence from past and present studies. Dialogues Clin Neurosci. 2014;16(4):539–544. | ||
Phillips ML, Chase HW, Sheline YI, et al. Identifying predictors, moderators, and mediators of antidepressant response in major depressive disorder: neuroimaging approaches. Am J Psychiatry. 2015;172(2):124–138. | ||
McGrath PJ, Khan AY, Trivedi MH, et al. Response to a selective serotonin reuptake inhibitor (citalopram) in major depressive disorder with melancholic features: a STAR*D report. J Clin Psychiatry. 2008;69(12):1847–1855. | ||
Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004;66(1):17–22. | ||
Shimodera S, Kawamura A, Furukawa TA. Physical pain associated with depression: results of a survey in Japanese patients and physicians. Compr Psychiatry. 2012;53(6):843–849. | ||
Fava M, Mallinckrodt CH, Detke MJ, Watkin JG, Wohlreich MM. The effect of duloxetine on painful physical symptoms in depressed patients: do improvements in these symptoms result in higher remission rates? J Clin Psychiatry. 2004;65(4):521–530. | ||
Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162(6):1171–1178. | ||
Young EA, Kornstein SG, Marcus SM, et al. Sex differences in response to citalopram: a STAR*D report. J Psychiatr Res. 2009;43(5):503–511. | ||
Judd LL, Akiskal HS, Maser JD, et al. Major depressive disorder: a prospective study of residual subthreshold depressive symptoms as predictor of rapid relapse. J Affect Disord. 1998;50(2–3):97–108. | ||
Harada E, Satoi Y, Kikuchi T, Watanabe K, Alev L, Mimura M. Residual symptoms in patients with partial versus complete remission of a major depressive disorder episode: patterns of painful physical symptoms in depression. Neuropsychiatr Dis Treat. 2016;12:1599–1607. | ||
Arnold LM. Duloxetine and other antidepressants in the treatment of patients with fibromyalgia. Pain Med. 2007;8(Suppl 2):S63–S74. | ||
Williamson OD, Sagman D, Bruins RH, Boulay LJ, Schacht A. Antidepressants in the treatment for chronic low back pain: questioning the validity of meta-analyses. Pain Pract. 2014;14(2):E33–E41. | ||
King JB, Schauerhamer MB, Bellows BK. A review of the clinical utility of duloxetine in the treatment of diabetic peripheral neuropathic pain. Ther Clin Risk Manag. 2015;11:1163–1175. | ||
Martinez JM, Katon W, Greist JH, et al. A pragmatic 12-week, randomized trial of duloxetine versus generic selective serotonin-reuptake inhibitors in the treatment of adult outpatients in a moderate-to-severe depressive episode. Int Clin Psychopharmacol. 2012;27(1):17–26. | ||
Cipriani A, Koesters M, Furukawa TA, et al. Duloxetine versus other anti-depressive agents for depression. Cochrane Database Syst Rev. 2012;10:CD006533. | ||
Kuga A, Tsuji T, Hayashi S. An observational study of duloxetine versus SSRI monotherapy for the treatment of painful physical symptoms in Japanese patients with major depressive disorder: primary analysis. Neuropsychiatr Dis Treat. In press 2017. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Text revision. Washington DC: American Psychiatric Association; 2000. | ||
Ministry of Health, Labor, and Welfare. Good post-marketing study practices. Ordinance No 171 issued on 20 December, 2004. | ||
Poquet N, Lin C. The Brief Pain Inventory (BPI). J Physiother. 2016;62(1):52. | ||
Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ. 1998;316(7133):736–741. | ||
Aas IH. Global Assessment of Functioning (GAF): properties and frontier of current knowledge. Ann Gen Psychiatry. 2010;9:20. | ||
Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–296. | ||
Bosc M, Dubini A, Polin V. Development and validation of a social functioning scale, the Social Adaptation Self-evaluation Scale. Eur Neuropsychopharmacol. 1997;7(Suppl 1):S57–S70. | ||
Nierenberg AA. Residual symptoms in depression: prevalence and impact. J Clin Psychiatry. 2015;76(11):e1480. | ||
Paykel ES, Scott J, Teasdale JD, et al. Prevention of relapse in residual depression by cognitive therapy: a controlled trial. Arch Gen Psychiatry. 1999;56(9):829–835. | ||
Novick D, Montgomery W, Aguado J, Peng X, Haro JM. Factors associated with and impact of pain persistence in Asian patients with depression: a 3-month, prospective observational study. Int J Psychiatry Clin Pract. 2017;21(1):29–35. | ||
Joffe RT, Young LT, Levitt AJ, MacQueen G, Marriott MJ, Robb J. Number of episodes and antidepressant response in major depression. Int J Neuropsychopharmacol. 1999;2(2):111–113. | ||
Trivedi MH, Rush AJ, Wisniewski SR, et al; STAR*D Study Team. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28–40. | ||
Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AT. Prevalence and predictors of recurrence of major depressive disorder in the adult population. Acta Psychiatr Scand. 2010;122(3):184–191. | ||
Post RM. Mechanisms of illness progression in the recurrent affective disorders. Neurotox Res. 2010;18(3–4):256–271. | ||
Thase ME, Pritchett YL, Ossanna MJ, Swindle RW, Xu J, Detke MJ. Efficacy of duloxetine and selective serotonin reuptake inhibitors: comparisons as assessed by remission rates in patients with major depressive disorder. J Clin Psychopharmacol. 2007;27(6):672–676. | ||
Inoue S, Kobayashi F, Nishihara M, et al. Chronic pain in the Japanese community – prevalence, characteristics and impact on quality of life. PLoS One. 2015;10(6):e0129262. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.