Back to Journals » International Journal of Women's Health » Volume 15
An Analysis of the Rate, Indications, and Associated Maternal Mortality for Cesarean Sections at a Tertiary Care Hospital, First Report from Somalia
Authors Hussein AI, Kurtay S, Omar AA, Yusuf AA, Mohamud RYH
Received 25 July 2022
Accepted for publication 1 February 2023
Published 11 February 2023 Volume 2023:15 Pages 225—233
DOI https://doi.org/10.2147/IJWH.S383122
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Marleen van Gelder
Ahmed Issak Hussein,1 Sabri Kurtay,1 Abdikarim Ali Omar,1 Abdisalam Abdullahi Yusuf,2 Rahma Yusuf Haji Mohamud1
1Obstetrics and Gynecology department, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia; 2Pediatric Department, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia
Correspondence: Ahmed Issak Hussein, Mogadishu Somalia Turkish Training and Research Hospital, Mogadishu, Somalia, Tel +252615597479, Email [email protected]
Background: There has been an increase in worldwide cesarean section rates, although they remain low in most Sub-Saharan African countries, including Somalia. The present is the first hospital-based study that analyzes the rate, indications, and associated maternal mortality of cesarean deliveries reported from Somalia.
Methods: This retrospective study reviewed data of all deliveries from 2015 to 2021 using electronic medical records in the hospital information system. Retrieved data include baseline demographic characteristics, mode of delivery, indications and the type of cesarean section, and the documented maternal mortality during the study period.
Results: During seven years, there were 12,540 total deliveries. Among these, 2703 were cesarean sections giving an overall cesarean section rate of 21.6%. The mean age of the patients was 26.7± 7.3 years [14– 44 years]. Multiparous mothers constituted 67.7% during the study period. According to cesarean deliveries, nulliparous mothers (55.7%) underwent the maximum number of cesarean sections. Emergency cesarean section was the predominant intervention compared to elective C-sections (59.2% vs 40.8%). Primary CS was the most common predominant, while repeat CS increased timely, 77.7% vs 22.3%, respectively. Overall, previous C-sections and fetal distress were the two most common indications for cesarean delivery (22.3% and 22.1%), respectively. C-sections were predominant in women of younger age, Primiparity, having term deliveries, and did not receive regular antenatal care. The maternal mortality rate was 1.7%, and 61% was due to direct obstetric hemorrhage, including postpartum hemorrhage, Placenta abruption, and uterine rupture.
Conclusion: The study findings showed a slight increase in cesarean delivery rates during the study period. This rate is higher than the 10– 15% recommended by the WHO in developing countries. Policies and efforts to decrease unnecessary cesarean sections should be promoted and implemented at each health facility.
Keywords: cesarean delivery, indications, maternal mortality, Sub-Saharan Africa
Introduction
While most pregnancies and births are uneventful, all pregnancies are at risk.1 Around 15% of all pregnant women will develop a potentially life-threatening complication that calls for skilled care; some will require significant obstetrical intervention to survive.
Cesarean section is a significant obstetric procedure used to save the lives of mothers and their infants from potentially fatal pregnancy and childbirth complications.2 There has been an increase in worldwide cesarean section rates, although they remain low in most African nations.3 Despite a global increase in rates, the cesarean delivery rate in Sub-Saharan Africa remains stable at around 3.5%.4 However, the number of C-sections performed in private hospitals has risen in almost every country compared to public healthcare settings, including sub-Saharan Africa.3,5
Unnecessary Cesarean section may increase maternal, neonatal, and infant morbidity and mortality.2 Furthermore, this increasing caseation rate is a significant public health problem because it increases the health risks for mothers and babies as well as the costs of health care compared with normal delivery, particularly in low and middle-income countries.6 Non-medical indications account for one-third of the total 18.5 million C-sections performed annually, contributing significantly to the global excess of C-sections. This very high C-section rate in the world necessitates monitoring all C-section indications in public and private facilities.2 Compared to women who have a vaginal delivery, the risk of pregnancy-related morbidity and mortality is significantly higher for women who have a Caesarean delivery, according to a report by the American College of Obstetricians and Gynecologists (9.2 deaths per 100,000 live births for vaginal deliveries vs 35.9 deaths per 100,000 live births for cesarean deliveries, respectively).7 The World Health Organization considers Cesarean section rates of 5–15% the optimal range for targeted provision of this life-saving intervention for mothers and infants.8
In resource-limited settings, however, access to safe Cesarean sections is much lower, with estimates ranging from 1–2% in Sub-Saharan African countries.8 Even though not all caesareans are life-saving, cesarean rates of less than 1% indicate an unmet need for potentially life-saving care.9
There have been no studies regarding the rate, indications, and maternal mortality rate for cesarean delivery reported from Somalia. Therefore, this study aimed to analyze the rate, indications and associated maternal mortality rate of cesarean section deliveries over seven years at an only tertiary care hospital in Somalia, which serves a diverse urban and rural population in the country.
Materials and Methods
This retrospective study reviewed and analyzed data of all deliveries at Mogadishu Somali Turkish Training and Research Hospital, a referral teaching and training hospital in Mogadishu, Somalia, from January 2015 to December 2021, using labor ward records and electronic medical records in the hospital information system (HIS).
The Mogadishu Somalia Turkish Training and Research Hospital Clinical Research Ethics Committee were approved for this study (approval number MSTH/7892). In addition, all study participants and a parent of participants under 18 years of age previously consented to use their medical and surgical data in this study. This study was carried out in accordance with the Helsinki Declaration’s contents.
Over seven years, all women who gave birth vaginally or underwent a Cesarean section were included in this study. All Cesarean sections were performed according to established peri-operative protocols. 106 Patients with incomplete data were excluded from the study.
Retrieved data include baseline demographic characteristics such as age, gravity, parity, gestational weeks, mode of delivery, indications for cesarean delivery, the type of cesarean section (Elective or Emergency), and the documented maternal mortality during the study period.
Cesarean section indications were classified as follows: previous cesarean section, fetal distress, prolonged labor, pre-eclampsia, eclampsia, antepartum hemorrhage (placenta Previa or placental abruption), cephalopelvic disproportion, macrosomia, malpresentation (breech, transverse lie, face presentation, arm prolapse), multiple gestations (twins/triplets), cord prolapse, and others. Pregnant mothers with previous uterine surgeries (ie, myomectomy), history of previous traditional cervical cauterizations, those with severe cardiac diseases, fetuses with congenital anomalies such as severe hydrocephaly, and mothers with bad obstetric history are included in other indications.
Obstetric ultrasound and cardiotocography (CTG) machines were used to diagnose maternal and fetal indications such as fetal distress, placenta Previa and abruption, fetal macrosomia, and multiple births. Maternal indications are defined as maternal conditions that could complicate delivery. Fetal distress was defined on cardiotocography (CTG) alone in our setting.
A combination of obstetric ultrasound and vaginal examination by an obstetrician assessing head descent into the pelvic brim before labor was used to diagnose cephalopelvic disproportion.
Statistical analyses were used in the Statistical Package for Social Sciences (SPSS -IBM, Armonk, NY, USA) for Windows, version 26. Data were analyzed using univariate descriptive statistics. The frequencies and percentages, as well as the mean (SD), were presented. Numerical variables were first test for assumption of normality with Shapiro–Wilk test. Binary logistic regression was applied to assess the association between categorical variables and the Cesarean section.
Results
Description of the Study Population
During a 7-year period, there were 12,540 total deliveries. Among these, 2703 were cesarean sections. The mean age of the patients was 26.7±7.3 years [14–44 years]. Most patients were between 20 and 30 years of age (51.3%), followed by the 31–40 years group, who accounted for 36.5%. According to parity, overall deliveries, multiparous mothers constituted 67.7% during the study period. Regarding gestational weeks, 78.6% of deliveries were term, while 21.4% were preterm deliveries. Regarding antenatal visits (ANC), most patients (n=8665, 69%) were unbooked. Table 1 displays the demographic characteristics of the patients.
 |
Table 1 Demographic Characteristics and C-Section Indications of the Study Population |
The Rate of Cesarean Sections, Including a Time Trend
Out of 12,540 deliveries, 2703 were cesarean sections giving an overall cesarean section rate of 21.6%. According to cesarean deliveries, primiparous mothers (55.7%) underwent the maximum number of cesarean sections. Emergency cesarean section was the predominant intervention compared to elective cesarean sections (59.2% vs 40.8%). According to the mode of cesarean sections, primary CS was the most common predominant, while repeat CS increased timely, 77.7% vs 22.3%, respectively.
There were no significant differences in Cesarean section rates over the years during the study period, with the highest C-section performed in 2018 (23.5%) and the lowest C-section performed in 2016 (16.1%) (Figure 1).
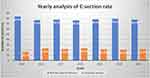 |
Figure 1 Yearly analysis of cesarean section trend. |
Indications for Cesarean Sections
Our cohort analyzed the documented indications for all cesarean sections. Overall, previous cesarean section and fetal distress were the two most common reasons for cesarean delivery (22.3% and 22.1%), respectively. Other indications are listed in Table 1. The five leading causes of maternal indications include previous cesarean sections (22.3%), severe pre-eclampsia (8.7%), prolonged labor (5.8%), Cephalopelvic disproportion (5.8%), and eclampsia (5.3%). Major fetal indications include fetal distress (22.1%), Malpresentation (6.8%), Macrosomia (4.4%), and Multiple gestations (4.2%).
A significant proportion of cesarean sections was performed due to hypertensive diseases of pregnancy, especially severe Preeclampsia and Eclampsia (n=235, 8.7%, n=144, 5.3%), respectively. 314 (83%) of these cases were young Primigravida mothers under 30 years old.
Determinants of Cesarean Sections
Maternal age, parity, gestational weeks, and antenatal visits were significantly associated with the mode of delivery (Normal delivery vs C-sections). The majority of women who gave birth via cesarean section were under 30 years old, primiparous, had term births, and did not receive regular antenatal care. In binary logistic regression analysis, women with maternal age of less than 30 were four and a half times more likely to deliver by cesarean section compared to women over 30 years of age (OR, 4.31; 95% Cl, 3.74–4.98). Similarly, primiparous mothers were three and a half times more likely to deliver by cesarean section compared to multiparous women (OR, 3.59; 95% Cl, 3.29–3.93). According to gestational age, Women with preterm fetuses (<37 weeks) were 90% less likely to undergo C-section (OR, 0.24; 95% Cl, 0.20–0.28) than women with term fetuses. In addition, regarding the antenatal visit, unbooked women were two times more likely to deliver by Cesarean section compared to booked mothers (OR, 2.15; 95% Cl, 1.94–2.39) (Table 2).
 |
Table 2 Determinants of Cesarean Section |
Maternal Mortality
Our cohort revealed a significantly higher maternal mortality rate of about 1.7% (n=216) during the study period. Of 216 maternal deaths, 132 (61%) were due to direct obstetric hemorrhage, including postpartum hemorrhage (n=83, 38.4%), Placenta abruption (n=24, 11.1%), and uterine rupture (n=18, 8.3%). Detailed underlying causes of maternal mortality are shown in (Table 3).
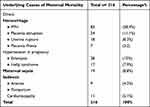 |
Table 3 Maternal Mortality Rate |
Discussion
Cesarean section can significantly reduce maternal and perinatal mortality in appropriate circumstances and should be universally accessible.23 Despite the significant increase in the CS rate worldwide, inadequate access to CS is still a major issue in most Sub-Saharan African countries, including Somalia.10–12 The present is the first hospital-based study that examines the rate, indications, and associated maternal mortality of cesarean deliveries over seven years reported from Somalia. The cesarean section rate of 21.6% observed in the present study is higher than the rate of 10–15% recommended by the WHO in developing countries.13 According to the 2020 Somalia Demographic and Health Survey, the percentage of women who delivered babies by cesarean sections was 2% in a population-based study.4,9 The higher CS rate reported in the present study shows that our hospital is the only referral serving a diverse urban and rural population that usually receives complicated cases, although most births occur at home. Therefore, a much higher incidence of emergency cesarean section is observed compared to elective cesarean section.
A systematic review across 34 SSA countries by Yaya S and associates reported a high prevalence of Caesarean sections in private hospitals compared to public healthcare facilities, with an overall C-section rate of 7.9% in public hospitals and 12.3% in private hospitals, with the highest rate seen in Rwanda about 64.2%.15 Another systematic review and meta-analysis from Ethiopia included 23 cross-sectional studies of 36,705 patients conducted by Gedefaw et al reported an overall pooled Caesarean section rate of 29.55%, which is higher than the rate reported in our study.7
Previous CS is a significant indication of CS worldwide.13 In our study, previous Caesarean section and fetal distress were the two main indications for Caesarean deliveries. These findings are supported by a study by Penn Z, exploring that 30% of C-sections in developed countries were for repeat Caesarean sections.16 Another study in Bangladesh reported that 35% of Caesarean sections were repeated C-sections in governmental hospitals.17 Another review study by Mahadik K found that previous cesarean delivery contributes to rising rates as per evidence from the literature review in the last five years.18 Between 2012 and 2016, the proportion of live births to women with a previous CS increased from 10% to 18% in China, and Brazil reached 27% in 2015. The WHO multi-country studies found a significant proportion of women with a history of CS. Previous CS significantly influences increased CS use, highlighting socioeconomic and other inequalities.5 The American College of Obstetricians and Gynecologists have pointed out that a previous Caesarean section should not be an indication in the absence of any obstetric emergencies.2 In Somalia, most women with prior Caesarean section try normal vaginal delivery at home or at centers for birth attendants in the hands of untrained midwives, which significantly increases the risk of complications, including uterine rupture, and accompanied catastrophes treated with repeat surgery. However, adopting the policy of trial vaginal delivery after a previous cesarean is essential to reduce high CS rates.
Fetal distress was identified as the second leading cause of Caesarean section in this study. This result aligns with the previously reported studies.19–21 This might be due to the availability, reliance, and use of electronic fetal monitoring, a well-equipped neonatal intensive care unit, increased misoprostol tab (Cytotec) for labor induction, and meconium-stained liquor. To avoid performing too many cesarean sections for fetal distress, excellent care, clinical expertise, and knowledge should be used but not delay intervention for a truly compromised fetus.
Due to decades of civil war in Somalia, many health indicators are abysmal.22 According to the Maternal Mortality Estimation Inter-agency Group for Somalia, the MMR in Somalia has reduced from 732 in 2015 to 692 in 2020. Even though this is a reduction, it remains high compared to rates in neighboring countries, such as Kenya (362 per 100,000), Ethiopia (412 per 100,000), and Uganda (336 per 100,000).14 In our study, Two-thirds of MMR were due to direct obstetric hemorrhage, including postpartum hemorrhage, Placenta abruption, and uterine rupture. Trial of labor after previous uterine scar at home, late arrival, and delay of intervention caused by waiting family decisions contributed the most to uterine rupture cases.26,27
Severe Preeclampsia and eclampsia were associated with high maternal morbidity and mortality in our study. A recent study by Omar et al28 revealed that Preeclampsia -eclampsia was the most common cause of postpartum acute kidney injury in Somalia. This might be due to a lack of antenatal care, harmful socio-cultural beliefs, and late referrals.24,25 Therefore, health education, antenatal care, early diagnosis, and prompt referrals need to be improved in Somalia.
This study has certain limitations, including its hospital-based study, and the results may not be generalizable for the whole of Somalia. In addition, the study did not provide data regarding perinatal outcomes. Besides the limitations, the present is the first study that analyses the rate, indications, and associated maternal mortality of cesarean deliveries reported from Somalia.
Conclusion
The study findings showed a slight increase in cesarean delivery rates during the study period. This rate is higher than the 10–15% recommended by the WHO in developing countries. Repeat C-sections and fetal distress were the two most common indications of C-sections in our settings; therefore, reduction of primary C-sections should be given priority, and effective clinical interventions for reducing the primary C-section rate and its associated complications are essential. The data presented in this study can increase the awareness of the maternal care concern among the public and policy-makers, leading to a broad basis of support for the necessary steps to improve reproductive health in Somalia.
Abbreviations
ANC, Antenatal care. CS, Cesarean section; CTG, Cardiotocography; MMR, Maternal Mortality Rate; PPH, Postpartum Hemorrhage; SSA, Sub-Saharan Africa; WHO, World Health Organization.
Data Sharing Statement
Data included in the manuscript.
Institutional Review Board Statement
The Mogadishu Somalia Turkish Training and Research Hospital Clinical Research Ethics Committee were approved for this study (approval number MSTH/7892). All methods were performed in accordance with the relevant guidelines and regulations.
Informed Consent Statement
All study participants and a parent of participants under 18 years of age previously consented to use their medical and surgical data in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare that this study has not received any funding resources.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Managing Complications in Pregnancy and Childbirth. Integrated Management of Pregnancy And Childbirth; 2017:390.
2. Begum A. Indications and determinants of caesarean section delivery in Matlab, Bangladesh. PLoS One. 2017;12(11):1–16. doi:10.1371/journal.pone.0188074
3. Schantz C, Ravit M, Traoré AB, et al. Why are caesarean section rates so high in facilities in Mali and Benin? Sex Reprod Healthc. 2018;16:10–14. doi:10.1016/j.srhc.2018.01.001
4. Bishop D, Dyer RA, Maswime S, et al. Maternal and neonatal outcomes after caesarean delivery in the African Surgical Outcomes Study, a 7-day prospective observational cohort study. Lancet Glob Heal. 2019;7(4):e513–e522.
5. Boerma T, Ronsmans C, Melesse DY, et al. Series Optimising caesarean section use 1 Global epidemiology of use of and disparities in caesarean sections. Lancet. 2018;392(10155):1341–1348. doi:10.1016/S0140-6736(18)31928-7
6. Geidam AD, Audu BM, Kawuwa BM, Obed JY. Rising trend and indications of caesarean section at the university of Maiduguri teaching hospital, Nigeria. Ann Afr Med. 2009;8(2):127–132. doi:10.4103/1596-3519.56242
7. Gedefaw G, Demis A, Alemnew B, Wondmieneh A, Getie A, Waltengus F. Prevalence, indications, and outcomes of caesarean section deliveries in Ethiopia, A systematic review and meta-analysis. Patient Saf Surg. 2020;14(1):1–10. doi:10.1186/s13037-020-00236-8
8. Chu K, Cortier H, Maldonado F, Mashant T, Ford N, Trelles M. Cesarean section rates and indications in Sub-Saharan Africa, a multi-country study from medecins sans frontieres. PLoS One. 2012;7(9):5–10. doi:10.1371/journal.pone.0044484
9. Ronsmans C, Holtz S, Stanton C. Socioeconomic differentials in caesarean rates in developing countries, a retrospective analysis. Lancet. 2006;368(9546):1516–1523. doi:10.1016/S0140-6736(06)69639-6
10. Gao Y, Xue Q, Chen G, Stone P, Zhao M, Chen Q. An analysis of the indications for cesarean section in a teaching hospital in China. Eur J Obstet Gynecol Reprod Biol. 2013;170(2):414–418. doi:10.1016/j.ejogrb.2013.08.009
11. Temmerman M, Mohiddin A. Cesarean section, More than a maternal health issue. PLoS Med. 2021;18(10):10–12. doi:10.1371/journal.pmed.1003792
12. Sobhy S, Arroyo-Manzano D, Murugesu N, et al. Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries, a systematic review and meta-analysis. Lancet. 2019;393(10184):1973–1982. doi:10.1016/S0140-6736(18)32386-9
13. Statement T. WHO Statement on Caesarean Section Rates €; 2015:667–670.
14. Federal Republic of Somalia. Somali Health and Demographic Survey 2020; 2020.
15. Yaya S, Uthman OA, Amouzou A, Bishwajit G. Disparities in caesarean section prevalence and determinants across sub-Saharan Africa countries. Glob Heal Res Policy. 2018;3(1):1–9.
16. Penn Z, Ghaem-Maghami S. Indications for caesarean section. Best Pract Res Clin Obstet Gynaecol. 2001;15(1):1–15. doi:10.1053/beog.2000.0146
17. Aminu M, Utz B, Halim A, Van Den BN. Reasons for performing a caesarean section in public hospitals in rural Bangladesh. BMC Pregnancy Childbirth. 2014;14:1–8. doi:10.1186/1471-2393-14-130
18. Mahadik K. Rising Cesarean Rates, Are Primary Sections Overused? J Obstet Gynecol India. 2019;69(0123456789):483–489. doi:10.1007/s13224-019-01246-y
19. Ozturk M. Cesarean section rates and indications in turkey, a systematic review and cesarean section rates and indications in Turkey, a systematic review and meta-analysis. AJRNH. 2021;4(4):31–57.
20. Waniala I, Nakiseka S, Nambi W, et al. Prevalence, indications, and community perceptions of caesarean section delivery in Ngora District, eastern Uganda, mixed method study. Obstet Gynecol Int. 2020;2020:1–11. doi:10.1155/2020/5036260
21. Belizán JM, Minckas N, McClure EM, et al. An approach to identify a minimum and rational proportion of caesarean sections in resource-poor settings, a global network study. Lancet Global Health. 2018;6(8):e894–e901. doi:10.1016/S2214-109X(18)30241-9
22. Somali Federal Ministry of Health. Somali Federal Ministry of Health. Second phase of health sector strategic plan 2017–2021. Somalia Mogadishu. 2017;66:1–79.
23. Ye J, Zhang J, Mikolajczyk R, Torloni MR, Gülmezoglu AM, Betran AP. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century, a worldwide population-based ecological study with longitudinal data. BJOG. 2015;123:745–753. doi:10.1111/1471-0528.13592
24. Abdullah A, Shaikh AA, Jamro B. Maternal and perinatal outcome associated with eclampsia in a teaching hospital, Sukkur. Rawal Med J. 2010;35(1):23–26.
25. Irene K, Amubuomombe PP, Mogeni R, Andrew C, Mwangi A, Omenge OE. Maternal and perinatal outcomes in women with eclampsia by mode of delivery at Riley mother baby hospital, a longitudinal case-series study. BMC Pregnancy Childbirth. 2021;21(1):1–14. doi:10.1186/s12884-021-03875-6
26. Omer Handady S, Hassan Sakin H, Alawad AM. Uterine rupture, a review of 15 cases at bandier maternity hospital in Somalia. Clin Obstet Gynecol Reprod Med. 2015;1(2):55–58. doi:10.15761/COGRM.1000115
27. Getahun WT, Solomon AA, Kassie FY, Kasaye HK, Denekew HT. Uterine rupture among mothers admitted for obstetrics care and associated factors in referral hospitals of Amhara regional state, institution-based cross-sectional study, Northern Ethiopia, 2013–2017. PLoS One. 2018;13(12):1–14. doi:10.1371/journal.pone.0208470
28. Omar NM, Osman MM, Hilowle IA, et al. Demographic characteristics and risk factors affecting the development of postpartum acute kidney injury in Somalia, single-center experience. Int J Women’s Health. 2022;14:881. doi:10.2147/IJWH.S372453
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
