Back to Journals » Clinical Ophthalmology » Volume 16
An All-Digital, Binocular, Indirect Virtual Video Ophthalmoscope: A Novel Approach to Retinal Examination and Photography
Authors Solyman O , Aref A , Abo Obaia AS, Kamel HF, Al-Muhaylib A
Received 18 October 2022
Accepted for publication 14 November 2022
Published 24 November 2022 Volume 2022:16 Pages 3905—3909
DOI https://doi.org/10.2147/OPTH.S393892
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Supplementary video of "An all-digital virtual video BIO" [ID 393892].
Views: 176
Omar Solyman,1 Amr Aref,1 Ahmed S Abo Obaia,1 Hesham F Kamel,1 Ahmed Al-Muhaylib2
1Department of Ophthalmology, Research Institute of Ophthalmology, Giza, 12211, Egypt; 2Department of Ophthalmology, School of Medicine, Qassim University, Al-Qassim, Saudi Arabia
Correspondence: Omar Solyman, Department of Ophthalmology, Research Institute of Ophthalmology, Giza, 12211, Egypt, Email [email protected]
Purpose: We describe a novel method of digital, virtual-reality based binocular indirect ophthalmoscopy which allows for simultaneous stereoscopic recording of the examination with the potential of real-time anatomic correction of the retinal view.
Materials and Methods: A provisional prototype of the all-digital, binocular, indirect virtual stereo video ophthalmoscope was designed consisting of a generic LED light source and two synchronized closely spaced side-by-side minicameras which are connected to a processor, storage media (a Samsung note-9 android smartphone in the current provisional prototype), and a virtual reality set (VISIONHMD Bigeyes H1 3D Video Glasses, in the current prototype). A custom designed android application was developed to capture the examination media and allow optional real-time anatomical correction of the examination view. Binocular stereoscopic indirect ophthalmoscopy was attempted on 15 eyes of 15 patients without and with digital real-time anatomic correction of the examination view.
Results: Binocular, video, stereo ophthalmoscopic media could be successfully obtained in all 15 patients. Anatomic correction of the examination view as well as a collateral observer’s view could be achieved in all 15 patients.
Conclusion: An all-digital, binocular, stereo, video indirect ophthalmoscopy is a feasible alternative for conventional binocular indirect ophthalmoscopy and provides stereoscopic video documentation identical to what the examiner sees. The examination video can be streamed in the real-time of the examination for educational or telemedicine purposes.
Keywords: indirect ophthalmoscopy, fundus examination, retinal imaging, telemedicine, medical education
Introduction
Since the introduction of the modern self-luminous binocular indirect ophthalmoscope (BIO) in the mid-20th century, enhancements have been directed mainly to improve illumination without much change in the core optical system.1,2 The optical principle of BIO depends on the reduction of the interpupillary distance (IPD) of the examiner by means of mirrors and/or prisms to allow the examiner’s visual axes of both eyes to simultaneously receive light rays bouncing back through the patient’s pupil. Light rays coming back from the ocular fundus are collimated by indirect ophthalmoscopy lens to form a real, inverted and laterally reversed image between the patient and the examiner. Performing and anatomically interpreting a BIO examination is a skill which ophthalmology trainees develop during their residency training programs.3 Conventional BIOs are not capable of capturing videos and images of the examination. Video enabled BIO devices are commercially available at a higher cost, are bulkier and allow 2D capturing of videos and still images of the ophthalmoscopy examination by means of an integrated digital camera4–6 The limitations of currently available video enabled BIO devices include possible decentration of the captured image from the view of the examiner that requires frequent adjustments4 and the lack of stereovision of the recordings as they provide two dimensional (2D) rather than stereoscopic 3D images. Herein, we describe a novel design of an all-digital video recording enabled BIO prototype that provides stereoscopic three dimensional (3D) recording of the ocular fundoscopy image with the potential of real-time anatomical correction.
Methods
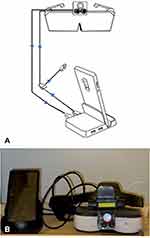
This prospective observational pilot study was approved by the human research ethics committee of the Research Institute of Ophthalmology, Giza, Egypt, and was performed in accordance with all local laws and in compliance with the principles of the Declaration of Helsinki. A written informed consent was obtained from all study participants. The prototype used in this study consists of a generic LED light source and two synchronized 15 mm apart side-by-side minicameras. The minicameras are connected to a processor, storage media (a Samsung note-9 android smartphone in the current prototype), and a virtual reality set (VISIONHMD Bigeyes H1 3D Video Glasses, in the current prototype) (Figure 1). The synchronized dual cameras were configured to export their captured video to the Samsung note-9 phone by means of a connecting console (Samsung Dex Dock Station). A custom-made android application was designed to capture the examination media from the dual camera so that the right camera projects to the right half of the screen and the left camera projects to the left half of the screen to create a side-by-side stereogram. The software also allows optional real-time anatomic correction of the examination view by touching a screen button or via a wired remote shutter. Examination media are then projected to the virtual reality set so that the image of the right camera is projected to the right side of the virtual reality glasses and is seen by the examiner’s right eye and the left image from the left camera is projected to the left side of the virtual reality glasses and is seen by the examiner’s left eye.
The prototype was first tested and adjusted on three different schematic eyes including Ocular Imaging Eye Model (Ocular Instruments inc. Bellevue, WA, USA), RetCam Digital Retinal Camera Practice Kit (Massie Research Laboratories Inc., Pleasanton, CA, USA), and Reti Eye Model (Gulden Ophthalmics, Elkins Park, PA, USA). The LED light was tested for its safety to the human eye in terms of light intensity and spectrum. Light intensity was 3.8 mW/cm2 (safe limits are at least 1 order of magnitude below the safety limit set by the ISO15004-2.2 which is 706 mW/cm2)7,8 and light spectrum fell entirely in the safe visible spectrum with no ultraviolet or infrared composition.
Binocular, stereoscopic indirect ophthalmoscopy was then attempted on 15 eyes of 15 patients in a dim light condition after dilation of the pupils with Tropicamide 1% eyedrops without and with digital real-time anatomic correction of the examination view. Collateral video output was attempted to another virtual reality set for observers to view in 10 patients and to an outside monitor in 5 patients.
Results
Binocular, virtual, stereoscopic indirect ophthalmoscopic examination could be successfully tested on the three schematic model eyes using this prototype in conjunction with a +20 diopter indirect ophthalmoscopy lens.
Binocular video stereo ophthalmoscopic media could be obtained in all patients (n = 15). Anatomic correction of the examination view was achieved in all patients (n = 15) (Figure 2 and Supplementary Video). A collateral educational view could be simultaneously streamed in all patients either to another set of virtual reality glasses (10 patients out of 10) and to a monitor screen (5 patients out of 5).
 |
Figure 2 Indirect retinal photography showing (A) optic disc, (B) macular, and (C) peripheral retinal pathologies. |
Discussion
The aim of this work was to investigate the feasibility of indirect binocular ophthalmoscopy using a newly designed all-digital, binocular indirect ophthalmoscope that replaces the conventional optical system of BIO by two side-by-side minicameras. This achieves the goal of decreasing the examiner’s IPD and allowing virtual binocular indirect simultaneous visualization through the pupil of the subject and projects two images of the ocular fundus view to the corresponding screen of a virtual reality set. This allows the examiner to see the ocular fundus virtually and binocularly in real-time.
Conventional BIOs are not capable of recording the examination in pictures or videos. Video enabled BIOs are available at markedly higher cost, are bulkier in size, provide 2D recordings and may be limited by the decentration of the view of the camera relative to the examiner’s view that requires frequent adjustments.4 In our design, the video examination of the ocular fundus seen by the examiner is simultaneously recorded in stereoscopic 3D side-by-side format.
The image of the ocular fundus seen by the examiner is inverted and laterally reversed relative to the real anatomic orientation in conventional BIO examination.1 Using our described design, anatomic correction of the view of the examination is achievable during the real-time examination by digitally horizontally reversing and vertically inversing each of the two side-by-side images of the ocular fundus examination. Although the skill of anatomical interpretation of the BIO image is usually mastered during the residency training years,3 providing the option of an anatomically corrected view may make this part of a BIO examination more convenient.
Ophthalmology trainees can observe the ophthalmoscopy examination findings through an accessory teaching mirror attached to the front of the conventional BIO devices. These teaching mirrors provide a 2D image of the examiners view9 that can be seen by the trainee in a narrow window between the examiner and the patient which may be inconvenient to the patient. In video enabled BIOs, trainees can watch the examination findings in 2D in real-time or after the examination on a connected monitor.5 Kong et al, described using two accessory cameras with the conventional BIO to provide the trainees with a 3D view.10 This makes the BIO bulkier, heavier to put on and does not prevent decentration of the trainees’ view from the view seen by the examiner. Our design provides the ophthalmology trainees with a real-time stereoscopic 3D view of the ophthalmoscopy identical to the view seen by the examiner. The examination can also be captured in 2D or in 3D for documentation and for clinical education. Limitations of our current provisional prototype include the use of commercially available affordable minicameras and virtual-reality headset since our aim at this point was just to prove the concept. We think that the view can be made superior to this and the device can be more compact if the minicameras can be upgraded and custom-designed.
Conclusion
We describe a novel design of a video recording enabled BIO device that replaces the complex optical system of conventional BIO with two closely placed side-by-side minicameras. Advantages of this novel design include optional real-time anatomic correction of the examiner’s view of the ocular fundus and optional identical recording of the examiner’s BIO view in stereoscopic 3D as well as in 2D which can enhance clinical documentation and education.
Data Sharing Statement
Data used in this study is available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This report was approved by the Research Institute of Ophthalmology Research Ethics Committee and followed the tenets of the Declaration of Helsinki. A written informed consent was obtained from all participating patients.
Acknowledgments
The design described in this article is related to a pending international patent for Dr Omar Solyman (PCT # PCT/US2021/071604).
Funding
There is no funding to report.
Disclosure
Dr Omar Solyman initiated a start up of ophthalmology related hardware and software solutions for Wadjet: the Eye Gadget. The design of the prototype described in this article is related to a pending international patent for Dr Omar Solyman (PCT # PCT/US2021/071604). The authors report no other conflicts of interest in this work.
References
1. Brockhurst RJ, Tour RL. Modern indirect ophthalmoscopy. Am J Ophthalmol. 1956;41(2):265–272. doi:10.1016/0002-9394(56)92021-9
2. Kothari M, Kothari K, Kadam S, Mota P, Chipade S. Converting a conventional wired-halogen illuminated indirect ophthalmoscope to a wireless-light emitting diode illuminated indirect ophthalmoscope in less than 1000/- rupees. Indian J Ophthalmol. 2015;63(1):42–45. doi:10.4103/0301-4738.151466
3. Rai AS, Rai AS, Mavrikakis E, Lam WC. Teaching binocular indirect ophthalmoscopy to novice residents using an augmented reality simulator. Can J Ophthalmol J Can Ophtalmol. 2017;52(5):430–434. doi:10.1016/j.jcjo.2017.02.015
4. Vantage Plus Digital Instructions Manual . Available From: https://support.keeler-global.com/_manuals/Indirect%20Ophthlmoscopes/Vantage%20Plus%20Digital%20(EP59-09863-art-F)/EP59-09863-art-F.pdf.
5. Sridhar J, Shahlaee A, Mehta S, et al. Usefulness of structured video indirect ophthalmoscope-guided education in improving resident ophthalmologist confidence and ability. Ophthalmol Retina. 2017;1(4):282–287. doi:10.1016/j.oret.2016.12.010
6. Ho T, Lee TC, Choe JY, Nallasamy S. Evaluation of real-time video from the digital indirect ophthalmoscope for telemedicine consultations in retinopathy of prematurity. J Telemed Telecare. 2020;1357633X20958240. doi:10.1177/1357633X20958240
7. Solyman OM, Hamdy O, Abdelkawi SA, Hassan AA. Investigating the light emitting diode (LED) flashlight characteristics of a sample of smartphones for its safety in indirect retinal photography. Pan Afr Med J. 2022;43:15. doi:10.11604/pamj.2022.43.15.32963
8. Hong SC, Wynn-Williams G, Wilson G. Safety of iPhone retinal photography. J Med Eng Technol. 2017;41(3):165–169. doi:10.1080/03091902.2016.1264491
9. Saunders RA, Bluestein EC, Berland JE, Donahue ML, Wilson ME, Rust PF. Can non-ophthalmologists screen for retinopathy of prematurity? J Pediatr Ophthalmol Strabismus. 1995;32(5):302–304; discussion 305. doi:10.3928/0191-3913-19950901-08
10. Kong HJ, Cha JP, Seo JM, Hwang JM, Chung H, Kim HC. Development of cold light indirect ophthalmoscopic video system for sharing stereopsis. Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Int Conf. 2007;2007:2219–2222. doi:10.1109/IEMBS.2007.4352765
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.