Back to Journals » Local and Regional Anesthesia » Volume 10
Ambulatory thyroidectomy: an anesthesiologist’s perspective
Authors Murray B, Tandon S, Dempsey G
Received 21 December 2016
Accepted for publication 21 February 2017
Published 5 April 2017 Volume 2017:10 Pages 31—39
DOI https://doi.org/10.2147/LRA.S111554
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Stefan Wirz
Benjamin Murray,1 Sankalap Tandon,2 Ged Dempsey1
1Department of Anaesthesia and Critical Care, 2Department of Otolaryngology, Head & Neck Surgery, Aintree University Hospital NHS Foundation Trust, Liverpool, UK
Abstract: Thyroidectomy has been performed on an inpatient basis because of concerns regarding postoperative complications. These include cervical hematoma, bilateral recurrent laryngeal nerve injury and symptomatic hypocalcemia. We have reviewed the current available evidence and aimed to collate published data to generate incidence of the important complications. We performed a literature search of Medline, EMBASE and the Cochrane database of randomized trials. One hundred sixty papers were included. Twenty-one papers fulfilled inclusion criteria. Thirty thousand four hundred fifty-three day-case thyroid procedures were included. Ten papers were prospective and 11 retrospective. The incidences of complications were permanent vocal cord paralysis 7/30259 (0.02%), temporary hypocalcemia 129/4444 (2.9%), permanent hypocalcemia 405/29203 (1.39%), cervical hematoma 145/30288 (0.48%) and readmission rate 105/29609 (0.35%). Analysis of cervical hematoma data demonstrated that in only 3/14 cases the hematoma presented as an inpatient, and in the remaining 11/14, it occurred late, with a range of 2–9 days. There is a paucity of data relating to anesthetic techniques associated with ambulatory thyroidectomy. Cost comparison between outpatient and inpatient thyroidectomy was reported in three papers. Cost difference ranged from $676 to $2474 with a mean saving of $1301 with ambulatory thyroidectomy. There is a body of evidence that suggests that ambulatory thyroidectomy in the hands of experienced operating teams within an appropriate setting can be performed with acceptable risk profile. In most circumstances, this will be limited to hemithyroidectomies to reduce or avoid the potential for additional morbidity. We have found little evidence to support the use of one anesthetic technique over another. The rates of hospital admission and readmission related to anesthetic factors appear to be low and predominantly related to pain and postoperative nausea and vomiting. A balanced anesthetic technique incorporating appropriate analgesic and antiemetic regimens is essential to avoid unnecessary hospital admission/readmission.
Keywords: ambulatory, day case, same day, thyroidectomy, hemithyroidectomy
Introduction
Thyroidectomy has long been performed on an inpatient basis primarily because of concerns regarding postoperative complications, the most feared of which is airway compromise due to postoperative bleeding or recurrent laryngeal nerve (RLN) palsy. Routine practice has previously included hospital inpatient stays of multiple days.1 With improved patient selection and surgical techniques, the length of hospital stay has gradually reduced, particularly through the early part of this century.2 The complications that have resulted in thyroidectomy remaining predominantly an inpatient procedure have largely been surgical; the risk of airway compromise because of cervical hematoma and bilateral RLN injury and symptomatic hypocalcemia due to inadvertent parathyroid injury or removal.2 Proponents of same-day thyroidectomy believe that these complications can be minimized through robust surgical technique and operative pathways and assessment.2,3 Since the 1990s there have been a small but significant number of authors who have reported same-day thyroidectomy.4,5
Opinions as to the safety and benefits of day-case thyroidectomy differ. The British Association of Endocrine and Thyroid Surgeons (BAETS) commissioned a review in 2012 concluding that “Same day discharge in a UK setting cannot be endorsed. Any financial benefits may be outweighed by the exposure of patients to an increased risk of an adverse outcome. Consequently, 23-hour surgery is recommended”.6 The European Association Francophone De Chirurgie Endocrinienne has also recommended a “standard hospital stay including an overnight stay”.7 A different view, however, has been taken by the American Thyroid Association which stated “Outpatient thyroidectomy may be undertaken safely in a carefully selected patient population provided that certain precautionary measures are taken to maximize communication and minimize the likelihood of complications”.8 The differing opinions proffered by these surgical bodies may partly reflect the health care systems prevalent within their areas of practice.
Due to the current contradictory advice as to the safety of day-case thyroidectomy and the varied definitions of “day case” and “ambulatory”, we have reviewed the current available evidence relating to both anesthetic and surgical complications. We aimed to collate published data to enable the incidence of the important complications to be estimated. We also aimed to assess the impact of anesthetic technique used upon the ability to perform same-day thyroid surgery. The cost implications of the different approaches and the common inclusion and exclusion criteria used in patient selection will also be included.
Methods
We performed a literature search of Medline, EMBASE and the Cochrane database of randomized trials using www.evidence.nhs.uk from National Institute for Health and Care excellence (NICE–UK). To more accurately reflect contemporary practice, only studies published from 2000 onward were included. The study selection flow chart is presented in Figure 1. We searched using the key words, thyroidectomy, hemithyroidectomy, ambulatory surgical procedures, day case and same day. We defined day-case surgery as that which resulted in the patient being discharged on the same calendar day (i.e., no overnight stay). Consequently, papers with differing definitions, including those in which a day case was defined as <24 hours in hospital, were excluded. For the purpose of calculating the incidence of complications, we only included papers with data specific to said complication and procedure – we excluded data from papers if we were unable to separate composite outcomes from a number of differing operations (e.g., para-thyroidectomy and hemithyroidectomy). Our search was focused on complications that would prevent same-day discharge: cervical hematoma requiring operative intervention, RLN injury, permanent hypocalcemia, temporary hypocalcemia, anesthetic-related complications and readmission rate. Vocal cord paralysis was considered permanent if follow-up had not taken place or if follow-up demonstrated an ongoing deficit. The definition of temporary and permanent hypocalcemia was frequently not stated.
  | Figure 1 Study selection flow-chart. |
Results
Initial search revealed a total of 160 papers that were considered for inclusion. Of these, 21 papers fulfilled our inclusion criteria. A total of 30,453 day-case thyroid procedures were studied by the included papers. Ten papers were prospective and 11 retrospective. Of the included papers, one paper, by Orosco et al, accounted for 25,634 of 30,453 (84%) included cases. We attempted to separate the data to give the incidence of complications for both retrospective and prospective series respectively. This proved impossible to achieve as some papers reported both prospective and retrospective data. The operations included are summarized as hemithyroidectomy, completion thyroidectomy and total thyroidectomy. We also aimed to report complication rates by operation but were unable to do so as some papers were not explicit as to the actual operation performed. In some papers, data for completion thyroidectomy were included with total thyroidectomy, and in others it was included with hemithyroidectomy. For example, when assessing hypocalcemia completion, thyroidectomy was considered part of the total thyroidectomy group. However, in papers assessing cervical hematoma, they were grouped with hemithyroidectomy. Hemithyroidectomy/unilateral surgery accounted for 16,891 (55.6%) and total/bilateral surgery accounted for 13,504 (44.4%) of procedures.
The overall incidences of complications were permanent vocal cord paralysis 7/30259 (0.02%), temporary hypocalcemia 129/4444 (2.9%), permanent hypocalcemia 405/29203 (1.39%), cervical hematoma 145/30288 (0.48%) and readmission rate 105/29609 (0.35%; Table 1). One patient planned for ambulatory thyroidectomy suffered bilateral vocal cord palsy requiring reintubation. This was immediately apparent at extubation.3 One patient, a nursing-home resident, died two days after a total thyroidectomy from a perioperative cardiac event.2
Further analysis of the cervical hematoma data looking specifically at the timing of presentation demonstrated that in only 3/14 cases (where timing information is available) the hematoma presented as an inpatient, and in the remaining 11/14, it occurred late, with a range of 2–9 days.
There is a paucity of data relating to anesthetic techniques associated with ambulatory thyroidectomy. Of the papers included in this analysis, only Snyder et al 20069 studied anesthetic techniques. He performed a randomized control trial of 60 patients undergoing thyroidectomy with general anesthesia (GA) versus local anesthesia (LA) with sedation. Surgical procedures included both hemithyroidectomy and total thyroidectomy in each group. Time spent in hospital was significantly (p=0.2) less in the LA group. However, rates of nausea and vomiting were not significantly different but patients undergoing GA had more frequent administration of antiemetics. Nonanesthetic complication rates did not vary between the two groups. Within the remaining papers, complications that could be attributed to anesthetic factors were not widely reported. Of those that were reported, the most common were pain and nausea. Unplanned admission due to anesthetic factors was reported in four papers with a total of 30/334 (9%) patients requiring unexpected admission (Table 1).10–13 Readmissions due to anesthetic factors were reported in three papers (Table 1).14–16 A total of 221/25947 (0.85%) patients required readmission.
As stated above, there was one perioperative death in 30,453 (0.003%) cases, which was unrelated to any surgical or anesthetic complication.
All 21 papers required the patients to undergo preoperative assessment. This was performed in different ways, including preoperative questionnaire, preoperative nurse-led clinic, preoperative anesthetic clinic, preoperative surgical clinic or a variable combination of each. All studies only allowed patient discharge in the presence of a responsible adult. Although this is standard practice, no paper commented whether the responsible adult was expected to regularly check on the patient or be in the same room. Patient education was undertaken in most centers prior to surgery. This included documentation explaining complications and contact details to raise concerns and aid prompt identification of any potential problems.
Cost comparison between outpatient and inpatient thyroidectomy was reported in three papers.1,13,17 In all cases outpatient care was cost effective. Cost difference ranged from $676 to $2474 with a mean saving of $1301 with ambulatory thyroidectomy.
Further detail of the data collected from the papers including demographic data can be found in Table 1. We have included a summary of the themes used in the criteria for ambulatory thyroidectomy. These can be found in Table 2. Further information on potential barriers to same-day discharge is summarized in the 2014 paper by Rutledge et al.18
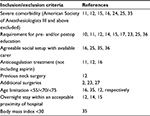  | Table 2 Assessment of patient suitability for ambulatory thyroidectomy |
Discussion
We have analyzed all the papers that fulfilled our search criteria with the aim of generating an incidence of the common complications that occur following ambulatory thyroidectomy. We have attempted to analyze the different techniques employed to minimize the complications. We attempted to generate separate incidences for both total thyroidectomy and hemithyroidectomy but were unable to do because of selective reporting within the papers reviewed. The mortality rate from the incorporated papers was 0.003% (1 in 30,453), and this was related to a postoperative cardiac event. One patient suffered bilateral vocal cord palsy requiring tracheal reintubation, which was identified immediately postoperatively.
Hematoma
Cervical hematoma is arguably the most serious of the complications, which has led to the resistance in performing thyroidectomy as a same-day procedure. The risk of airway compromise has led to a short inpatient stay to be traditionally advocated.2 Our analysis has produced an incidence of 145/30288 (0.48%) for cervical hematoma. This is similar to previously reported rates in the paper by Bononi et al from 2009. They collated cervical hematoma rates from multiple papers giving an incidences range between 0 and 1.6%. Both Burkey et al19 and Leyre et al20 have studied the incidence of cervical hematoma demonstrating that 40%–50% occur within 6 hours of the operation, a further 40% will manifest between 7 and 24 hours and the remaining 10%–20% will present beyond 24 hours. Using these percentages, monitoring patients for up to 24 hours enabled 80%–90% of cervical hematoma to occur in hospital where prompt treatment to minimize harm was possible.2 Analysis of historical outcome data by Schwartz et al predicted that for every 100,000 thyroidectomies performed, 94 deaths secondary to postoperative bleeding could be prevented by 24-hour hospitalization, compared with 6-hour observation.21 Bononi et al later quoted the timings from Schwartz’s paper and stated that the recommended 24-hour stay does “not offer the safety margin required”.22 Although the percentages from the Schwartz et al paper are useful, in order to assess suitability to change from a policy of hospital discharge at 24 hours to discharge at 6 hours, further analysis of cervical hematoma rates between 7 and 12 hours postoperatively would allow a more comprehensive risk assessment for earlier discharge. Subgroup analysis from our data set of patients who suffered cervical hematoma (where information on the timing was available) demonstrated that in 11 out of the 14 cases reported, the hematoma presented after two or more days (range: 2–9 days). Therefore, all 11 of these patients would have developed their cervical hematoma after hospital discharge even if this occurred at 24 hours postoperatively. From the evidence available currently, it would appear that the timing of this complication is unpredictable with poorly defined risk factors – none of the papers cited describing definite perioperative risk stratification to predict the occurrence of cervical hematoma.19
Recurrent laryngeal nerve injury
The incidence of permanent vocal cord paralysis in this analysis was found to be 7/30259 (0.02%). There were two main techniques described within the papers reviewed to assess RLN function. Continuous monitoring using electromyography was the only intraoperative means of assessment of RLN function and integrity described. RLN function was otherwise assessed pre- and postoperatively, at varying time intervals, by direct or indirect laryngoscopy. Only Mazeh et al23 did not perform any assessment of RLN function. In two studies,12,24 assessment was only performed if there was a specific clinical indication such as change in voice.
The primary concern with RLN injury is related to bilateral injury resulting in unopposed vocal cord adduction leading to airway obstruction. Only one paper reported an incidence for bilateral RLN palsy (one patient).10 Given the serious nature of bilateral RLN palsy as a serious complication it seems fair to assume that it would be reported in a paper. There appears to be only one case of bilateral RLN palsy giving an estimated incidence of 1 in 13504 (0.007%) total thyroidectomies performed. The case could be made for completion thyroidectomy to be added to the denominator; however, we were unable to separate the completion thyroidectomy cases as some papers included them with hemi-thyroidectomy, and others with the total thyroidectomy. As such we recognize the incidence of 0.007% as an estimate.
While unilateral injury will not usually cause airway obstruction, it may alter voice and lead to increased risk of aspiration.2 As stated above, the incidence of permanent RLN injury is very small at 0.02%. However, nerve injury is transient in the great majority of cases.13 We were, however, unable to quantify an incidence for transient paralysis or neuropraxia. There is a wide spectrum of symptoms over variable time frames included under the umbrella term temporary RLN injury that formulating an acceptable definition to allow data collection from different studies is problematic.
Hypocalcemia
Hypocalcemia is a common cause for hospitalization after thyroid surgery.25 In this analysis, we split results between temporary and permanent hypocalcemia. The respective incidences were 129/4444 (2.9%) for temporary hypocalcemia and 405/29203 (1.39%) for permanent hypocalcemia. Rates of temporary hypocalcemia have previously been reported as high as 40%.26 Rates in more recent papers are, however, significantly lower.2,26,27 This reduction has been attributed to improved surgical technique, parathyroid implantation, postoperative calcium supplementation and calcium and/or parathyroid hormone (PTH) measurement with protocols for supplementation. Although hypocalcemia can occur in any thyroid procedure, the highest risk procedures for this complication were the total and completion thyroidectomies. In this analysis, on only one occasion did a patient undergoing hemithyroidectomy require treatment for symptomatic hypocalcemia.10
Management of hypocalcemia was predominantly split between three techniques. 1) Measuring either calcium or PTH, 2) giving patients undergoing total or completion thyroidectomy oral calcium supplementation in the postoperative period and 3) neither treating nor measuring calcium or PTH so called “watchful waiting”. The majority of papers managed hypocalcemia risk by discharging patients on oral calcium supplementation with or without vitamin D. Most authors advocating this approach have regarded it a cost-effective and safe method of prophylaxis. It does, however, result in a proportion of patients being treated that would never have gone on to develop symptomatic hypocalcemia. Consequently, protocols using rapid (within 6 hours) PTH measurement have been developed and evaluated. Three papers23,26,27 used PTH-based discharge algorithms and all felt these facilitated safe ambulatory thyroidectomy. Both Houlton26 and Payne27 utilized PTH-based algorithms to discharge completion and total thyroidectomies on the day of surgery. Table 3 summarizes the different techniques used to avoid hypocalcemia.
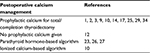  | Table 3 Different techniques used to prevent and manage hypocalcemia postoperatively and the papers that used each |
Readmission rate
The readmission rate from the composite data we have collected is 105/29609 (0.35%). This is in the lower range of the 0%–2.6% incidence described previously.2,10,15,28–31 Somewhat surprisingly, the definition of hospital readmission varied across the papers studied. Some papers considered a readmission as patients requiring inpatient stay, and others included patients who were seen and treated, but not admitted. It is highly likely that there are cases incorporated in our analysis that were readmitted to a hospital other than that in which the surgery was undertaken. Such cases, therefore, will not be included in our analysis.
Anesthetic technique
Within the bounds of this search we have found very little information assessing anesthetic techniques and their effect on the ability to perform ambulatory thyroidectomy. Readmission rates that could be attributed to anesthetic factors were found in 30/334 (9%)10–13 cases, with unplanned admissions attributed to anesthetic factors at 221/25947 (0.85%).14–16 Only Snyder et al,9 in their 2006 paper, compared GA with LA techniques. They reported no difference in postoperative adverse outcomes, complications, patient admissions or patient satisfaction but did report a reduced in-hospital time and a possible cost saving with the LA technique.9 A standardized general anesthetic technique was described in the papers by Champault et al12 and Sklar et al.16 The remaining papers analyzed either allowed a nonstandardized anesthetic technique or made no reference to the anesthetic technique employed. Bononi et al, in their 2009 paper, assessed postoperative vomiting and found no relationship between emesis and cervical hematoma formation.22 Other anesthetic-specific techniques described included laryngeal nerve monitoring,1,25 deep tracheal extubation to prevent coughing on emergence,25 postoperative RLN function assessment either before waking in theater or using flexible endoscopy in the postsurgical unit.2
Therefore, reviewing the available evidence, there does not appear to be a preferred anesthetic technique for ambulatory thyroidectomy. There may be a reduction in postsurgical time with an LA and sedation technique. However, given that the most prominent anesthetic factors related to readmission and unplanned admission were postoperative nausea and vomiting and poor pain control, meticulous attention paid to these aspects of anesthetic care should help to reduce in-hospital time and facilitate prompt discharge.
Cost
Cost is a well-understood driver to increase the proportion of elective surgery performed on an ambulatory basis. This is independent of the type of health care system the procedure is being performed in. Three papers in this analysis by Terris et al1, Lacroix et al13 and Narayanan et al17 briefly discussed cost difference between inpatient and outpatient thyroid surgery. In all three reports, outpatient care conferred a significant cost saving. Savings ranged from $676 to $2474 with a mean value of $1301. In a paper entitled “Better value in the NHS: The role of changes in clinical practice”, The Kings Fund stated “As day case patients cost less to treat than patients who stay overnight as inpatients (in 2013–14, the average day case cost was $698 and the average elective inpatient case $3375), the increasing proportion of day case activity has helped reduce overall costs”.32 Marino et al when assessing the cost of outpatient thyroidectomy in US academic medical centers quoted charges of $20,510 for inpatient and $14,796 for outpatient surgery.33 Assessing the exact cost for comparison is difficult as different values are frequently quoted. Some papers use the cost of performing surgery, and others the charge to the patient. Although the exact value is difficult to calculate, it is clear that there is a cost saving when thyroidectomy surgery is performed in the outpatient setting.
Limitations
We have attempted to accurately represent all the contemporary data pertaining to ambulatory thyroidectomy. However, a large proportion of the overall cases incorporated within the analysis are from a single paper by Orosco et al (25,634 of 30,453 [84%]).15 This may obviously introduce a bias into any results or conclusions reached from this analysis. Additionally, a lack of standardization across studies in relation to defining procedures and outcomes makes comparison of papers challenging and interpretation difficult.
Although we have attempted to extract all relevant contemporaneous data pertaining to ambulatory thyroidectomy with our search criteria, the resulting studies are a heterogeneous mix with a significant proportion being retrospective with few randomized control trials and a potential for reporting bias. Consequently, we have not felt able to undertake a formal meta-analysis of the data extracted.
We accept that it is also possible that duplication of data may have occurred from different papers if the individual institution published data and another author used national databases with the same data included. In some of the papers, because of the outpatient nature of the surgery, the only way postoperative complications were found was if the patient represented to the same hospital. It is possible that patients either did not represent or presented elsewhere. This would have the apparent effect of reducing complication incidence.
Conclusion
Authors advocating ambulatory thyroidectomy emphasize the importance of patient selection, monitoring and appropriate setup. The predominant concern remains on cervical hematoma and the risk of airway compromise. We believe that this is the main reason why ambulatory thyroidectomy is not more widespread.
Cervical hematoma appears unpredictable, and 11/14 (70%) cases discussed above presented between 2 and 9 days postoperatively. None of the papers cited described definite perioperative risk factors to predict the occurrence of cervical hematoma. We have found only one report of a postoperative death that was unrelated to surgical complications. There is a body of evidence that suggests that ambulatory thyroidectomy in the hands of experienced operating teams within an appropriate setting can be performed with acceptable risk profile. We have found little evidence to support the use of one anesthetic technique over another. There appears to be a shorter in-hospital stay for patients undergoing an LA/sedation technique over those receiving GA. There is no difference between the two in relation to perioperative complications. The rates of hospital admission and readmission related to anesthetic factors appear to be low and relate to pain and postoperative nausea and vomiting.
Currently practise at our institution is to perform thyroidectomy on an inpatient basis. This is in line with current BAETS guidance, due to the concern regarding cervical hematoma. We have, however, previously undertaken day case thyroidectomy, without incident, prior to the publication of the BAETS guideline. Although our data would seem to indicate the relative safety of ambulatory thyroidectomy within a well set up service it is unlikely we will change our practice in light of these findings. This is largely due to the medico-legal difficulties which are likely to be encountered, having contravened current BAETS guidance, should any significant complications arise.
Disclosure
The authors report no conflicts of interest in this work.
References
Terris DJ, Moister B, Seybt MW, Gourin CG, Chin E. Outpatient thyroid surgery is safe and desirable. Otolaryngol Head Neck Surg. 2007;136(4):556–559. | ||
Snyder SK, Hamid KS, Roberson CR, et al. Outpatient thyroidectomy is safe and reasonable: experience with more than 1,000 planned outpatient procedures. J Am Coll Surg. 2010;210(5):575–584. | ||
Ayala MA, Yencha MW. Outpatient thyroid surgery in a low-surgical volume hospital. World J Surg. 2015;39(9):2253–2258. | ||
Mowschenson PM, Hodin RA. Outpatient thyroid and parathyroid surgery: a prospective study of feasibility, safety, and costs. Surgery. 1995;118(6):1051–1053. | ||
Lo Gerfo P, Gates R, Gazetas P. Outpatient and short-stay thyroid surgery. Head Neck. 1991;13(2):97–101. | ||
Doran HE, England J, Palazzo F, Surgeons BAoEaT. Questionable safety of thyroid surgery with same day discharge. Ann R Coll Surg Engl. 2012;94(8):543–547. | ||
Menegaux F, AFCE. Ambulatory thyroidectomy: recommendations from the Association Francophone de Chirurgie Endocrinienne (AFCE). Investigating current practices. J Visc Surg. 2013;150(3):165–171. | ||
Terris DJ, Snyder S, Carneiro-Pla D, et al. American Thyroid Association statement on outpatient thyroidectomy. Thyroid. 2013;23(10):1193–1202. | ||
Snyder SK, Roberson CR, Cummings CC, Rajab MH. Local anesthesia with monitored anesthesia care vs general anesthesia in thyroidectomy: a randomized study. Arch Surg. 2006;141(2):167–173. | ||
Hessman C, Fields J, Schuman E. Outpatient thyroidectomy: is it a safe and reasonable option? Am J Surg. 2011;201(5):565–568. | ||
Torfs A, Laureyns G, Lemkens P. Outpatient hemithyroidectomy: safety and feasibility. B-ENT. 2012;8(4):279–283. | ||
Champault A, Vons C, Zilberman S, Labaille T, Brosseau S, Franco D. How to perform a thyroidectomy in an outpatient setting. Langenbecks Arch Surg. 2009;394(5):897–902. | ||
Lacroix C, Potard G, Clodic C, Mornet E, Valette G, Marianowski R. Outpatient hemithyroidectomy. Eur Ann Otorhinolaryngol Head Neck Dis. 2014;131(1):21–26. | ||
Trottier DC, Barron P, Moonje V, Tadros S. Outpatient thyroid surgery: should patients be discharged on the day of their procedures? Can J Surg. 2009;52(3):182–186. | ||
Orosco RK, Lin HW, Bhattacharyya N. Ambulatory thyroidectomy: a multistate study of revisits and complications. Otolaryngol Head Neck Surg. 2015;152(6):1017–1023. | ||
Sklar M, Ali MJ, Solomon P. Outpatient thyroid surgery in a Toronto community hospital. J Otolaryngol Head Neck Surg. 2011;40(6):458–461. | ||
Narayanan S, Arumugam D, Mennona S, Wang M, Davidov T, Trooskin SZ. An evaluation of postoperative complications and cost after short-stay thyroid operations. Ann Surg Oncol. 2016;23(5):1440–1445. | ||
Rutledge J, Siegel E, Belcher R, Bodenner D, Stack BC. Barriers to same-day discharge of patients undergoing total and completion thyroidectomy. Otolaryngol Head Neck Surg. 2014;150(5):770–774. | ||
Burkey SH, van Heerden JA, Thompson GB, Grant CS, Schleck CD, Farley DR. Reexploration for symptomatic hematomas after cervical exploration. Surgery. 2001;130(6):914–920. | ||
Leyre P, Desurmont T, Lacoste L, et al. Does the risk of compressive hematoma after thyroidectomy authorize 1-day surgery? Langenbecks Arch Surg. 2008;393(5):733–737. | ||
Schwartz AE, Clark OH, Ituarte P, Lo Gerfo P. Therapeutic controversy: thyroid surgery–the choice. J Clin Endocrinol Metab. 1998;83(4):1097–1105. | ||
Bononi M, Amore Bonapasta S, Vari A, et al. Incidence and circumstances of cervical hematoma complicating thyroidectomy and its relationship to postoperative vomiting. Head Neck. 2010;32(9):1173–1177. | ||
Mazeh H, Khan Q, Schneider DF, Schaefer S, Sippel RS, Chen H. Same-day thyroidectomy program: eligibility and safety evaluation. Surgery. 2012;152(6):1133–1141. | ||
Chin CW, Loh KS, Tan KS. Ambulatory thyroid surgery: an audit of safety and outcomes. Singapore Med J. 2007;48(8):720–724. | ||
Segel JM, Duke WS, White JR, Waller JL, Terris DJ. Outpatient thyroid surgery: safety of an optimized protocol in more than 1,000 patients. Surgery. 2016;159(2):518–523. | ||
Houlton JJ, Pechter W, Steward DL. PACU PTH facilitates safe outpatient total thyroidectomy. Otolaryngol Head Neck Surg. 2011;144(1):43–47. | ||
Payne RJ, Hier MP, Tamilia M, Mac Namara E, Young J, Black MJ. Same-day discharge after total thyroidectomy: the value of 6-hour serum parathyroid hormone and calcium levels. Head Neck. 2005;27(1):1–7. | ||
Stack BC, Moore E, Spencer H, Medvedev S, Bodenner DL. Outpatient thyroid surgery data from the University Health System (UHC) Consortium. Otolaryngol Head Neck Surg. 2013;148(5):740–745. | ||
Seybt MW, Terris DJ. Outpatient thyroidectomy: experience in over 200 patients. Laryngoscope. 2010;120(5):959–963. | ||
Materazzi G, Dionigi G, Berti P, et al. One-day thyroid surgery: retrospective analysis of safety and patient satisfaction on a consecutive series of 1,571 cases over a three-year period. Eur Surg Res. 2007;39(3):182–188. | ||
Sahmkow SI, Audet N, Nadeau S, Camiré M, Beaudoin D. Outpatient thyroidectomy: safety and patients’ satisfaction. J Otolaryngol Head Neck Surg. 2012;41(Suppl 1):S1–S12. | ||
Alderwick Ha. Better ValueiIn the NHS : The Role of Changes in Clinical Practice. Marylebone: The King’s Fund; 2015. | ||
Marino M, Spencer H, Hohmann S, Bodenner D, Stack BC. Costs of outpatient thyroid surgery from the University HealthSystem Consortium (UHC) database. Otolaryngol Head Neck Surg. 2014;150(5):762–769. | ||
Rajeev P, Sutaria R, Ezzat T, Mihai R, Sadler GP. Changing trends in thyroid and parathyroid surgery over the decade: is same-day discharge feasible in the United Kingdom? World J Surg. 2014;38(11):2825–2830. | ||
Teoh AY, Tang YC, Leong HT. Feasibility study of day case thyroidectomy. ANZ J Surg. 2008;78(10):864–866. | ||
Carlos A. Outpatient hemi-thyroidectomy: is it safe? Ammbul Surg. 2010;16:17–19. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

