Back to Journals » Clinical Ophthalmology » Volume 13
Amblyopia Treatment Efficacy in Anisometropia
Authors Al Ammari HM, Al Shamlan FT
Received 24 July 2019
Accepted for publication 8 November 2019
Published 5 December 2019 Volume 2019:13 Pages 2395—2402
DOI https://doi.org/10.2147/OPTH.S224463
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hessa M Al Ammari, Fatemah T Al Shamlan
Pediatric Ophthalmology and Strabismus Department, Dhahran Eye Specialist Hospital, Dhahran, Saudi Arabia
Correspondence: Fatemah T Al Shamlan
Dhahran Eye Specialist Hospital, 7630 H.E Ali Naimi Street, Aljamiah District, Dhahran 34257, Saudi Arabia
Email [email protected]
Purpose: To compare the treatment efficacy of optical correction and occlusion therapy and/or penalization for different anisometropic refractive errors (hyperopic, myopic, and mixed).
Methods: Medical records of 51 patients with anisometropic amblyopia managed by both optical correction and occlusion therapy and/or penalization were evaluated retrospectively. Patients were categorized into hyperopic, myopic or mixed anisometropia groups. Cycloplegic refraction, spherical anisometropia, baseline visual acuity, baseline interocular difference, final visual acuity and final interocular difference were analyzed to assess association between type of anisometropia with both resolution of anisometropic amblyopia and the time required to achieve it.
Results: Baseline visual acuity of the amblyopic was 0.94±0.47 in the hyperopic group; 1.12±0.56, in the myopic group; and 1.08 ±0.39 in the mixed group. Final visual acuity in the amblyopic eye was 0.34±0.30 in the hyperopic group, 0.78±0.59 in the myopic group, and 0.78±0.56 in the mixed group. The difference in final visual acuity in the amblyopic eye between the groups was significant (P=0.014). The amblyopia was improved in 50% of patients in the hyperopic group, 23.8% in the myopic group, and 14.3% in the mixed group (P=0.081). The type of anisometropia was significantly associated with the improvement of visual acuity in the amblyopic eyes (P=0.044). The mean time for amblyopia improvement was 16.50±10.52 months in the hyperopic groups, 15.60±12.44 months in the myopic group, and 21.00±21.21 months in the mixed group (P=0.947).
Conclusion: Lower amounts of hyperopic anisometropia are as amblyogenic as higher amounts of myopic or mixed anisometropia. Mean improvement in visual acuity of an amblyopic eye with both optical correction, occlusion therapy and/or penalization is higher in patients with hyperopic anisometropia in comparison with myopic or mixed anisometropia. No significant difference was found in the time required to achieve improvement between the study groups.
Keywords: amblyopia, anisometropia, hyperopia, myopia, occlusion therapy, penalization
Introduction
Amblyopia is the most common cause of preventable monocular visual loss in children,1–3 affecting approximately 1.6–3.6% of the population.4 It is defined as a decrease in best-corrected visual acuity due to refractive error, strabismus or deprivation at the critical period of visual development.5 Anisometropia is a refractive imbalance between the patient’s eyes.6 The eye that results in anisometropic amblyopia is the one that receives blurred image to retina and transmits it to the brain. It is the only amblyogenic factor detected in 37% of cases.6 Anisometropic amblyopia is still being treated by glasses or contact lenses, or with adding patching or other modalities that cause the two eyes to be stimulated differentially.
Anisometropia has been evaluated in numerous studies.7–9 However, the comparison of efficacy of amblyopia treatment with both optical correction and occlusion therapy and/or penalization between different types of anisometropia (hyperopic, myopic, astigmatic and mixed) has not, we believe, been evaluated or conducted in our region or elsewhere.
The purpose of our study is to compare the treatment efficacy of optical correction and patching and/or penalization and discover which type of anisometropic refractive error is more responsive to treatment so that we can deliver optimal care and management for our patients’ condition.
Method
A retrospective cohort study was conducted at Dhahran Eye Specialist Hospital, Dhahran, Saudi Arabia. The approval to conduct the study was obtained from the ethical board and research committee in Dhahran Eye Specialist Hospital and in compliance with the Declaration of Helsinki. All patients upon having a medical record in the hospital sign an acknowledgment and agreement that their medical records can be reviewed and used for research purposes. The medical records of patients who had anisometropic amblyopia diagnosed between January 2008 and January 2018 were included. The selection criteria of patients were;
- Anisometropia ≥1 diopters (spherical and/or cylindrical).
- Difference of ≥2 lines in best-corrected visual acuity.
- Age at first presentation between 3 and 12 years.
- Minimum follow-up of 12 months.
- No ocular or neurological disorder.
- Absence of strabismus or other forms of amblyopia.
- No previous ocular surgery.
Fifty-one patients were included in the study. All patients went through a complete ophthalmological examination including cycloplegic retinoscopy, slit-lamp examination, and fundoscopy and motility tests. Best-corrected visual acuity was measured using Allen pictures, Sheridan–Gardiner test, Snellen chart which was obtained on the next visit after prescribing glasses or contact lens based on cycloplegic refraction result. The appropriate refractive correction was prescribed together with occlusion in the form of adhesive patches placed on the sound eye as per the recommendation of the Pediatric Eye Disease Investigator Group10 or penalization using atropine ointment 1% once daily on the sound eye11 (both therapeutic components were prescribed together). Contact lenses were given wherever required to decrease the aniseikonia.
Patients were classified into three groups – myopic, hyperopic or cylindrical anisometropia. If a cylindrical component was present with either myopia or hyperopia the classification of anisometropia was based on the component with the highest degree. In cases where one eye was myopic and the other hyperopic, patients were classified as a mixed group. The amount of the amblyopia corrected was defined as (VAas-VAae/VAas-Vase) ×100 (%), where VAas is the visual acuity of the amblyopic eye at the beginning; VAae is the visual acuity of the amblyopic eye at the end; Vase is the visual acuity of the sound eye at the end.12 Amblyopia was considered resolved when the difference between the eyes was ≤1 line.
Visual acuity was in a logarithm of minimum angle of improvement (Log MAR) for statistical analysis. The analysis was performed with IBM SPSS v.22 for Windows (IBM, Armonk, New York, USA). The normality of data was measured using the Shapiro–Wilk test. Normally distributed data were tested by analysis of variance (ANOVA), non-normally distributed data were tested by Kruskal–Wallis. A P-Value < 0.05 was considered statically significant.
The required sample size was determined to be 66 patients with G* Power software (v3.1.9.2, University Kiel, Germany) using large size effect of 0.4, 3 groups, and a study power of 80%. However, with a sample size of 51 patients the power achieved was 70%.
Results
The study included 51 patients (29 male and 22 female) with a mean age at presentation of 7.04±2.63 years. All had a minimum follow-up of 12 months, and out of the 51 patients, 21 were followed for up to 36 months (41.1%) (Table 1). The mean follow-up of patients was 25.65±9.30 months. Final visual acuity was defined as final follow-up after 12 months. The hyperopic group consisted of 16 patients, followed by 21 in the myopic group, 0 in the cylindrical group and 14 in the mixed group. Since the cylindrical anisometropia group had no patients, that group was omitted. Hence, the number of groups was reduced to three (hyperopic, myopic, and mixed anisometropia). The mean age at presentation was 6.60±3.00 years in the hyperopic group, 8.10±2.61 years in the myopic group, and 5.85±1.46 years in the mixed group (P=0.042). The mean follow-up time was 24.38±8.89 months in the hyperopic group, 24.86±9.54 months in myopic group, and 28.29±9.54 months in the mixed group (18–36 months) [P=0.509].
 |
Table 1 Demographic Features of Patients in the Study |
The mean spherical anisometropia was 2.29±1.02 diopters in the hyperopic group, 7.57±3.93 diopters in the myopic group, and 10.21±3.61 diopters in the mixed group. This was statistically significant (P < 0.001). The mean cylindrical anisometropia was 0.45±0.70 diopters in the hyperopic group, 0.82±0.89 diopters in the myopic group, and 1.09±1.48 diopters in the mixed group (P=0.371).
Baseline visual acuity of the amblyopic and sound eye was 0.94±0.47, 0.13±0.17, respectively, in the hyperopic group (Table 2, Figure 1); 1.12±0.56, 0.20±0.20 in the myopic group (Table 2, Figure 2); and 1.08 ±0.39, 0.17±0.18 in the mixed group (Table 2, Figure 3). Baseline interocular difference was 0.81 ±0.42, 0.92 ±0.64, 0.90 ±0.37 in the hyperopic, myopic and mixed groups, respectively (Table 3, Figure 4). There was no significant difference in the baseline visual acuity of the amblyopic eye, sound eye and in interocular difference in the three groups (P=0.595, 0.416, 0.831, respectively) (Table 3).
 |
Table 2 Evaluation of Visual Acuity in Log MAR During Follow-Up |
 |
Table 3 Spherical Anisometropia, Visual Acuity, and Interocular Difference Among Study Group |
 |
Figure 1 Visual acuity in hyperopic anisometropia group during follow-up. |
 |
Figure 2 Visual acuity in myopic anisometropia group during follow-up. |
 |
Figure 3 Visual acuity in mixed anisometropia group during follow-up. |
 |
Figure 4 Intraocular difference in visual acuity among anisometric groups. |
Final visual acuity in the amblyopic and sound eye was 0.34±0.30, 0.03±0.07, respectively, in the hyperopic group (Table 3, Figure 1); 0.78±0.59, 0.11±0.17 in the myopic group (Table 3, Figure 2); and 0.78±0.56, 0.07±0.09 in the mixed group (Table 3, Figure 3). Final interocular difference was 0.30±0.31, 0.67±0.61, 0.71±0.57 in the hyperopic, myopic and mixed groups, respectively (P=0.065) (Table 3, Figure 4). The mean increase in visual acuity of the amblyopic eyes from the first presentation to the final evaluation was 0.61 ± 0.37 in the hyperopic group, 0.34 ± 0.37 in the myopic group, and 0.29 ± 0.55 in the mixed group (P=0.086) (Figure 5). The improvement in visual acuity of the sound eye from baseline to the final evaluation was 0.10 ± 0.17 in hyperopic group, 0.09 ± 0.20 in myopic group, and 0.10 ±0.16 in the mixed group (P=0.993).
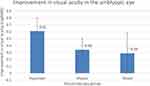 |
Figure 5 Improvement in visual acuity in amblyopic eye from baseline to final evaluation. |
The mean time for amblyopia resolution was 16.50±10.52 months in the hyperopic groups, 15.60±12.44 months in the myopic group, and 21.00±21.21 months in the mixed group (P=0.947).
Final visual acuity of 20/20 was achieved in the amblyopic eye in 25% (n=4) of patients in the hyperopic group, 4.8% (n=1) in the myopic group, and 0% in the mixed anisometropia group.
The age at presentation was not a predictive factor for final visual acuity (P=0.898).
Discussion
In our study the average age at presentation was 7.04±2.63 years. This is possible because anisometropic amblyopia is not detected until children go to school. Presentation of children with strabismus is with a mean age of 3.5 years, yet those with anisometropic amblyopia and no detected strabismus are on average 3 years older.13–15 Furthermore, anisomyopes presented at an older age (8.10±2.61 years) when compared with anisohyperopia (6.60±3.00 years). This could be because myopia increases later in life, as the eye enlarges during age progresses.
The average spherical anisometropia was found to be significantly different between the three groups (p<0.001). Despite this statistically significant difference, the initial visual acuity of the amblyopic eyes and the initial interocular difference in the three groups were not significantly different (p=0.595, 0.831, respectively). This may indicate that lower amounts of hyperopic anisometropia are as amblyogenic as higher amounts of myopic or mixed anisometropia. Results similar to ours were found in a study by Levi et al where amblyopia was doubled in hyperopic anisometropia compared to myopic anisometropia with the same degree of anisometropia.16 Tanlamai and Goss stated that regardless of the way anisometropia was measured, occurrence of amblyopia in anisohyperopia equals anisomyopes with two diopters more of anisometropia.17
This can be attributed to that defocus happens more in the eye with higher hyperopia in anisohyperopic cases. Yet in the case of anisomyopes the eye with higher degree of myopia can see near objects and the one with lesser degree of myopia will see the distant objects, thus the defocus of one eye will be less. Furthermore, amblyopia may be much worse in anisohyperopia because anisohyperopia presents in an early age.
In our study, resolution of amblyopia with both optical correction, occlusion therapy and/or penalization was found to be higher in patients with hyperopic anisometropia (50%) in comparison with patients with myopic or mixed anisometropia (23.8%, 14.3%, respectively) [P=0.081]. Although the difference in resolution of amblyopia among anisometropic groups was not statistically significant, it was clinically important.18 The mean resolution in visual acuity in amblyopic eye from baseline to final evaluation was also higher in the hyperopic anisometropia group (P=0.044) although all three groups were subjected to the same modalities of treatment (spectacle correction with either patching or penalization). These results indicate that hyperopic anisometropia is more responsive to treatment than myopic and mixed anisometropia taking into consideration that the amount of anisometropia in hyperopic group was as amblyogenic as the amount of anisometropia found in myopic and mixed group which indicates that the amblyopia was associated with the type of anisometropia rather than the amount.
Steele et al analyzed the efficacy of treating different anisometropic refractive errors with only glasses correction.19 The results of this study showed a statistically significant increase in visual acuity of the amblyopic eye in the hyperopic and astigmatic anisometropia groups with only glasses correction. In our study, 25% (n=4) of anisohyperopia achieved 20/20 vision or better, compared with 39% (n=7) in the Steele et al study. This difference can be explained by the number of patients in their study group (28 patients) that is less than what we collected and the better baseline visual acuity of amblyopic eyes (20/60) in comparison with the baseline visual acuity in our study (20/174). In addition, they only included patients who were responsive to spectacle correction and excluded those who failed this modality of treatment and required occlusion therapy, while our study included patients treated with optical correction with occlusion therapy and/or penalization.
The time required to achieve resolution in the three groups of our study was longer than that of Steele et al (6–36 months, compared with 3–22 weeks). This may be attributed to two factors. First, the better initial visual acuity at Steele et al. Second, our study was retrospective. Follow-up visits were variable according to the preference of the treating ophthalmologist. Therefore, it is difficult to know exactly when improvement and resolution happened.
In a prospective pilot study conducted by Pang et al, the outcomes of treating amblyopia associated with myopic anisometropia with both optical correction and occlusion therapy were evaluated. The mean increase in visual acuity in the amblyopic eye was 2.59 lines.20 This is consistent with mean increase in visual acuity of anisomyopes found in our study (0.34 ± 0.37).
A study conducted by Chen et al5 illustrated that there was no difference in the percentage of patients who reached resolution and the time to achieve this between different anisometropic refractive error groups. The disparity between this study and ours might be because of various definitions of anisometropia types. Chen et al classified patients with spherical and cylindrical anisometropia into a mixed group, while we classified patients into myopic, hyperopic or cylindrical groups based on the component with the highest degree of anisometropia. And if myopic and hyperopic errors were present patients were classified as a mixed group.
We found that age at presentation was not a predictive factor for final visual acuity in the amblyopic eye. This could be explained by the age of our patients, since none of them was over 12 years on presentation. Other studies21,22 indicated that for patients treated with patching, the age at presentation was not a significant factor in affecting duration to cure or final visual acuity.
Like other studies, ours has some limitations. First, this study is retrospective in nature with the follow-up visits spaced variably, unlike those of a prospective-design study. Second, the follow-up period was not the same for all patients. Third, no patients with cylindrical anisometropia were included in the study. Fourth, long-term stability of visual acuity after discontinuing of patching and/or penalization was not evaluated. And finally, we did not evaluate the changes in anisometropia along the course of follow-up treatment, which could, by itself, be a cause of improvement or decline in the status of the amblyopic eye.
Conclusion
Although there was no significant difference in time required to achieve resolution between the three groups, it was found that the type of anisometropia rather than the amount of anisometropia is a significant factor on the degree of amblyopia and the response to treatment (anisometropic hyperopia was having similar results of amblyopia compared to anisometropic myopia and mixed although the amount of anisometropia is less in the former. Furthermore, it responded better to treatment than the latter groups). Further, larger prospective studies are needed to address these findings.
Disclosure
The authors report no conflicts on interest in this work.
References
1. Ederer F, Krueger DE. Report on the National Eye Institute’s Visual Acuity Impairment Survey Pilot Study. Washington, DC: National Eye Institute; 1984:81–84.
2. Simons K. Preschool vision screening: rational, methodology and outcome. Surv Ophthamol. 1996;41:3–30. doi:10.1016/S0039-6257(97)81990-X
3. Attebo K, Mitchell P, Cumming R, et al. Prevalence and causes of amblyopia in an adult population. Ophthalmology. 1998;105:154–159. doi:10.1016/S0161-6420(98)91862-0
4. Simons K. Amblyopia characterization, treatment and prophylaxis. Surv Ophtalmol. 2005;50(2):123–166. doi:10.1016/j.survophthal.2004.12.005
5. Chen P-L, Chen JT, Tai M-C, et al. Anisometropic amblyopia treated with only glasses correction: possible factors predicting success and time to start patching. Am J Ophthalmol. 2006;09–27.
6. Pediatric Eye Disease Investigator Group. The clinical profile of moderate amblyopia in children younger than 7 years. Arch Ophthalmol. 2002;120:281–287. doi:10.1001/archopht.120.3.281
7. Caputo R, Frosini: R, De Libero C, Campa L, Magro EF, Secci J. Factors influencing severity of and recovery from anisometropic amblyopia. Strabismus. 2007;15(4):209–214. doi:10.1080/09273970701669983
8. Pediatric Eye Disease Investigator Group, Holmes JM, Kraker RT, Beck RW, et al. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110(11):2075–2087.
9. Pediatric Eye Disease Investigator Group, Holmes JM, Beck RW, Kraker RT, et al. Impact of patching and atropine treatment on the child and family in the amblyopia treatment study. Arch Ophtalmol. 2003;121(11):1625–1632.
10. Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol. 2003;121(5):603–611. doi:10.1001/archopht.121.5.603
11. Pediatric Eye Disease Investigator Group. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111(11):2076–2085. doi:10.1016/j.ophtha.2004.04.032
12. Stewart CE, Moseley MJ, Fielder AR. Defining and measuring treatment outcome in unilateral amblyopia. Br J Ophthamol. 2003;87(10):1229–1231. doi:10.1136/bjo.87.10.1229
13. Ingram MR. Refraction of 1-year old children after atropine cycloplegia. Br J Ophthamol. 1979;63(5):343–347. doi:10.1136/bjo.63.5.343
14. Shaw DE, Fielder AR, Minshull C, Rosenthal AR. Amblyopia: factors influencing age of presentation. Lancet. 1988;2(8604):207–209. (). doi:10.1016/S0140-6736(88)92301-X
15. Woodruff G, Hiscox F, Thompson JR, Smith LK. The presentation of children with amblyopia. Eye (London). 1994;8(Pt 6):623–626. doi:10.1038/eye.1994.156[PubMed]
16. Levi DM, McKee SP, Movshon JA. Visual deficit in anisometropia. Vision Res. 2011;51(1):48–57. (). doi:10.1016/j.visres.2010.09.029
17. Tanlamai T, Goss DA. Prevalence of monocular amblyopia among anisometropes. Am J Optom Physiol Opt. 1979;56(11):704–715. (). doi:10.1097/00006324-197911000-00006
18. Man-Son-Hing M, Laupacis A, O’Rourke K, et al. Determination of the clinical importance of study result: a review. J Gen Intern Med. 2002;17(6):469–476. doi:10.1046/j.1525-1497.2002.11111.x
19. Steele A, Bradfield YS, Kushner BJ, et al. Successful treatment of anisometropic amblyopia with spectacle alone. J Aapos. 2006;10:37–43. doi:10.1016/j.jaapos.2005.08.003
20. Pang Y, Allison C, Frantz KA. A prospective pilot study of outcomes for amblyopia associated with myopic anisometropia. Arch Ophthalmol. 2012;130:05. doi:10.1001/archopthalmol.2011.1203
21. Lithander J, Sjostrand J. Anisometropic and strabismic amblyopia in the age group 2 years and above: a prospective study of the results of treatment. Br J Ophthalmol. 1991;75:111–116. doi:10.1136/bjo.75.2.111
22. Wick B, Wright CM, Hrisos S, et al. Randomized controlled trial of treatment of unilateral visual impairment detected at preschool vision screening. BMJ. 2003;327:1251–1254. doi:10.1136/bmj.327.7426.1251
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
