Back to Journals » Clinical Optometry » Volume 13
Adaptation of the WHO Hand Hygiene Observation Form for Application in Optometry Training Facilities
Authors Richter SM , Barnard TG
Received 28 January 2021
Accepted for publication 17 June 2021
Published 23 July 2021 Volume 2021:13 Pages 227—234
DOI https://doi.org/10.2147/OPTO.S304315
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Susarah Maria Richter,1,2 Tobias George Barnard2
1Department of Optometry, University of Johannesburg, Johannesburg, South Africa; 2Water and Health Research Centre, University of Johannesburg, Johannesburg, South Africa
Correspondence: Susarah Maria Richter
University of Johannesburg, PO Box 17077, Doornfontein, Johannesburg, 2028, South Africa
Tel +27115596716
Email [email protected]
Background: The link between hand and surface hygiene and the spread of disease has been reported by various studies and understanding the appropriate use of hand hygiene is important in healthcare. The World Health Organization (WHO) introduced the “My Five Moments for Hand Hygiene” model to educate healthcare workers about the importance of hand hygiene to stop the spread of disease.
Objective: The objectives of this paper were to determine if the WHO Hand Hygiene Observation Form could be used to monitor for hand and personal hygiene practices of Optometry students, and what their actual hygiene practices are in an Optometry training facility in South Africa.
Methods: This cross-sectional study was performed at an Optometry training facility in South Africa using third (n=32) and fourth year (n=39) students. The Hand Hygiene Knowledge Questionnaire for Health Care Workers by the WHO was used to determine their knowledge regarding hand hygiene. After completing the questionnaire, participants were observed in the clinic while consulting patients to determine the hand and surface hygiene practices they apply.
Results: The WHO hand hygiene observation rubric was not appropriate to evaluate hand and surface hygiene in Optometry facilities. The adapted observation rubric created was a better tool to evaluate student hygiene practices and was able to record which hand or surface hygiene were missed when presented with such opportunities. Although 90.1% of the students knew that germs could be transferred to the patients via hands, only 46.5% routinely used an alcohol-based hand sanitizer.
Conclusion: This observation rubric developed during this study can assist in creating awareness with students about their own hand and surface hygiene deficiencies when interacting with patients.
Keywords: hand hygiene, Optometry in South Africa, surface hygiene, clinical observations
Background
Various studies have been published on the impact of poor personal or “public” hygiene practices on the health of patients, specifically in clinical surroundings since one is not always sure what one is exposed to. The transfer or acquisition of nosocomial infections in healthcare settings can be attributed to under staffing, overcrowding and very close patient contact due to the immense patient numbers in public health care facilities.1,2 The greater mobility of people, ever changing demographics such as the aging population,3 the increase in non-communicable diseases, the possible influx of displaced persons, an increase in new and unknown infections and insufficient access to housing and sanitation are creating an environment where there is an increased use of public health facilities. The possibility of exposure to micro-organisms in public health facilities and other common areas are a great risk4 especially patients that are immuno-compromised, the aged and children have an increased risk of contracting some form of infection due to their fragile immune systems when exposed to environmental pathogens.5,6
Mitchell et al7 indicate that healthcare workers in clinic and community settings may be at higher risk of exposure to infectious micro-organisms, and currently COVID-19 can be included in this risk6 as it has been shown to survive on surfaces such as steel for 13 hours and plastic for 16 hours.8 A lot of time is spent on cleaning hard and non-porous surfaces, but very little attention is given to other surfaces such as health care textiles (ie, uniforms, linen and curtains) and office and patient furniture. Mitchell et al7 also report that proper hand hygiene, washing hands with soap and water, using an alcohol hand rub and making use of gloves when necessary, are important routines that needs to be followed, especially when working with highly infectious diseases. If there is a disruption in the “chain” of this routine, it can have detrimental consequences for the health care worker and the patient alike. When many people share the same area, it is possible for pathogens to colonize certain surfaces and be transferred from person to person as they can survive for long periods of time in certain environments. Young et al9 report that almost 80% of infections traced back to the origin were transferred by contaminated hands.
Optometry is one of the professions most influenced by the spread of microorganisms, including the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as the optometrist not only works directly with the eyes but is near the patients’ face making direct transfer of the virus also possible.3 In the public health and clinic environment where the patient load will possibly be higher and not easily controlled, patients may sit for hours waiting to be seen by the health care worker or optometrist. There is a possibility for cross-contamination, and this should be traced to the source. Loon et al10 indicated with the first severe acute respiratory syndrome (SARS) outbreak that there is great potential for the virus (SARS) to spread to other patients through reuse of equipment including the Goldmann applanation tonometer, trial contact lenses and trial frames.
The World Health Organization (WHO) implemented the five moments of hand hygiene in 2006. The “My Five Moments for Hand Hygiene” model is described as washing or cleaning your hands (1) before touching the patient (2) before a clean/aseptic procedure (3) after a body fluid exposure risk (4) after touching a patient and (5) after touching patient surroundings.11,12 Moment 1 is mainly described as being necessary to prevent cross contamination of the patient. Moment 2 is necessary as it can be a high-risk procedure and the possibility of transference should be kept to an absolute minimum. Moment 3 is needed to protect the health care worker from transference of micro-organisms. Moment 4 would be the same as for moment 1. Moment 5 is described as when leaving the patient environment.13 This is a very elementary and important action however it has been shown that health care workers often do not comply with the requirements. Querido et al14 report on a study where only 42% of health care workers washed their hands before contact with a patient and 50% after contact with the patient. In a study15 where observers were placed in wards to monitor the 5MHH process in a hospital, it was found that health care workers were very good at complying with hygiene procedures upon entering and exiting the ward but not so much inside the ward. Health care workers touched various surface areas such as that of tubes, drips, monitors, etc. without following the required procedures. It was noted that health care workers tend to not remove their gloves inside the ward, contrary to what is required between procedures, thereby increasing the risk of cross contamination.
The objectives of this paper were to determine if the WHO Hand Hygiene Observation Form could be used to monitor for hand and personal hygiene practices of Optometry students, and what their actual hygiene practices are in an Optometry training facility in South Africa.
Materials and Methods
Study Design
This cross-sectional study was performed in May 2019 at the Optometry training facility of the University of Johannesburg (Johannesburg, South Africa). Ethical approval for the study was obtained from the Research Ethics Committee (REC-01-168-2018) of the Faculty of Health Sciences and approval from the University of Johannesburg. Optometry students in their third (n=32) and fourth year (n=39) of study working in the clinics were invited to participate in this research study. Participation was voluntary basis and they were informed that they could withdraw at any time. There were no risks involved in participating in the study and measures were taken to ensure the participants privacy and anonymity.
Data Collection
After agreeing to participate, and signing the consent forms, the students were requested to complete the Hand Hygiene Knowledge Questionnaire for Health Workers as adapted from the WHO.16 The questionnaire was to determine their knowledge and attitude of practicing hand hygiene as a daily necessity, and their perception towards hand hygiene practices. Only questions relevant to the work presented is included in this publication. After completion of the questionnaires, the students were observed at the onsite optometry training clinic in terms of how hand hygiene was practiced using the WHO17 standardized form for observation and managing hand hygiene. Answers were coded and could not be traced back to the individual student.
Due to the nature of the observations, the researcher would enter the examination room at different times during the optometric examination and did not necessarily observe the same technique completed by all students. During all observations, the opportunities were noted and if the student washed/rubbed their hands and/or cleaned the surface where contact has taken place using the WHO My 5 Moments for Hand Hygiene form. Based on the data obtained an observation rubric was developed which divided the examination room into three distinct zones namely the patient zone, student (practitioner) zone and the intermediate zone. The intermediate zone is the area shared by the optometry student and the supervisor (qualified optometrist) during the visual examination. Seventeen distinct areas were identified on the scheme (see Figure 1) of where the student most likely continuously would touch a surface and where a hand hygiene opportunity (according to the “My 5 Moments for Hand Hygiene”) could present itself. This was used for the data capturing reported in this publication.
 |
Figure 1 Observation rubric for hand hygiene opportunities at the onsite clinic. |
Students were not informed of what the observation would entail and the interaction with the patient were noted on the observation form and coded as well. Names on the questionnaire/data sheet were removed once analysis started.
Data Analysis
Data obtained from the questionnaires were entered into Microsoft Excel sheets and all statistical analyses were conducted in IBM SPSS Statistics 22. Analysis parameters were used to describe the attitudes of participants related to hand hygiene and hand hygiene practices. Tests for analysis are the Chi-squared test, independent sample t tests for significance, nonparametric methods of analysis (the Mann–Whitney U-test) and geometric mean, standard deviation, median and percentages. Differences are considered significant if the p-value is less than 0.05.
Results
The observations were initially done according to the observation form of the WHO for monitoring of hand hygiene practices.23 Data saturation was reached fairly early as it was apparent from the first number of observations at the onsite clinic that the “My 5 Moments for Hand Hygiene” observation form could not be applied in its current format in the Optometry training clinic. There were too many hygiene opportunities that presented itself (of optometry specific hygiene practice) and it was decided to adjust the observation form to suit the needs of the research study in order to take note of the hand hygiene opportunities (hand wash, hand rub or missed opportunity).
The observation rubric was developed to make it easier to keep track of the contact areas which were defined as “when during a procedure the student may touch a surface, the patient or equipment”. Every time a contact happened, it was recorded, as well as if there was an opportunity to clean the surface, wipe it or wash it. The proposed 17 distinct hygiene “areas”, as well as how it links to the three different identified zones that were initially classified after the first observations were completed (in the researcher’s opinion) were also included on the observation rubric. The patient zone is where the patient will have contact with surfaces, the student (practitioner) zone is mainly where the student will have contact with surfaces and the intermediate zone is a mixture of contact opportunities. This was translated into to the observation form (Figure 1) that was developed after the initial observations to expand on the conventional WHO observation form for the managing of hand hygiene opportunities related to optometry that was not described before.
Table 1 presents the summary of observations done at the onsite clinic after the observation form was modified. It can be seen from the information presented above, that the students had been presented with many hygiene opportunities but did not attempt to either wash or rub their hands or did not attempt to clean the equipment they came in contact with or any of the surfaces. Not even the researcher’s presence made the students think twice about the need for cleaning surfaces, their hands or equipment.
 |
Table 1 Number of Observations and Hygiene Opportunities |
All students completed the WHO questionnaires on Hand Hygiene Knowledge for Health Care workers but only questions relevant to the observations are presented. When asked about the use of an alcohol-based hand rub (Table 2), 53.5% of the students indicated that they do not use an alcohol-based hand rub routinely, which link to what was observed in the onsite clinic. It must be noted that this work was completed prior to the start of COVID-19; however, all students had received training in clinic protocol for Diagnostic Procedures in both third and fourth year of study.
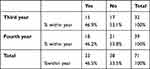 |
Table 2 Summary of Question Answer: “Do You Routinely Use an Alcohol-Based Hand Rub for Hand Hygiene?” |
Two more questions in the questionnaire asked participants if they received any training in hand hygiene practices in the last three years and if they know what the WHO “My 5 Movement of Hand Hygiene” referred too. According to the Optometry curriculum, the first-year students are introduced to the concepts of hygiene and clinical practice and the assumption would follow that the students should be aware of the concepts. Third year students are introduced to hygiene practices in the subject “Diagnostic Techniques” and the fourth-year students are once again faced with hygiene practices when they are consulting patients. Only 29.6% of the whole group indicated that they received formal training in hand hygiene in the last 3 years and only 21.1% of the group indicated that they were aware of what the “My 5 Movements for Hand Hygiene” refers to. This is an important result and will be relayed to the curriculum advisors for further action; however, it may explain the lack or complete disregard for hand hygiene and general hygiene practices that were observed in the onsite clinic.
Although the students indicated that alcohol hand rub can remove most germs from your hands, 43.7% of the students stated that 20 seconds is needed as recommended by the WHO. No statistical significant difference between the third- and fourth years were observed (p-value 0.217). The majority of the students did know that hand hygiene actions can reduce the transfer of germs to patients (90.1%) and again no significant differences were obtained between the third- and fourth-year students (p-value 0.223).
When determining the knowledge relating to hand hygiene, the question was asked in terms of which hand hygiene actions prevents transmission of germs to the patient. Table 3 also refers to the answers of the whole group in relation to the first part that was asked if prevention of transmission of germs to the patient can occur before touching the patient? Although the students are indicating the importance of hand hygiene before touching the patient to prevent any transfer of infectious organisms, it was clear from the observations that they did not do this in practice.
 |
Table 3 Summary of the Results Obtained from the Questionnaire Relating to Alcohol-Based Hand Rub and Transmission of Germs |
Discussion
The adapted observation rubric for hand hygiene opportunities proved to be more appropriate for the Optometry facilities than the WHO Hand Hygiene Observation Form. It allowed for the more comprehensive monitoring of missed hand and surface hygiene opportunities that can be used to engage with the student to explain where they missed hygiene opportunities. One of the aspects noticed during the observations completed were that equipment was used repeatedly. Students did not attempt to clean the equipment (wiping it down) or cleaning/washing their hands before commencing using the phoropter or trial frame or after touching the equipment and/or the patient. It was observed that they will leave the examination room and return and not really be concerned about hand hygiene and the impact thereof. The supervisor (facilitator) for the session will also enter the room and use/share equipment that the student used without any basic hygiene procedure practiced. The Clinic Policies and Procedures of Berkeley School of Optometry18 protocol for instrument sanitation and hygiene recommends that any instrument that will be used on a patient should be wiped down with alcohol or even rinsed and dried. It is advocated that the hands should be washed a few times during the test, especially when there was contact with the patient.
The importance of proper hand, surface and equipment hygiene was shown during the outbreak of epidemic keratoconjunctivitis (EKC) secondary to adenovirus infection traced to a single optometric clinic in the Los Angeles County Department of Public Health in 2017. Poor hand hygiene, poor cleaning of contact surfaces and equipment and the non-use of gloves when working with patient body fluids (flushing of eye) were identified as the reasons for the EKC outbreak.19 Optometry hand hygiene measures are mostly related to contact lens wear, how to clean the contact lens case and how to clean and care for the lenses. What is obvious from literature is that standard “general hygiene practice” for Optometry is lacking (especially in South Africa) in terms of how to deal with the environment where the optometrist and patient will encounter each other. This may include, but is not limited to the door to the examination room, the examination chair, handling of some of the equipment of the optometrist such as the reading card or the occluder and pd-ruler that may touch the patient’s face. Atkins20 recommended that Optometry practices implement a clear, documented strategy to prevent cross contamination in optometric practice.
Recent research by Fonn and Jones21 indicate that poor hand washing has been shown to be a risk factor for the development of microbial keratitis and corneal inflammation in contact lens wearers. A very important note is that contamination from both the hands and water plays a role in developing the associated problems. Thus, general hygiene is not only about keeping surfaces and surroundings clean, but it is also to give attention to the water source. In a review22 on contact lens care tips, it is reported that only approximately 53–77% of contact lens wearing patients wash their hands before handling or insertion of their contact lenses. It is reported that the potential for infection can be reduced by 33% if there is good hand hygiene; keeping into account how often the hands of contact lens wearers come in contact with the face, make-up, face creams, possible nicotine and even dirt. More importantly, a process is described where hand washing before lens insertion should change depending on how dirty the hands are.22 The authors advocate the WHO method of hand washing and emphasize that washing with soap and water is enough as using alcohol-based rubs may damage the surface of the contact lens. Azuamah et al23 conducted research relating to external eye diseases and personal hygiene among the patients visiting the optometry clinic in Owerri, Nigeria. Bacterial conjunctivitis caused by Staphylococcus aureus was the most prevalent eye disease as this can easily spread from person to person. Almost 80% of participants in this study indicated that they do not wash their hands after using the toilet and if they do, it will only be with water. Many indicated that they share face clothes and 60% indicated that they only clean their hand towels after two weeks or even longer. These findings could be true for any culture where there are poor social-economic circumstances, extreme poverty and poor access to clean water and sanitation.
Very little or no information related to standard hygiene practices prescribed for clinical optometric facilities in South Africa were available when the research study commenced. No direct information could be obtained from the website of the Health Professions Council of South Africa (HPCSA) nor the Professional Board of Optometry and Dispensing Opticians (PBODO). It is one of the most important things that must be in place as both the practitioner and patient may be exposed to infectious organisms. Mashige24 indicated that the PBODO should develop and publish guidelines on infection control and this would come down to proper hand hygiene practices that should be monitored for compliance. Only with the outbreak of COVID-19 did the PBODO release a directive to Optometrists in South Africa in May 2020 describing the operational requirements under the Level 4 lockdown restrictions as announced by the South African Government.25
Although hygiene is included in the curriculum, the replies from the WHO questionnaire for health care workers indicated that the students claimed that no training was given in hand hygiene practices. This correlates with the lack of hygiene practices observed during the observations and in itself is a cause of concern when taken into consideration that this could lead to the spread of germs to the patients. Interestingly, the students did report that they knew that this is one way germs could be transferred but did not make the link with the importance of hand hygiene.
Potential limitations of this study include that the work preceded the COVID-19 pandemic and that the hand and surface hygiene practices may have improved. This would still need to be tested and the observation rubric could be a useful tool for this. A second limitation is that the rubric still need to be validated against other tools and in different settings but should be adaptable for most Optometry clinic or practice settings.
Conclusion
Although no standardized hygiene practices existed for Optometry in South Africa at the stage of the study commenced, it was postulated that the students should have knowledge about basic hand hygiene practices and should be able to practice these in the clinic environment. Results from the knowledge questionnaire and the observations by the researcher in the clinic, clearly showed that there is a gap in terms of knowledge and practice of hand hygiene methods. The gap in the practicing of correct infection control measures in the long run, like with COVID-19 currently, may have a detrimental effect in the clinic environment. Based on the fact that the students did not consider proper hygiene practices, even in the presence of the facilitator, it is recommended that the adapted observation rubric be used to observe Optometry students to evaluate their hand and surface hygiene practices. It can be a useful training tool to make students aware of their lapses in hand and surface hygiene.
Disclosure
Data published in this article is obtained for the purposes of completion of a DPhil (Optometry).
The authors have no conflicts of interest in this work.
References
1. Price JR, Cole K, Bexley A, et al. Transmission of Staphylococcus aureus between health-care workers, the environment, and patients in an intensive care unit: a longitudinal cohort study based on whole-genome sequencing. Lancet Infect Dis. 2017;17(2):207–214. doi:10.1016/S1473-3099(16)30413-3
2. Willie I, Mayr A, Kreidl P, et al. Cross-sectional point prevalence survey to study the environmental contamination of nosocomial pathogens in intensive care units under real-life conditions. J Hosp Infect. 2018;98(1):90–95. doi:10.1016/j.jhin.2017.09.019
3. Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefe’s Arch Clin Exp Ophthalmol. 2020;258(5):1049–1055. doi:10.1007/s00417-020-04641-8
4. Stanwell-Smith R. The infection potential in the home and the role of hygiene: historical and current perspectives. Int J Environ Health Res. 2003;13:S9–S17. doi:10.1080/0960312031000102769
5. Sydnor ERM, Perl TM. Hospital epidemiology and infection control in acute-care settings. Clin Microbiol Rev. 2011;24(1):141–173.
6. Vouga M, Greub G. Emerging bacterial pathogens: the past and beyond. Clin Microbiol Infect. 2016;22:12–21. doi:10.1016/j.cmi.2015.10.010
7. Mitchell A, Spencer M, Edmiston C. Role of healthcare apparel and other healthcare textiles in the transmission of pathogens: a review of literature. J Hosp Infect. 2015;90:285–292. doi:10.1016/j.jhin.2015.02.017
8. Romano MR, Montericcio A, Montalbano C, et al. Facing COVID-19 in ophthalmology department. Curr Eye Res. 2020;45(6):653–658. doi:10.1080/02713683.2020.1752737
9. Young H, Plumb Z, Stevenson J, et al. Chlorhexidine to maintain cleanliness of restroom door handles. J Environ Health. 2015;78(4):14–17.
10. Loon S-C, Teah SCB, Oon LLE, Se-Thoe S-Y, Ling A-E, Leo Y-S. The severe acute respiratory syndrome coronavirus in tears. Br J Ophthalmol. 2004;88:862–863.
11. Pittet D, Allegranzi B, Boyce J. World Health Organization world alliance for patient safety first global patient safety challenge core group of experts. The World Health Organization guidelines on hand hygiene in health care and their consensus recommendations. Infect Control Hosp Epidemiol. 2009;30(7):611–622. doi:10.1086/600379
12. WHO guidelines on hand hygiene in health care: first global patient safety challenge clean care is safer care. Geneva: World Health Organization; 2009. PMID: 23805438. Available from: https://www.who.int/publications/i/item/9789241597906.
13. Price L, Roome K, Lisa R, et al. Towards improving the World Health Organization fifth moment for hand hygiene in the prevention of cross-infection. Am J Infect Control. 2016;44(6):631–635. doi:10.1016/j.ajic.2015.12.017
14. Querido MM, Aguiar L, Neves P, Pereira CC, Teixeira JP. Self-disinfecting surfaces and infection control. Colloids Surf B Biointerfaces. 2019;178:8–21. doi:10.1016/j.colsurfb.2019.02.009
15. Bergsbaken J, Schulz LT, Trapskin PJ, Marx J, Safdar N. Pharmacist participation in infection prevention: an innovative approach to monitoring compliance with the five moments for hand hygiene in a large academic medical center. Am J Infect Control. 2014;42(3):331–332. doi:10.1016/j.ajic.2013.10.009
16. World Health Organization. Hand hygiene knowledge questionnaire for health-care workers; 2009b. Available from: https://www.who.int/gpsc/5may/tools/evaluation_feedback/en/.
17. World Health Organization. Observation form. A form to complete when monitoring hand hygiene; 2009c. Available from: https://www.who.int/gpsc/5may/tools/evaluation_feedback/en/.
18. Clinic Policies and Procedures. Berkeley school of optometry. Available from: https://optometry.berkeley.edu/clinicmanual/clinic-policies-and-procedures/clinic-equipment-instrument-sanitation-hygiene/.
19. Fernandes P, Oyong K, Terashita D. There’s more than meets the eye. Opportunities for infection prevention in optometry clinics. Open Forum Infect Dis. 2018;5(Suppl1):S245. doi:10.1093/ofid/ofy210.686
20. Atkins N. The role of hand hygiene in infection control. The Optician; April, 2015. Available from: https://www.opticianonline.net/cet-archive/74.
21. Fonn D, Jones L. Hand hygiene is linked to microbial keratitis and corneal inflammatory events. Cont Lens Anterior Eye. 2019;42(2):132–135. doi:10.1016/j.clae.2018.10.022
22. Lievers CW, Cilimberg KC, Moore A. Contact lens care tips: an optometrist’s perspective. Clin Optom (Auckl). 2017;9:113–121. doi:10.2147/OPTO.S139651
23. Azuamah YC, Esenwah EC, Ahuamah OC, Ikoro NC, Iwuagwu FC, Dozie INS. External eye infections and personal hygiene practices among patients attending optometry teaching clinic Federal University of Technology, Owerri. J Nigerian Optom Assoc. 2018;20(2):53–61.
24. Mashige KP. Infection, prevention and control in optometric practice. Vision; February, 2014. Available from: https://www.researchgate.net/publication/273107508_Infection_Prevention_and_Control_in_Optometric_Practice.
25. Health Professions Council of South Africa (HPCSA). HPCSA COVID-19 guidelines Ι optometry and dispensing opticians board. eBulletin; May, 2020. Available from: https://mailchi.mp/tipafrica/ebulletin_6_may_2020-99333?e=4319fd7610.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
