Back to Journals » Clinical Optometry » Volume 7
Accommodation deficit in children with Down syndrome: practical considerations for the optometrist
Authors Little J
Received 5 May 2015
Accepted for publication 19 June 2015
Published 15 September 2015 Volume 2015:7 Pages 81—89
DOI https://doi.org/10.2147/OPTO.S63351
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Mr Simon Berry
Julie-Anne Little
School of Biomedical Sciences, University of Ulster, Coleraine, Northern Ireland, UK
Abstract: Down syndrome is the most common cause of intellectual impairment, and life expectancy in this group has increased in recent decades, meaning that health care is increasingly focused on quality of life and the management of treatable illnesses. There are frequent problems associated with vision in Down syndrome, including refractive errors, strabismus, reduced vision, and reduced accommodative ability. This review will discuss the importance of accommodative ability; describe the prevalence and nature of accommodative deficits in Down syndrome, which are found in approximately 55%–76% of individuals; discuss the management of this deficit with the prescription of bifocal correction; and summarize the possible etiologies of hypoaccommodation in Down syndrome. Finally, the review will consider practical considerations for the optometrist managing accommodative deficits in patients with Down syndrome.
Keywords: Down syndrome, accommodation, accommodative deficits, dynamic retinoscopy, bifocals, refractive error
Introduction
Down syndrome is the most common cause of intellectual disability in humans, affecting approximately one in 500–600 births in the United Kingdom.1 In addition to a higher risk of systemic diseases,2 such as hypothyroidism, osteoporosis, and cardiac problems,3 there are frequent visual deficits associated with Down syndrome. These include refractive errors,4–7 strabismus,8,9 reduced vision,10,11 nystagmus,12,13 cataract,14,15 and reduced accommodative ability.9,16–18
There has been a substantial increase in life expectancy in Down syndrome over the last number of decades, with average life expectancy reported in 2002 at 59 years in Australia,19 and 49 years in the United States.20 Quality of life and the management of treatable illnesses are increasingly the focus of medical care in Down syndrome,21 especially with increased risk of dementia and respiratory failure.22 It has been reported that vision disorders can negatively impact cognitive function in individuals with Down syndrome.23 Consequently, it is important for optometrists in primary care to have knowledge of this condition to be equipped for examination and the effective management of patients with Down syndrome in order to maximize these patients’ visual capacity.
One particular aspect of visual function that can be effectively managed by optometrists is accommodative deficits. Woodhouse et al16 initially established that significant accommodative deficits were present in children with Down syndrome, and further work has established that this is not just a consequence of other ocular conditions, such as uncorrected refractive error or poor visual acuity (VA). Accommodative deficits are particularly important as near tasks are central to development in childhood. Children with Down syndrome are considered visual learners,24 and vision is a key sense contributing to the achievement of developmental milestones and accessing educational and recreational material. This article will describe the profile of accommodative deficits in Down syndrome and the management of this with bifocal correction. As accommodation and refractive error are closely linked, the review will begin by summarizing what is known about refractive error in this population.
Refractive errors in Down syndrome
Refractive errors are common in Down syndrome, and longitudinal refractive assessment on infants and young children report a failure to emmetropize.4,5,25 Large magnitudes of refractive error are common in Down syndrome, particularly hyperopic refractive errors,26 and Woodhouse et al27 note that refractive errors present in infancy in Down syndrome are often not only retained, but they increase. Prevalence of hyperopia has been reported to be as much as 55%,7 depending on the definitions used. Astigmatism is also more prevalent, with Little et al28 reporting a 41% rate of astigmatism >0.50 DC and significantly steeper corneas. Mirrored oblique astigmatism is a frequent finding.28 Again, depending on classification and the age of the children examined, myopia prevalence is reported to range between 8% and 25%,4,7,29 and Bromham et al29 noted an association between congenital heart defects and the presence of myopia. It is important that refractive error is measured and monitored in Down syndrome and refractive correction prescribed when significant.
Accommodative function
The accommodative ability of the eye is vital for the human visual system to effectively see over a range of near distances. The retina is provided with a clear, sharp image through changes to the shape and thickness of the crystalline lens by contraction of the ciliary muscle. Accommodation develops early in infancy, with accurate accommodation displayed by the age of 6 months of life.30,31 Throughout childhood and early adulthood, accommodative response is typically unconscious and innate to our visual system, occurring in conjunction with vergence eye movements and pupil constriction. Early work from Donders32 in the 1860s and Duane33 demonstrated large accommodative amplitudes in childhood. Consequently, accommodative function is not routinely measured in children, as there is still the traditional clinical view that this is unnecessary. However, more recent research has challenged the convention that children always have ample reserves of accommodation.34 With the advent of portable electronic technology increasing the burden of near work educationally and recreationally, it could be increasingly important to assess accommodation to investigate near visual status.35,36
Uncorrected hyperopia places an obvious burden on accommodative performance, but while the status of accommodative function has been assessed in myopia as a precursor for myopia development,37,38 there has been limited work involving hyperopic status and accommodative deficits, and the exact magnitude of hyperopia leading to accommodative deficits and interplay with binocular functions is not well understood. Consequently, there is a lack of clinical guidance regarding prescribing for hyperopia, and considerable variation between the prescribing habits of individual optometrists. Interestingly, recent work has noted that even low amounts of uncorrected hyperopia can reduce visual performance,39 and Shankar et al40 reported that uncorrected hyperopes show evidence of avoiding reading tasks. However, it is important to note that this association does not imply causation – ie, we cannot determine whether the presence of uncorrected hyperopia leads to reading avoidance, or whether there are other factors contributing to this situation.
While optometrists are often familiar with the measurement of amplitude of accommodation, an individual’s “typical” accommodative response to a target placed at a near distance may be more indicative of their typical function and accommodative exertion. This can be assessed through the technique of dynamic retinoscopy. Unlike the amplitude of accommodation measures where the examiner is dependent on the observer to report blurring of the target, dynamic retinoscopy is an objective technique, which can be undertaken for targets at several near test distances, and compared with normative findings. The accommodative response is the actual amount of accommodation exerted by the crystalline lens. The accommodative demand is the dioptric distance of the target from the eye, and for reasons of aberrations, depth of focus, etc (see Charman41), the accommodative response tends to be less than the demand. Rouse et al42 reported that an accommodative lag of up to 0.75 D could be considered “normal” for a child and, more recently, McClelland and Saunders43 report that a lag of up to 1.00 D for a 25 cm target is within normal limits for a typically developing child.
The accommodative deficit in Down syndrome
The prevalence of accommodative deficits in Down syndrome is approximately 55%–76%.4,6,17,44 For children with Down syndrome, a subjective assessment of amplitude of accommodation is often not appropriate, and several groups have established the use of Nott dynamic retinoscopy as an effective, objective means at assessing accommodative status.43–45 These studies have used a slightly different criterion for categorizing accommodative deficits in Down syndrome, ranging from 0.75 to >1.00 D lag, but nevertheless, this approach is attractive, due to the objective nature of the test and the relatively straightforward task of gazing at a near target required of the observer. Details of how to carry out this technique are given in the next section of this review. Figure 1, adapted from Woodhouse et al,17 illustrates the deficit in accommodative response for a group of young children with Down syndrome (5 to 85 months) compared with age-matched typically developing children. The line of equality denotes the accommodative response matching the accommodative demand, and it is evident that individuals with Down syndrome, unlike controls, have a significantly reduced response at all test distances.
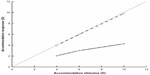  | Figure 1 Scatterplot demonstrating accommodative deficit in Down syndrome. |
The convention of Woodhouse et al17,44 and Al-Bagdady et al46 is to measure accommodation by dynamic retinoscopy at three accommodative demands, 4 D, 6 D, and 10 D. Other authors have assessed accommodation using different methods (eg, Haugen et al4), but all have consistently reported underaccommodation in Down syndrome, and also that as the accommodative demand increases, the accommodative deficit increases too.
Anderson et al18 used a photorefractive method to assess the dynamic accommodative response in Down syndrome and reported that only 13.5% of participants had a typical response. They also reported larger accommodative microfluctuations in comparison to controls.
Further research has investigated associations with other aspects of vision, but no clear pattern has emerged. Nandakumar and Leat47 did not find a link between underaccommodation and hyperopia in Down syndrome, whereas Stewart et al9 reported a relation between poorer accommodative responses and high levels of hyperopia. These authors also reported that those with accommodative deficits were more likely to be strabismic, but Haugen and Høvding8 failed to demonstrate this relationship in their study.
The clinical measurement of accommodation using dynamic retinoscopy
Nott dynamic retinoscopy uses the fact that if an individual is accommodating accurately on a target at near, when one observes the retinoscopy reflex holding the retinoscope beside the target, the reflex perceived will be “neutral”. If the individual has a lag of accommodative response, the reflex perceived will be a “with” movement. The examiner can then move the retinoscope away from the individual and target until a neutral reflex is observed and this distance can be recorded to quantitatively determine the lag of accommodation. Occasionally, an individual may demonstrate a “lead” of accommodation (with an “against” movement noted), and so in this case, the examiner would move the retinoscope closer to the eye until a neutral reflex is observed. To accurately determine accommodative performance, the individual will need to wear their full refractive correction for this procedure.
The monocular estimate method dynamic retinoscopy is a variation on the Nott method where plus (or minus) lenses are employed to neutralize the reflex rather than moving the retinoscope. This method, while useful, is arguably more complex to perform on an individual with Down syndrome, as the lenses are often a distraction to attention to the target.
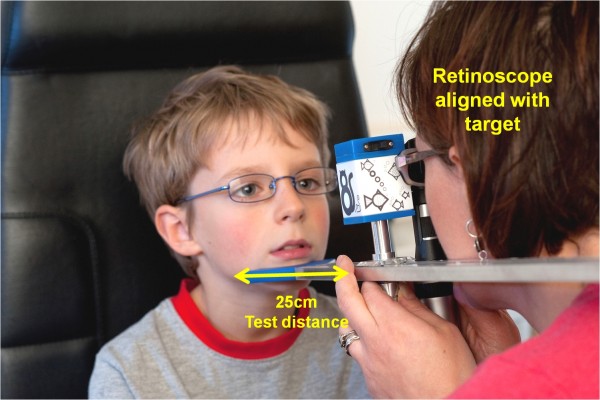
Figure 2 demonstrates the Nott dynamic retinoscopy technique with the Ulster–Cardiff accommodation cube (PA Vision Ltd, Ramsgate, UK). This instrument was recently developed to enable clinicians to easily measure accommodative function with Nott dynamic retinoscopy. The illuminated cube provides four cartoon targets of differing resolutions, to ensure that a target appropriate for a range of visual acuities can be accessed.
Accommodative norms have been reported by McClelland and Saunders43 for three target distances – 25 cm (4 diopter (D) demand), 16.67 cm (6D demand), and 10 cm (10D demand) for children aged between 4 and 15 years. McClelland & Saunders43 report the following lower 95% confidence limits for these three measurements, which gives the threshold beyond which a lag would be deemed to be significant: for the 10D demand, lag significant beyond 19.9 cm from the child; for the 6D demand, lag significant beyond 24.3 cm from the child; and for the 4D demand, lag significant beyond 34.0 cm from the child. The target distance of 25 cm (4D demand) is the most commonly used: so, for this demand, a significant lag of accommodation would be determined from dynamic retinoscopy if the examiner noted a “neutral” reflex at a distance of 34 cm or greater from the child. Adyanthaya et al,48 in a retrospective analysis of clinical visual assessments in children with Down syndrome, noted that where accommodative deficits were found, they tended to be obvious lags of accommodation.
Management of the accommodative deficit
Accommodative deficits in Down syndrome can be managed with the prescription of bifocal correction. This pragmatic approach ameliorates the accommodative deficit and ensures near vision is optimized. In some cases, single vision near glasses are prescribed, but there are several reports of the success of bifocal correction in Down syndrome and that children with Down syndrome rapidly adapt to bifocals and use the appropriate portion for tasks in daily life. A recent study reported on the increased compliance with bifocal correction in Down syndrome compared with single vision correction,48 which is in agreement with earlier work.6,47 There have been a number of longitudinal studies that have investigated bifocal prescribing, and have reported significantly improved accommodation, to accurate levels, when the accuracy of focus was measured through the bifocal segment.6,46,47,49 These studies assessed accommodative ability with dynamic retinoscopy and prescribed bifocals when a significant accommodative deficit was found. Nandakumar and Leat47 and Nandakumar et al49 also reported improvement in literacy skills once bifocal correction was given.
Nandakumar and Leat47 used a bespoke reading addition depending on the amount of accommodative lag. Our clinic, in common with Woodhouse et al17,44 and Al-Bagdady et al,46 prescribes a +2.50 DS near addition when an accommodative deficit outside the normative values is found. The position of the bifocal is important to ensure that the segment is accessed appropriately. For children with Down syndrome, the segment top is positioned at the pupil center and a flat-top bifocal design is recommended.6
Recently, Al-Bagdady et al46 reported that the prescription of bifocals seemed to act as a treatment for accommodative deficits for a number of children with Down syndrome. In a longitudinal investigation, they reported that some children appeared to recover accommodative function, demonstrating accurate accommodation through the distance portion of their bifocal. These individuals were then returned to single vision distance glasses. This is intriguing, as it suggests that the accommodative deficit can be overcome once an individual is “shown” clear near vision, and learns to use their accommodation effectively. However, in their bifocal study in Down syndrome, Nandakumar and Leat47 and Nandakumar et al49 did not report any children where accommodative function recovered. Consequently, it is as yet unresolved as to whether bifocal correction could be considered an active treatment for accommodative deficits, or a passive correction, and these studies differed in their convention for refraction under cycloplegia or noncycloplegic methods. However, it is established that the accuracy of focus is improved with the prescription of bifocals in Down syndrome, and this provide significant benefits in terms of spectacle compliance and improving educational outcomes.
What is the etiology of accommodative deficits found in Down syndrome?
It is at yet unresolved why individuals with Down syndrome exhibit a failure to accommodate to near tasks. There are a number of explanations for this, including a mechanical or presbyopic-type deficit, or a sensory deficit.
It is known that structural aspects of the eye are different in Down syndrome, with a steeper, thinner cornea,28,50 and thinner crystalline lens.50 This could mean that even with typical innervation of the ciliary muscle, the lens does not change shape and increases in power to provide an appropriate accommodative response. However, Watt et al51 used derived lens power data from Haugen et al50 to calculate the predicted reduction in response that a thinner lens could yield (based on the percentage change in lens power), and they only found a small theoretical 0.23 D deficit in accommodative response. Another possibility is that is the crystalline lens in Down syndrome is stiffer, such as occurs in presbyopia, which could mean that the lens does not produce a response despite an input of effort. However, this is not supported by Cregg et al,52 who demonstrated that the accommodative response did not saturate, as would be found in presbyopia. In addition, Anderson et al18 noted increased microfluctuations in Down syndrome, and suggested that could indicate a more flexible crystalline lens.
Alternatively, sensory explanations of the deficit could involve differences in the accommodative/convergence relationship. The fact that esotropias are much more common in Down syndrome8,9 could support an abnormal neural control mechanism between the two systems. Recent work from our group has simultaneously investigated, for the first time, accommodation and convergence using binocular photorefraction measurements.53 This has shown that accommodative deficits occur in conjunction with accurate and appropriate vergence eye movements, substantiating the theory of a difference between the neural control mechanisms for accommodation and convergence. The accurate vergence eye movements noted also refute the notion that accommodative deficits are merely an attentional issue. Further work could involve eliciting the role of blur and disparity cues in accommodative responses and examination of the crystalline lens under accommodative effort in vivo.
Practical considerations for the optometrist
While this review has focused on accommodative deficits, visual management of the individual with Down syndrome will compromise several other aspects of assessment. Along with an understanding of the refractive error profile in Down syndrome, it is worth noting that VA is often reduced, even with optimal refractive correction. Children with Down syndrome rarely achieve “6/6” or “20/20” levels of VA. Figure 3 illustrates this with data from Little et al.54 This figure demonstrates VA (plotted against age) measured with the Lea symbols VA chart in a group of children with Down syndrome aged 6–16 years. These were compared with normative data from age-matched typically developing children, indicated by the black solid and dashed lines in Figure 3. These results indicate that when using the Lea symbols VA chart, acuity that falls outside the fifth centile (the lowest dashed line) of these normative results is considered significantly poorer, and it is evident from Figure 3 that the majority of children with Down syndrome had acuity below the normative values.
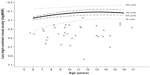  | Figure 3 Scatterplot showing the normative data for children aged 6–16 years for the Lea acuity chart, indicated by black lines, and individuals with Down syndrome, indicated by gray triangles (n=29). |
The following sections are key aspects of visual assessment for consideration of accommodative deficits in the patient with Down syndrome.
Establish visual acuity (preferably monocular) distance and near where possible
It is important to obtain a measure of VA, both binocularly and monocularly, where possible. There are a variety of alternatives to the conventional VA charts used for adults – eg, the Keeler logMAR crowded acuity test, the Lea symbols acuity chart, or the crowded Kay picture test. Getting an assessment of near VA can also be useful. A clinician may find it takes more than one visit to be confident that a reliable measure of VA is elicited. For all types of visual assessment, it can be useful to document the degree of cooperation obtained. A simple qualitative score of good/moderate/poor cooperation can be a useful reference for interpreting visual findings at future visits.
Undertake dynamic retinoscopy to assess accommodative ability
As described earlier, the technique of dynamic retinoscopy is straightforward and quick, and with practice, a clinician can efficiently determine accommodative function.
Undertake cycloplegic refraction to know the full magnitude of hyperopia
Cycloplegic refraction is recommended to elicit knowledge of the full hyperopic correction and will likely produce more reliable results for the skilled retinoscopist. For Caucasian patients, one drop of 1% cyclopentolate hydrochloride is usually sufficient to yield effective cycloplegia, and after a time lapse of 30 minutes, cycloplegic retinoscopy can be performed. Even where no deficit in accommodation is found, children with Down syndrome are likely to benefit from the correction of hyperopic refractive errors, so consideration of refractive findings is important. Once the decision to prescribe has been made, our clinic typically employs the full hyperopic refractive correction. As emmetropization does not occur, the more frequent assessment of refractive error is indicated, typically on a 6-monthly or annual basis, depending on the child’s age and necessary visual management. Astigmatism can be a frequent finding, and accompanying corneal curvature information is valuable to capture and monitor any potential pathological changes in corneal shape, as keratoconus is more frequent in Down syndrome (8%–15%).55,56
If prescribing glasses for the first time, parental and child education will be necessary to maximize compliance and success with spectacle wear. Resources for eye care professionals are available on the Ulster University Vision Resources Webpages, including a useful leaflet directed to parents encouraging spectacle wear.57
If necessary, repeat dynamic retinoscopy assessment with full refractive correction once known
If a new or significantly changed refractive correction is prescribed, once adaptation has occurred and the child is compliant with spectacle wear, it will be necessary to re-evaluate accommodation with refractive error in place. It may be that the correction of distant hyperopic refractive error alone is sufficient to promote accurate accommodation, or that the child still exhibits a significant accommodative deficit even with refractive correction in place. In the latter case, near visual correction is then indicated, either with bifocals or another type of near refractive addition.
Consider the prescription of bifocals in cases where significant lag of accommodation exists
If the child requires near refractive addition due to hypoaccommodation, then bifocals are indicated, and recommended convention is a +2.50 DS reading addition using a wide D-segment, flat-top bifocal design, fitted at the pupil center. However, there may be patients with other lifestyle and educational considerations where single vision reading glasses or another progressive-type lens may be prescribed. The simplicity of the bifocal design, rather than a progressive lens design, has the benefit of enabling observation of when the bifocal segment is being viewed through. Finally, it may be the case that the child wears his or her bifocal correction on a full-time basis or, alternatively, some children may still maintain use of another pair of single vision distance glasses for other aspects of their daily life.
Monitor the accommodative status of each child
Whether an accommodative deficit has been found and corrected, or no significant hypoaccommodation has been noted, accommodation should be routinely assessed at the child’s visual assessments. If a bifocal or other form of reading addition has been prescribed for the first time, it is valuable not only to assess accuracy of focus through the bifocal segment at the time of collection, but also as the child adapts to wearing the bifocal. It is also valuable to follow up with the parents to elicit how the child is adapting to the bifocal, and to facilitate communication of the visual status and management of spectacle wear of the child to teachers and other people involved in their daily life, especially where there may be more than one pair of spectacles.
Conclusion
With an understanding of the ocular problems and accommodative deficits frequently found in Down syndrome, and practical tips regarding visual assessment, optometrists should be able to effectively monitor and manage these patients in their clinical practice. Over time, this can be an extremely rewarding and valuable area of clinical practice, fulfilling an important aspect of care for individuals with Down syndrome.
Acknowledgment
The photographs in Figure 2 are the author’s own, and permission was granted from parent and child to use this image.
Disclosure
The author reports no conflicts of interest in this work.
References
Bell R, Rankin J, Donaldson LJ; Northern Congenital Abnormality Survey Steering Group. Down’s syndrome: occurrence and outcome in the north of England, 1985–1999. Paediatr Perinat Epidemiol. 2003; 17(1):33–39. | |
Källén B, Mastroiacovo P, Robert E. Major congenital malformations in Down syndrome. Am J Med Genet. 1996;65(2):160–166. | |
Carfì A, Antocicco M, Brandi V, et al. Characteristics of adults with down syndrome: prevalence of age-related conditions. Front Med (Lausanne). 2014;1:51. | |
Haugen OH, Høvding G, Lundström I. Refractive development in children with Down’s syndrome: a population based, longitudinal study. Br J Ophthalmol. 2001;85(6):714–719. | |
Cregg M, Woodhouse JM, Stewart RE, et al. Development of refractive error and strabismus in children with Down syndrome. Invest Ophthalmol Vis Sci. 2003;44(3):1023–1030. | |
Stewart RE, Margaret Woodhouse J, Trojanowska LD. In focus: the use of bifocal spectacles with children with Down’s syndrome. Ophthalmic Physiol Opt. 2005;25(6):514–522. | |
Ljubic A, Trajkovski V, Stankovic B. Strabismus, refractive errors and nystagmus in children and young adults with Down syndrome. Ophthalmic Genet. 2011;32(4):204–211. | |
Haugen OH, Høvding G. Strabismus and binocular function in children with Down syndrome. A population-based, longitudinal study. Acta Ophthalmol Scand. 2001;79(2):133–139. | |
Stewart RE, Woodhouse JM, Cregg M, Pakeman VH. Association between accommodative accuracy, hypermetropia, and strabismus in children with Down’s syndrome. Optom Vis Sci. 2007;84(2):149–155. | |
Tsiaras WG, Pueschel S, Keller C, Curran R, Giesswein S. Amblyopia and visual acuity in children with Down’s syndrome. Br J Ophthalmol. 1999;83(10):1112–1114. | |
Little JA, Woodhouse JM, Lauritzen JS, Saunders KJ. The impact of optical factors on resolution acuity in children with Down syndrome. Invest Ophthalmol Vis Sci. 2007;48(9):3995–4001. | |
Liza-Sharmini AT, Azlan ZN, Zilfalil BA. Ocular findings in Malaysian children with Down syndrome. Singapore Med J. 2006;47(1):14–19. | |
Stirn Kranjc B. Ocular abnormalities and systemic disease in Down syndrome. Strabismus. 2012;20(2):74–77. | |
Catalano RA. Down syndrome. Surv Ophthalmol. 1990;34(5):385–398. | |
da Cunha RP, Moreira JB. Ocular findings in Down’s syndrome. Am J Ophthalmol. 1996;122(2):236–244. | |
Woodhouse JM, Meades JS, Leat SJ, Saunders KJ. Reduced accommodation in children with Down syndrome. Invest Ophthalmol Vis Sci. 1993;34(7):2382–2387. | |
Woodhouse JM, Cregg M, Gunter HL, et al. The effect of age, size of target, and cognitive factors on accommodative responses of children with Down syndrome. Invest Ophthalmol Vis Sci. 2000;41(9):2479–2485. | |
Anderson HA, Manny RE, Glasser A, Stuebing KK. Static and dynamic measurements of accommodation in individuals with Down syndrome. Invest Ophthalmol Vis Sci. 2011;52(1):310–317. | |
Glasson EJ, Sullivan SG, Hussain R, Petterson BA, Montgomery PD, Bittles AH. The changing survival profile of people with Down’s syndrome: implications for genetic counselling. Clin Genet. 2002; 62(5):390–393. | |
Yang Q, Rasmussen SA, Friedman JM. Mortality associated with Down’s syndrome in the USA from 1983 to 1997: a population-based study. Lancet. 2002;359(9311):1019–1025. | |
Bittles AH, Bower C, Hussain R, Glasson EJ. The four ages of Down syndrome. Eur J Public Health. 2007;17(2):221–225. | |
Uppal H, Chandran S, Potluri R. Risk factors for mortality in Down syndrome. J Intellect Disabil Res. Epub April 8, 2015. | |
Lott IT, Dierssen M. Cognitive deficits and associated neurological complications in individuals with Down’s syndrome. Lancet Neurol. 2010;9(6):623–633. | |
Davis AS. Children with Down syndrome: implications for assessment and intervention in the school. Sch Psychol Q. 2008;23(2):271–281. | |
Al-Bagdady M, Murphy PJ, Woodhouse JM. Development and distribution of refractive error in children with Down’s syndrome. Br J Ophthalmol. 2011;95(8):1091–1097. | |
McCullough SJ, Little JA, Saunders KJ. Higher order aberrations in children with Down syndrome. Invest Ophthalmol Vis Sci. 2013; 54(2):1527–1535. | |
Woodhouse JM, Pakeman VH, Cregg M, et al. Refractive errors in young children with Down syndrome. Optom Vis Sci. 1997;74(10):844–851. | |
Little JA, Woodhouse JM, Saunders KJ. Corneal power and astigmatism in Down syndrome. Optom Vis Sci. 2009;86(6):748–754. | |
Bromham NR, Woodhouse JM, Cregg M, Webb E, Fraser WI. Heart defects and ocular anomalies in children with Down’s syndrome. Br J Ophthalmol. 2002;86(12):1367–1368. | |
Banks MS. The development of visual accommodation during early infancy. Child Dev. 1980;51(3):646–666. | |
Horwood AM, Riddell PM. Developmental changes in the balance of disparity, blur, and looming/proximity cues to drive ocular alignment and focus. Perception. 2013;42(7):693–715. | |
Donders FC. On the anomalies of accommodation and refraction of the eye. London: The New Sydenham Society; 1984. | |
Duane A. The accommodation and Donder’s curve and the need of revising our ideas regarding them. JAMA. 1909;52:1992–1996. | |
Sterner B, Gellerstedt M, Sjöström A. The amplitude of accommodation in 6-10-year-old children – not as good as expected! Ophthalmic Physiol Opt. 2004;24(3):246–251. | |
Hunter DG. Dynamic retinoscopy: the missing data. Surv Ophthalmol. 2001;46(3):269–274. | |
Leat SJ, Mohr A. Accommodative response in pre-presbyopes with visual impairment and its clinical implications. Invest Ophthalmol Vis Sci. 2007;48(8):3888–3896. | |
Langaas T, Riddell PM, Svarverud E, Ystenaes AE, Langeggen I, Bruenech JR. Variability of the accommodation response in early onset myopia. Optom Vis Sci. 2008;85(1):37–48. | |
Sreenivasan V, Irving EL, Bobier WR. Effect of near adds on the variability of accommodative response in myopic children. Ophthalmic Physiol Opt. 2011;31(2):145–154. | |
Narayanasamy S, Vincent SJ, Sampson GP, Wood JM. Impact of simulated hyperopia on academic-related performance in children. Optom Vis Sci. 2015;92(2):227–236. | |
Shankar S, Evans MA, Bobier WR. Hyperopia and emergent literacy of young children: pilot study. Optom Vis Sci. 2007;84(11):1031–1038. | |
Charman WN. Keeping the world in focus: how might this be achieved? Optom Vis Sci. 2011;88(3):373–376. | |
Rouse MW, Hutter RF, Shiftlett R. A normative study of the accommodative lag in elementary school children. Am J Optom Physiol Opt. 1984;61(11):693–697. | |
McClelland JF, Saunders KJ. Accommodative lag using dynamic retinoscopy: age norms for school-age children. Optom Vis Sci. 2004; 81(12):929–933. | |
Woodhouse JM, Pakeman VH, Saunders KJ, et al. Visual acuity and accommodation in infants and young children with Down’s syndrome. J Intellect Disabil Res. 1996;40( Pt 1):49–55. | |
Leat SJ, Gargon JL. Accommodative response in children and young adults using dynamic retinoscopy. Ophthalmic Physiol Opt. 1996;16(5):375–384. | |
Al-Bagdady M, Stewart RE, Watts P, Murphy PJ, Woodhouse JM. Bifocals and Down’s syndrome: correction or treatment? Ophthalmic Physiol Opt. 2009;29(4):416–421. | |
Nandakumar K, Leat SJ. Bifocals in children with Down syndrome (BiDS) – visual acuity, accommodation and early literacy skills. Acta Ophthalmol. 2010;88(6):e196–e204. | |
Adyanthaya R, Isenor S, Muthusamy B, Irsch K, Guyton DL. Children with Down syndrome benefit from bifocals as evidenced by increased compliance with spectacle wear. J AAPOS. 2014;18(5):481–484. | |
Nandakumar K, Evans MA, Briand K, Leat SJ. Bifocals in Down syndrome study (BiDS): analysis of video recorded sessions of literacy and visual perceptual skills. Clin Exp Optom. 2011;94(6):575–585. | |
Haugen OH, Høvding G, Eide GE. Biometric measurements of the eyes in teenagers and young adults with Down syndrome. Acta Ophthalmol Scand. 2001;79(6):616–625. | |
Watt T, Robertson K, Jacobs RJ. Refractive error, binocular vision and accommodation of children with Down syndrome. Clin Exp Optom. 2015;98(1):3–11. | |
Cregg M, Woodhouse JM, Pakeman VH, et al. Accommodation and refractive error in children with Down syndrome: cross-sectional and longitudinal studies. Invest Ophthalmol Vis Sci. 2001;42(1):55–63. | |
Doyle L, Little JA, Saunders KJ. Vergence and accommodation in Down syndrome: exploring the role of disparity and blur cues [abstract]. Invest Ophthalmol Vis Sci. 2014;55:3762. | |
Little JA, McCullough S, McClelland J, Jackson AJ, Saunders KJ. Low-contrast acuity measurement: does it add value in the visual assessment of Down syndrome and cerebral palsy populations? Invest Ophthalmol Vis Sci. 2013;54(1):251–257. | |
Walsh SZ. Keratoconus and blindness in 469 institutionalised subjects with Down syndrome and other causes of mental retardation. J Ment Defic Res. 1981;25 Pt 4:243–251. | |
Real de Asua D, Quero M, Moldenhauer F, Suarez C. Clinical profile and main comorbidities of Spanish adults with Down syndrome. Eur J Intern Med. Epub May 26, 2015. | |
Encouraging your child to wear spectacles [webpage on the Internet]. Ulster University [updated 2015]. Available from: http://biomed.science.ulster.ac.uk/vision/-Encouraging-your-child-to-wear,54-.html. Accessed June 15, 2015. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

