Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 10
ABCB1 and ABCC1 single-nucleotide polymorphisms in patients treated with clozapine
Authors Piatkov I, Caetano D, Assur Y, Lau SL, Jones T , Boyages SC, McLean M
Received 22 May 2017
Accepted for publication 10 July 2017
Published 28 August 2017 Volume 2017:10 Pages 235—242
DOI https://doi.org/10.2147/PGPM.S142314
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin Bluth
Irina Piatkov, Dorgival Caetano, Yolinda Assur, Sue Lynn Lau, Trudi Jones, Steven C Boyages, Mark McLean
University Clinic and Research Centre Blacktown, Western Sydney University, Western Sydney Local Health District, Blacktown, NSW, Australia
Abstract: Clozapine (CZ) has superior efficacy to other antipsychotic agents in the treatment of schizophrenia and has been extensively used in clinical practice. ATP-binding cassette (ABC) transporter proteins are responsible for the distribution of various molecules as well as drugs across extracellular and intracellular membranes, including the blood–brain barrier. Genetic variations in these proteins can account for differences in treatment response. We investigated the influence of ABCB1 rs1045642 and ABCC1 rs212090 single-nucleotide polymorphisms (SNPs) on CZ serum level, clinical outcome, and changes in body mass index (BMI) in the first year of CZ treatment. These polymorphisms influenced baseline BMI in males (p=0.009 and 0.054, B1 and C1, respectively), changes in BMI in males after 3 (p=0.026, ABCB1) and 12 months (p=0.022, ABCC1) of CZ treatment, and level of diastolic pressure (p=0.002 and 0.051, respectively). The combination of ABCB1 + ABCC1 homozygote SNPs was associated with increased CZ and norclozapine serum levels (p=0.054 and 0.010, respectively). ABC transporter SNPs could be potential biomarkers for CZ-induced weight gain and cardiovascular complications. Further pharmacogenetic research is warranted to help clinicians with their treatment decision, including concomitant use of drugs and prevention of side effects.
Keywords: ABC transporters, weight gain, blood pressure, rs1045642, rs212090
Introduction
Meta-analysis demonstrated that clozapine (CZ) has superior efficacy in the treatment of refractory schizophrenic disorders over both typical and atypical antipsychotics, and in the treatment of youth with schizophrenia over other antipsychotics.1 Short-term CZ clinical trials suggest an average improvement of 69% on the Brief Psychiatric Rating Scale, which was sustained during long-term (up to 9 years) follow-up.2 Norclozapine (NCZ) is the principal metabolite of CZ, produced by the activity of multiple liver metabolizing enzymes, and the CZ:NCZ ratio in an individual patient is indicative of their speed of metabolism of the drug. NCZ may also have therapeutic and toxic activity. CZ serum levels are significantly affected by factors other than dosage or compliance, such as smoking (which induces metabolism of CZ to NCZ), gender, and age. There is a sharp decrease in CZ metabolism in those aged ≥55 years, and CZ concentrations in males, as compared to females (after correction for both dose and weight), are 40% lower.3,4
Just two variables (gender and smoking habit) can result in a two-fold variation in CZ serum levels. We used Perry et al’s dosing nomogram5 to calculate the influence of gender and smoking on CZ serum levels. Although important, dose, gender, and smoking together accounted for only 47% of the variance in CZ serum levels.5 In a more complex nomogram, including a larger number of covariants (dose, gender, cigarette smoking habit, body weight, CZ serum concentration, and CZ:NCZ ratio), Rostami-Hodjegan et al6 found that these covariants again only explained 48% of the observed variation in CZ serum levels. It is likely that about 50% of the variance is accounted for by genetic variations. Such variations may be as subtle as a single-nucleotide polymorphism (SNP).
ATP-binding cassette (ABC) transporters, ABCB1, and ABCC1
ABC proteins are responsible for transport of various hydrophilic molecules, including drugs, across extracellular and intracellular membranes. They are characterized by the presence of an ATP-binding cassette (giving rise to the ABC name) and a transmembrane domain. ABCB1 and ABCC1 are the membrane-associated proteins encoded by corresponding gene members of this protein superfamily. ABCB1 is also known as P-glycoprotein 1 and as multidrug resistance protein 1. It has broad substrate specificity and is involved in the cellular uptake/efflux of many drugs as well as their intracellular localization and metabolism.
Genetic variance in the structure of ABCB1, or acquired mutation in tumor cells, has been shown to affect cellular responses to many drugs, for example, causing multidrug resistance in cancer.7 ABC transporter polymorphisms can also predispose individuals to adverse drug reactions.8
ABCC1 protein is located intracellularly on the basolateral side of the plasma membrane, which differs from other ABC transporters.9 This protein functions as a multispecific organic anion transporter and is found throughout most tissues in humans. It is prevalent in the lungs, spleen, testes, kidneys, placenta, thyroid, bladder, adrenal glands, and in the endothelial cells of the blood–brain barrier.9 ABCC1 plays a role in the multidrug resistance of cancerous tumor cells due to its ability to transport many chemotherapeutic drugs out of the cells. In both small- and non-small-cell lung carcinoma, higher expression of ABCC1 was indicative of a reduced response to chemotherapeutic drugs and a lower rate of survival.10
CZ and ABC transporters
Although possessing superior efficacy compared to typical antipsychotic and other atypical agents, CZ is associated with significant adverse effects including weight gain, new-onset diabetes, hypotension, and bone marrow suppression. Evidence suggests that CZ metabolism and the incidence of adverse effects may relate to the variance in ABC protein function. Life-threatening CZ-induced agranulocytosis was reported in monozygotic twins with an allelic variant of ABCB1;11 and another ABCB1 variant was found to be associated with CZ-induced neutropenia.12
ABC transporters also function in the blood–brain barrier and may influence the delivery of drugs, including CZ, into the central nervous system. Variations in ABCB1 genotype have previously been associated with altered CZ pharmacokinetics in psychotic patients13,14 as well as with the treatment response to CZ.15
Potential effect of ABCB1 and ABCC1 gene variations on drug-induced metabolic changes is emerging. This study aimed to investigate the impact of ABCB1 rs1045642 and ABCC1 rs212090 gene polymorphisms on clinical, laboratorial, and demographic variables of patients treated with CZ.
Methods
Patients
The clinical data was collected from 187 patients attending CZ clinic after their written informed consent was obtained by CZ clinic coordinator and mental health nurses; 137 of these patients gave additional written informed consent for genetic testing. The research project was approved by the Western Sydney Local Health District Human Research Ethics Committee and conducted during the years 2014 and 2015. We investigated the association between the SNPs of ABCB1 and ABCC1 with several clinical parameters, including weight and body mass index (BMI) changes in the first year of CZ treatment; systolic and diastolic blood pressure (BP; mmHg); CZ daily dose (mg), CZ and NCZ serum levels (ng/mL), and CZ:NCZ ratio; white cell count (×109/L); fasting plasma glucose and random glucose (mmol/L); HbA1c (mmol/mol); total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL) cholesterol (mmol/L), and total cholesterol:HDL ratio; triglycerides (mmol/L); prolactin (mIU/L); and estimated glomerular filtration rate (eGFR) (mL/min/1.73 m2).
Smoking status, antipsychotic use prior to CZ treatment, age, gender, selective serotonin reuptake inhibitor (SSRI) coadministration, history of diabetes, and self-identified ethnicity were recorded as potential confounding factors.
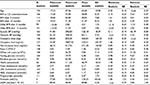
Clinical data including weight and BP readings were recorded at each clinic visit. For this analysis, we used measurements obtained at 3 and 12 months after commencement of CZ treatment. CZ and NCZ serum levels were monitored at least every 6 months. Fasting plasma glucose, HbA1c, and lipids were measured after 12 months of treatment. Because of the nature of psychotic illness and difficulties in managing a large patient cohort, there were some missing data (n is indicated for each analysis). We used average results for statistical analysis, after checking for normal distribution of data. Descriptive statistics and distribution data are presented in Table 1.
CZ treatment was initiated at low dosage and increased according to the protocol. CZ and NCZ serum levels were monitored to avoid toxicity, but were not the primary determinants of dosing decisions. Patients’ clinical status was classified as “improved” or “not-improved” according to clinical judgment made independently by the treating psychiatrist and the CZ Clinic Nurse-Coordinator, and confirmed wherever possible by the patient. Clinicians’ assessment and dosing decisions were made without any knowledge of genotype results.
Genotyping
We genotyped ABCB1 (rs1045642) and ABCC1 (rs212090) previously reported to be associated with CZ clinical efficacy.13,14 DNA was extracted using the manufacturer’s protocol for the Qiagen EZ1 BioRobot system (Qiagen, Venlo, the Netherlands). The genotyping method involved polymerase chain reaction (PCR) products analysis on an Agilent Bioanalyzer (Agilent Technologies, Santa Clara, CA, USA) in our laboratory and Sanger sequencing at the Australian Genome Research Facility. Primers used for genotyping were as follows: rs1045642 primers F-5′-GAATGTTCAGTGGCTCCGA-3′, R-5′-CTCCCAGGCTGTTTATTTGA-3′ and rs212090 primers F-5′-GACTAACGGCTAACCTGGACCT-3′, R-5′-GTTTTTCTCCCCGGAACAGTA-3′. Amplification was performed with HotStar Plus Master Mix (Qiagen, cat no 203643). The 20 µL reaction included 1 unit of HotStar polymerase, 200 µM each dNTP, 1.5 mM MgCl2, 0.5 µM primers, and ~50 ng DNA template. PCR cycling conditions were initial heating activation for 5 minutes at 95°C, 30 cycles of denaturation for 1 minute at 94°C, annealing for 1 minute at 61°C, extension for 1 minute at 72°C, and final extension for 10 minutes at 72°C.
Statistical analysis
Raw data were compiled in an Access database (Microsoft Office 2013; Microsoft Corporation, Redmond, WA, USA). Analyses were performed on the IBM SPSS 22 R-3.3.316 (IBM Corporation, Armonk, NY, USA) and GraphPad software (GraphPad Software, Inc, La Jolla, CA, USA). Variable mean differences between groups were tested by two-tailed t-test and analysis of variance (ANOVA). We compared variables influenced by the presence or absence of SNP, as well as between noncarriers and homozygote carriers. Multiple linear regression analysis was used to investigate the effects of smoking status, antipsychotic use prior to CZ treatment, age, gender, years on CZ treatment, SSRI coadministration, and ethnicity. The 95% confidence interval was used in all calculations and p-value was set at ≤0.05. Pearson correlation (two-tailed) was used to describe the strength of association between two variables. Clinical, demographic, and laboratory data were compared against the presence or absence of SNPs and its genotypes.
Results
Participant cohort
The patient cohort represented an ethnically mixed group. According to self-assessment of ethnicity, 64% were Caucasian, 13% Asian, 10% Pacific Islander, and 13% others. These were 45 (33%) women and 92 (67%) men with a mean age of 39.7 (±12.6) and 38.1 (±10.8), respectively. Forty patients (29%) were on antipsychotic medication prior to CZ commencement, 9 (6%) were co-medicated with an SSRI, and no contraceptives or estrogen containing medications were reported. Fifty-five patients (40%) were smokers. There was a significant difference in CZ dose (mg/day) between females 304 (±151) and males 392 (±180) (p<0.001).
Pearson correlation analysis revealed no association between age and BMIs in the study group (two-tailed p-values were 0.124 – BMI at CZ commencement, 0.107 – BMI after 3 months, and 0.632 – BMI after 12 months). Influence of age was demonstrated only for diastolic BP (p=0.035), fasting glucose (p=0.049), and LDL (p=0.038). For other variables (Table 1), correlation significance with age was >0.05.
The allele frequencies, calculated by Hardy–Weinberg formula, was 0.38 (T) for ABCB1 and 0.61 (A) for ABCC1, which is consistent with GenBank (National Institute of Health) data for an ethnically mixed population.
Baseline BMI level and SNPs
The BMI (kg/m2) for both homozygotic ABCB1 (T) 28.7 (±7.3) and ABCC1 (A) 26.9 (±3.7) were lower than the ones for noncarriers (31.9±10.8 and 31.2±10.0). However, these differences did not reach significance (p=0.095 and 0.060, respectively). After adjustment for age, the association between BMI and presence of SNPs for males was significant for ABCB1 and demonstrated a trend for ABCC1 (0.009 for ABCB1 and 0.054 for ABCC1; ANOVA results F=5.5, p=0.008 and F=3.5, p=0.037), but not for females (p>0.05) (Table 2).
  | Table 2 ABCB1 and ABCC1 genotypes and BMI at clozapine commencement Note: *Between presence and absence of polymorphisms. Abbreviation: BMI, body mass index. |
Multiple regression analysis was conducted to investigate the impact of other variables on the BMI of carriers and noncarriers of SNPs. Smoking status and coadministration of antidiabetic medication were identified as cofactors influencing BMI differences in ABCB1 carriers and noncarriers (p<0.001, beta =0.588, ANOVA, p=0.001, F=8.90; and p=0.008, beta =−0.521, ANOVA, p=0.026, F=4.30, respectively).
Effect of SNPs on changes in BMI after 3 and 12 months of CZ treatment
The change in BMI (∆BMI) 3 months after CZ commencement was +0.3 kg/m2 ±1.8 (N=99; min =−10.1; max =3.8) and after 12 months +0.9 kg/m2 ±3.9 (N=101; min =−12.1; max =11.0) Pearson’s correlation significance between 3 and 12 months ∆BMI was <0.001 (r=0.61).
Both ABCB1 and ABCC1 polymorphisms were associated with consistently higher, but nonsignificant, mean differences in ∆BMI (Figures 1 and 2, Table 3; p>0.05).
  | Figure 1 Changes in BMI after 3 months of clozapine commencement in carriers versus noncarriers of polymorphisms. Abbreviation: BMI, body mass index. |
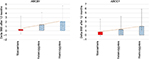  | Figure 2 Changes in BMI after 12 months of clozapine commencement in carriers versus noncarriers of polymorphisms. Abbreviation: BMI, body mass index. |
A linear regression analysis was performed holding ∆BMI as the independent variable and the following variables as dependent: age, gender, history of diabetes, family history of diabetes, country of birth, ethnicity, antipsychotic use before CZ commencement, smoking status, anticholesterol medication, anti-diabetes medication, SSRI coadministration, dosage, and CZ/NCZ serum level. We observed the association and some tendencies when we investigated the influence of gender on BMIs adjusted for age (ABCC1, F=4.6, p=0.036 BMI on commencement; ABCB1, F=3.7, p=0.056 at 12 months after commencement).
After adjustment for age and gender, statistically significant differences of ∆BMI in carriers of the polymorphisms emerged (Table 3). Noncarrier males had significantly lower ∆BMI (−0.54±2.86) than male ABCB1 carriers (0.39±1.07) when adjusted for age (p=0.026, at 3 months of CZ commencement) and lower ∆BMI (−0.038±4.1) than male ABCC1 carriers (1.98±5.5; p=0.022) adjusted for age at 12 months after CZ commencement.
We performed multiple regression analysis to investigate the influence of other variables on the BMI changes in the presence or absence of polymorphisms or genotypes. ABCB1 genotype in combination with smoking status influenced BMI changes (p=0.039, beta =−2.17; ANOVA p=0.026; F=4.20) as did ABCC1 (p=0.020, beta =0.461; ANOVA p=0.055, F=3.28).
CZ serum levels in combination with the presence or absence of ABCB1 were cofactors that also could influence BMI changes (p=0.056, beta =0.241; ANOVA p=0.054, F=3.06). CZ serum level also could correlate with ∆BMI after 3 months of CZ commencement (Pearson r=0.198, p=0.052), but not at 12 months (p=0.531). No important correlations were found between ∆BMI on the one hand and NCZ serum levels, CZ:NCZ ratio or BP, and the presence of ABC polymorphisms, on the other.
BP
Differences in diastolic BP (mmHg) at the commencement of CZ treatment were detected between carriers and noncarriers of polymorphisms (ABCB1 F=6.713, p=0.002 and ABCC1 F=3.042, p=0.051) (Table 4).
  | Table 4 Blood pressure and transporter polymorphisms Note: *Between groups Abbreviations: SNP, single-nucleotide polymorphism; SD, standard deviation; Sig, significance. |
There was also a trend to higher values of systolic BP in the presence of polymorphisms. Adjusted for age, this difference was significant for ABCB1 (beta =0.191, p=0.051), and borderline significant for ABCC1 (beta =0.175, p=0.056). After adjusting for age, the association between diastolic BP and ABCB1 genotype also remained (beta =0.187, p=0.053), but not for ABCC1 (beta =0.161, p=0.079).
Multiple regression analysis revealed that gender and the presence of ABCB1 or ABCC1 polymorphism influenced diastolic BP (beta =0.202, p=0.037 and beta =0.234, p=0.010, correspondingly), but not systolic BP (p=0.402 and 0.243, respectively) (Table 5).
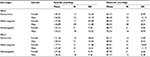  | Table 5 Gender differences in blood pressure and genotype Abbreviation: SD, standard deviation. |
When further adjusted for age, a statistically significant association was found between diastolic BP and ABCB1 or ABCC1 genotypes in males (p=0.006 and 0.031, respectively).
ABC transporter polymorphisms, CZ and NCZ serum levels, and CZ:NCZ ratio
There were no significant associations between the ABCB1 and ABCC1 SNPs genotypes and serum concentrations of CZ, NCZ, or CZ:NCZ ratio (t-test two-tailed p-values >0.05). No significant association was detected between CZ serum levels and genotypes after adjustment for age, gender, antipsychotics use prior to CZ, any co-medication, or smoking status (linear regression analysis p-values >0.05).
Influence of homozygote combination of ABCB1 and ABCC1
All variables studied were compared across the two groups: noncarriers of ABCB1 and ABCC1 (N=12) and homozygotes for both SNPs (N=3). CN and NCZ serum levels in haplotype, that includes homozygotes, were higher compared to noncarriers (CZ mean level 727.50 ng/mL ±96.73 vs 534.21 ng/mL ±230.09, t=1.23, df =8.55, p=0.054 and NCZ 460.00 ng/mL ±62.65 vs 278.04 ng/mL ±118.64, t=−3.65, df =6.23, p=0.010). No other significant associations were detected maybe because of the small sample statistical power.
Other variables
No associations were detected between the presence of polymorphisms and lipids levels, white cell count, fasting glucose, random glucose, HbA1c, prolactin, and eGFR, even when adjusted for age, smoking status, anticholesterol medication, antidiabetic medication, and gender. Ethnicity is one of the most important factors in genetic studies; however, due to the small sample cohort we have not investigated the influence of ethnicity on variations.
Discussion
Weight gain, one of the commonest CZ adverse effects,17 could be explained by the high affinity of CZ to serotonergic, dopaminergic, adrenergic, cholinergic, and histaminergic receptors.18 The mechanism of CZ-induced weight gain has not been fully elucidated. Large individual variations in weight gain suggest influence of the patient host factors.
We analyzed the impact of common SNPs of ABC transporters (ABCB1 rs1045642 and ABCC1 rs212090) on important clinical outcomes in patients treated with CZ. Carriers of T (A) allele (ABCB1) and A allele (ABCC1), in comparison with noncarriers, showed a considerable increase in BMI after 3 and 12 months of treatment and this was highly significant in males. Interestingly, the carriers of these alleles had the lowest BMIs at CZ commencement, which suggests a possible role for these ABC transporters in physiological weight control as well as in the response to drug treatment. Other identified cofactors influencing changes in BMIs in the presence of SNPs were smoking and CZ serum level.
ABCB1 polymorphisms have been previously associated with hypertension via action on renal tubular sodium transport.19,20 We found significantly higher diastolic BP in carriers of ABCB1 and ABCC1 SNPs. In males, the influence of both polymorphisms on diastolic BP was significant; however, in females significance emerged only between ABCC1 and systolic BP.
We could not find any influence of individual ABCB1 or ABCC1 SNPs on CZ, CNZ serum levels, or CZ:NCZ ratio. However, carriers with a combination of homozygote SNPs (TT + AA) did have higher levels of CZ and NCZ as compared to noncarriers (p=0.054 and 0.010, respectively).
Study limitation
This investigation was based only on data collected in everyday clinical practice. The patient cohort, who provided consent for genetic study, was comparatively small to investigate other factors that might have contributed to the results obtained. Research on the influence of other factors would require a larger group of patients.
Conclusion
ABCB1 rs1045642 and ABCC1 rs212090 SNPs can influence weight gain, BP, and CZ and NCZ serum levels in patients treated with CZ. These polymorphisms, in combination with other cofactors, could be potential biomarkers to predict CZ-induced weight gain, which in turn can lead to cardiovascular complications.
Disclosure
The authors report no conflicts of interest in this work.
References
Davis JM, Chen N, Glick ID. A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry. 2003;60(6):553–564. | ||
Schneider C, Corrigall R, Hayes D, Kyriakopoulos M, Frangou S. Systematic review of the efficacy and tolerability of clozapine in the treatment of youth with early onset schizophrenia. Eur Psychiatry. 2014;29(1):1–10. | ||
Haring C, Meise U, Humpel C, Saria A, Fleischhacker WW, Hinterhuber H. Dose-related plasma levels of clozapine: influence of smoking behaviour, sex and age. Psychopharmacology. 1989;99(Suppl):S38–S40. | ||
Centorrino F, Baldessarini RJ, Kando JC, Frankenburg FR, Volpicelli SA, Flood JG. Clozapine and metabolites: concentrations in serum and clinical findings during treatment of chronically psychotic patients. J Clin Psychopharmacol. 1994;14(2):119–125. | ||
Perry PJ, Bever KA, Arndt S, Combs MD. Relationship between patient variables and plasma clozapine concentrations: a dosing nomogram. Biol Psychiatry. 1998;44(8):733–738. | ||
Rostami-Hodjegan A, Amin AM, Spencer EP, Lennard MS, Tucker GT, Flanagan RJ. Influence of dose, cigarette smoking, age, sex, and metabolic activity on plasma clozapine concentrations: a predictive model and nomograms to aid clozapine dose adjustment and to assess compliance in individual patients. J Clin Psychopharmacol. 2004;24(1):70–78. | ||
Aldonza MB, Hong JY, Alinsug MV, Song J, Lee SK. Multiplicity of acquired cross-resistance in paclitaxel-resistant cancer cells is associated with feedback control of TUBB3 via FOXO3a-mediated ABCB1 regulation. Oncotarget. 2016;7(23):34395–34419. | ||
Zair ZM, Singer DR. Efflux transporter variants as predictors of drug toxicity in lung cancer patients: systematic review and meta-analysis. Pharmacogenomics. 2016;17(9):1089–1112. | ||
Yin J, Zhang J. Multidrug resistance-associated protein 1 (MRP1/ABCC1) polymorphism: from discovery to clinical application. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2011;36(10):927–938. | ||
Munoz M, Henderson M, Haber M, Norris M. Role of the MRP1/ABCC1 multidrug transporter protein in cancer. IUBMB Life. 2007;59(12):752–757. | ||
Anil Yagcioglu AE, Ilhan BC, Goktas MT, Babaoglu MO, Uz E, Yazici MK. Agranulocytosis related to clozapine in monozygotic twins and association with allelic variants of multidrug resistance gene MDR1. J Clin Psychopharmacol. 2011;31(2):247–249. | ||
van der Weide K, Loovers H, Pondman K, et al. Genetic risk factors for clozapine-induced neutropenia and agranulocytosis in a Dutch psychiatric population. Pharmacogenomics J. Epub 2016 May 10. | ||
Consoli G, Lastella M, Ciapparelli A, et al. ABCB1 polymorphisms are associated with clozapine plasma levels in psychotic patients. Pharmacogenomics. 2009;10(8):1267–1276. | ||
Jaquenoud Sirot E, Knezevic B, Morena GP, et al. ABCB1 and cytochrome P450 polymorphisms: clinical pharmacogenetics of clozapine. J Clin Psychopharmacol. 2009;29(4):319–326. | ||
Lee ST, Ryu S, Kim SR, et al. Association study of 27 annotated genes for clozapine pharmacogenetics: validation of preexisting studies and identification of a new candidate gene, ABCB1, for treatment response. J Clin Psychopharmacol. 2012;32(4):441–448. | ||
R Development CoreTeam. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2011. | ||
Tek C, Kucukgoncu S, Guloksuz S, Woods SW, Srihari VH, Annamalai A. Antipsychotic-induced weight gain in first-episode psychosis patients: a meta-analysis of differential effects of antipsychotic medications. Early Interv Psychiatry. 2016;10(3):193–202. | ||
Meltzer HY. An overview of the mechanism of action of clozapine. J Clin Psychiatry. 1994;55(Suppl B):47–52. | ||
Eap CB, Bochud M, Elston RC, et al. CYP3A5 and ABCB1 genes influence blood pressure and response to treatment, and their effect is modified by salt. Hypertension. 2007;49(5):1007–1014. | ||
Zhang XW, Yang JL, Liang W, et al. Genetic association study of ABCB1 gene polymorphisms with hypertension in Han Chinese population. Eur Rev Med Pharmacol Sci. 2016;20(17):3661–3671. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.