Back to Journals » ClinicoEconomics and Outcomes Research » Volume 11
A US hospital budget impact analysis of a skin closure system compared with standard of care in hip and knee arthroplasty
Authors Sadik K, Flener J, Gargiulo J , Post Z, Wurzelbacher S, Hogan A, Hollmann S, Ferko N
Received 27 July 2018
Accepted for publication 7 November 2018
Published 17 December 2018 Volume 2019:11 Pages 1—11
DOI https://doi.org/10.2147/CEOR.S181630
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samer Hamidi
Kay Sadik,1 Jana Flener,2 Jeanine Gargiulo,3 Zachary Post,4 Steven Wurzelbacher,5 Andrew Hogan,6 Sarah Hollmann,6 Nicole Ferko6
1Ethicon Inc., Health Economics Market Access, Somerville, NJ, USA; 2Proliance Orthopedic Associates, Renton, WA, USA; 3Anderson Orthopaedic Clinic, Arlington, VA, USA; 4Department of Orthopedic Surgery, Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA, USA; 5Trihealth Orthopaedic and Sports Institute, Cincinnati, OH, USA; 6Cornerstone Research Group Inc., Burlington, ON, Canada
Background: Medicare’s mandatory bundle for hip and knee arthroplasty necessitates provider accountability for quality and cost of care to 90 days, and wound closure may be a key area of consideration. The DERMABOND® PRINEO® Skin Closure System (22 cm) combines a topical skin adhesive with a self-adhering mesh without the need for dressing changes or suture or staple removal. This study estimated the budget impact of the Skin Closure System compared to other wound closure methods for hip and knee arthroplasty.
Methods: A 90-day economic model was developed assuming 500 annual hip/knee arthroplasties for a typical US hospital setting. In current practice, wound closure methods for the final skin layer were set to 50% sutures and 50% staples. In future practice, this distribution shifted to 20% sutures, 20% staples, and 60% Skin Closure System. Health care resources included materials (eg, staplers, steri-strips, and traditional/barbed sutures), standard or premium dressings, outpatient visits, and home care visits. An Expert Panel, comprised of three orthopedic physician assistants, two orthopedic surgeons, and a home health representative, was used to inform several model parameters. Other inputs were informed by national data or literature. Unit costs were based on list prices in 2016 US dollars. Uncertainty in the model was explored through one-way sensitivity and alternative scenario analyses.
Results: The analysis predicted that use of Skin Closure System in the future practice could achieve cost savings of $56.70 to $79.62 per patient, when standard or premium wound dressings are used, respectively. This translated to an annual hospital budgetary savings ranging from $28,349 to $39,809 when assuming 500 arthroplasties. Dressing materials and postoperative health care visits were key model drivers.
Conclusions: Use of the Skin Closure System may provide cost savings within hip and knee arthroplasties due to decreases in resource utilization in the postacute care setting.
Keywords: budget impact analysis, wound closure, knee arthroplasty, hip arthroplasty, hospital, economic, wound dressings, costs, postacute care
Introduction
Wound complications are one of the major sources of morbidity and costs related to arthroplasty procedures, including dehiscence, infection, inflammation, necrosis, abscess, and blistering.1–4 Surgical site complications (including infection, dehiscence, and disruption) have been reported as a key reason for readmissions, with over 30% of 30-day readmissions in total hip arthroplasty and total knee arthroplasty.5–9 Alone, surgical site infections (SSIs) are associated with serious outcomes, such as increased mortality and pose a significant economic burden.5 Another factor potentially impacting the occurrence of wound complications is wound perfusion.10 Depending on the method used for arthroplasty closure, perfusion and subsequent wound healing can either be improved (ie, using running sutures) or hindered (ie, using staples).10
In addition to current methods of wound closure such as sutures or staples, wound dressings are necessary for proper wound management.11 However, wound dressings are not intended for wound closure and therefore lack the required strength. In addition, several wound dressings require dressing changes which can be painful, time-consuming, increase pathogen exposure, and delay wound healing.11,12 In hip and knee arthroplasty, wound dressings are reported to be typically changed three to five times on average, which can impose a significant cost burden.4,13
The DERMABOND® PRINEO® Skin Closure System (22 cm) (Ethicon U.S., LLC, Somerville, NJ, USA) (ie, Skin Closure System) is a novel skin closure device that combines a topical skin adhesive (TSA) (2-octyl cyanoacrylate) with a self-adhering mesh.14 This design provides a wound closure method without the need for dressing changes. Also, the Skin Closure System has been proved to be 99% effective through 72 hours in vitro as a microbial barrier against bacteria most commonly associated with SSI, including Staphylococcus aureus, Pseudomonas aeruginosa, Escherichia coli, Enterococcus faecium, and Staphylococcus epidermidis.15 Four randomized trials have evaluated the Skin Closure System across a variety of surgery types.16–19 These randomized studies have demonstrated comparable wound closure efficacy16,17 and lower skin closure and procedure time relative to sutures.16–18 Furthermore, the Skin Closure System has also been shown to provide good cosmetic results up to 1 year,16–18 less pain at removal compared to other wound closure methods,18 and the ability for patients to shower immediately after procedure if directed by their health care practitioner.18 The TSA component has also been extensively studied in over 40 randomized trials, including within hip and knee arthroplasty.20–23
Recently, the Centers for Medicare & Medicaid Services (CMS) implemented the first mandatory bundle for hip and knee arthroplasty in 67 regions across the USA, which necessitates provider accountability for quality and cost of care to 90 days.24,25 Within the context of this health care reform environment, decision makers need to consider products that provide the best clinical outcomes, while balancing budgets. As such, the objective of this study was to conduct a 90-day budget impact analysis from the hospital provider perspective of the Skin Closure System compared with other wound closure methods (ie, sutures and staples) for hip and knee arthroplasty in the USA.
Methods
Model design
A budget impact model with a 90-day time horizon was developed using Microsoft Excel 2013 (Microsoft Corporation, Redmond, WA, USA) to estimate the total costs of wound closure methods for final skin layer closure in hip and knee arthroplasty procedures from a US hospital provider perspective, including acute and postacute care. The model assumed that 500 hip and knee arthroplasty procedures are performed annually at a facility. The model was developed in accordance with recommendations from the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Task Force Report: Budget Impact Analysis whenever possible.26
The model compared final skin layer wound closure materials, dressings, and postoperative visit costs between a current and future scenario in hip and knee arthroplasty procedures. The current scenario for wound closure methods primarily comprised staples and sutures, while the future scenario included the adoption of the Skin Closure System. In the current scenario, the model specifically assumed 50% use of staples and 50% use of sutures, as per US Premier Perspective® Database findings.27 In the future scenario, the model assumed 60% of arthroplasties would be treated with the Skin Closure System, 20% with staples, and 20% with sutures. Details of all model input values are provided in Table 1.
Expert panel
In the published literature, there is a lack of information on the steps involved in wound closure and postoperative care in hip and knee arthroplasty. To obtain a detailed understanding of these processes, expert opinion was sought. To characterize the treatment practices of wound closure care in hip and knee arthroplasty, from beginning to end, a 31-item survey was developed based on literature gaps and administered via teleconference individually with each expert. Although the survey is not a formally validated questionnaire, a face-to-face meeting was held with the expert panel after the first set of answers was obtained to help ensure face validity. The panel consisted of two orthopedic surgeons, three physician assistants that specialize in orthopedic surgeries, and one home health agency representative. The panel was used to determine typical resource use for hip and knee arthroplasty procedures over a 90-day period for wound closure with staples, sutures, or Skin Closure System. For the model, several inputs for wound closure materials, dressing materials, and postoperative visits were informed by the panel. If variability existed in clinician responses, a mean value was used where possible and variability tested in alternative scenarios.
Closure materials
Materials used for wound closure varied by closure method. Each closure method consisted of a primary product, which was used in all patients, and optional products that could be used adjunctively. The proportion of use for primary or optional materials was informed by the expert panel, analysis from the Premier Perspectives® Database, or through model assumptions.27 The number of units used for each product was gathered from the expert panel. Unit costs were determined from list prices.28 For closure with staples, the primary material was denoted to be a disposable stapler and the optional material included steri-strips. The expert panel predicted that 90% of cases would require a single stapler, whereas 10% of cases would require two, for a weighted average of 1.1 units per procedure. Added to the cost of staples was a single unit for a staple removal kit. The panel also determined all patients receiving staples were assumed to use steri-strips, with only a single package used each case.
For closure with sutures, the panel identified the primary materials to be traditional or barbed sutures and estimated breakdown of use. Traditional sutures were assumed to be used in 95% of cases and barbed sutures were used in the remaining 5%, with one suture unit used for all types. Traditional sutures comprised absorbable (ie, monocryl) and nonabsorbable (ie, nylon) sutures. All traditional suture patients were assumed to have absorbable sutures, with 5% of cases additionally requiring adjunctive nonabsorbable sutures. For optional materials, the panel identified TSAs as a potential adjunctive treatment with traditional or barbed sutures. The panel was not able to reach a consensus on the proportion of TSA use, so the US Premier Perspectives® Database was used to determine that 15.1% of suture cases require TSA.27 The panel estimated that an average of two TSA units are used per procedure.
Closure with the Skin Closure System was estimated to require one unit on average. For optional materials, the panel proposed sutures could be used adjunctively in 50% of cases. Although closure with the Skin Closure System does not require subcuticular suture use, the panel estimated that some users would still place these sutures, especially in higher tension knee procedures. It was further assumed that of suture use, 90% would involve traditional sutures (absorbable only, as nylon sutures cannot be used with Skin Closure System) and 10% would involve barbed sutures, with one unit used on average for either suture type.
Postoperative visits
The model considered postoperative costs over the 90-day period with the types of visits impacted by wound closure method being identified by the panel of experts. These included outpatient and home health nurse visits.
For outpatient visits, the panel agreed all patients would return for an average of 3 visits during the 90-day period with staples or sutures. This consisted of a visit at: 2 weeks, 6 weeks, and 3 months. The panel predicted that the use of the Skin Closure System as the primary wound closure method could reduce the number of visits by one visit. With outpatient visits, the cost per visit was assumed to be the same regardless of wound closure method and was calculated from the literature (cost per physician office visits during peri-operative period).29
With home health nursing visits, the panel was not able to estimate the proportion of arthroplasty patients receiving this service. The panel noted that hospitals would either have all patients or no patients receive home nursing care. The model default used the average as an assumption, with 50% of patients receiving home health visits during the 90-day follow-up. Similarly for outpatient visits, the panel estimated that the number of home health nursing visits during the 90-day period would be 3 on average for staples and sutures. This number could be reduced by one visit with the use of the Skin Closure System as the primary wound closure method. The cost of health nurse visits was taken from the Low Utilization Payment Adjustment rate for skilled nursing as reported by CMS.30
Dressing materials
The panel confirmed that wound dressings are commonly used following hip and knee arthroplasties. The model assumed dressings were required for all patients receiving staples or sutures for wound closure and that dressings were not required for patients treated with the Skin Closure System, as per its instruction for use.14 The panel identified that dressings could be used at different stages throughout the 90-day follow-up period, including: 1) the initial application after the arthroplasty procedure; 2) applications during inpatient stay; and 3) applications during outpatient care. The number of dressings used, and the frequency of dressing changes were assumed to depend on the type of dressing. The types of dressings were classified into two categories: standard and premium.
Standard dressings were assumed to be simple wound closure products, such as generic 4×4 gauze pads. The panel estimated that these products required a single unit during each application and that there was one dressing change during inpatient stay as well as 5 dressing changes in an outpatient setting. Premium dressings were assumed to be more advanced products that may possess antimicrobial properties. The panel further estimated that these products required a single unit during the initial application and required no dressing changes during inpatient stay or outpatient setting. Unit costs for standard and premium dressings were taken from RED BOOK Online average wholesale prices for Tegaderm™ HP Transparent Dressing and Aquacel® Ag Surgical Hydrofiber, respectively.31,32
The panel could not estimate the proportion of cases where standard vs premium dressings were utilized. Based on this, two analyses were modeled, one where only standard dressings were used and the other where only premium dressings were used (all other inputs relating to wound closure and postoperative care were identical between the two analyses).
Modeled analysis
Two base case (ie, most likely) scenarios were analyzed using model input values from Table 1. The distinction between the two scenarios was that one included only standard dressings and the other included only premium dressings. For each of the base case scenarios, several one-way sensitivity analyses were performed by increasing or decreasing the default model input values, one parameter type at a time, by 20%.
Several additional scenarios, some of which varied multiple inputs at a time, were also modeled to test potential variations in current market-share as well as uptake rates of the Skin Closure System (see Table 2). Extreme values for certain treatment practices were also tested in scenario analyses. This included the assumption of no difference in the number of outpatient visits, home health nurse visits, or both (multi-way), between comparators. Scenarios were also evaluated which assumed that either 0% or 100% of patients received home health nurse visits, as this practice is expected to dichotomously vary across settings.
  | Table 2 Market-share scenarios for base case and alternative scenario analyses |
Results
Base case scenario
Assuming 500 annual hip and knee arthroplasty procedures, the model predicted that a 60% uptake of the Skin Closure System could be cost saving to the hospital provider, regardless of the type of wound dressing (ie, standard or premium) used in the facility. Specifically, the model predicted that a facility using standard (low-cost) dressings may anticipate annual savings of $28,349 ($56.70 per patient). When a facility uses premium (higher-cost) dressings, an annual savings of $39,809 ($79.62 per patient) was predicted. In both analyses, the increased wound closure material costs were offset by reductions in the costs associated with dressing materials and postoperative visits (Figure 1; Table 3).
  | Table 3 Detailed summary of 90-day wound closure-related cost results for 500 hip and knee arthroplasty procedures in a current vs future scenario Notes: Results are provided for both standard dressing and premium dressing analysis. Negative values indicate cost savings for the future vs current scenario analysis. aAssumes 50% use of both sutures and staples.27 bAssumes 20% suture use, 20% staple use, and 60% Skin Closure System use. |
Sensitivity analysis results
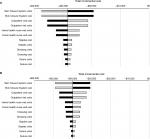
The results of the one-way sensitivity analysis, where parameters were varied by 20%, are presented in Figure 2. The model conclusions remained robust, with cost savings predicted across all scenarios tested. The results were most sensitive to changes in the number of units or unit costs of the Skin Closure System. Results were also sensitive to the number and costs of health care visits. As demonstrated by the bottom of the tornado diagram, results were least sensitive to changes in the number of units and costs of staples and sutures.
Of the 16 alternative scenarios tested, 13 were predicted to be cost saving (Figure 3). For the market-share scenarios, increasing the adoption of the Skin Closure System was predicted to increase cost savings to the hospital provider, irrespective of whether sutures or staples were the main comparator. For health care visit scenarios, the presence or absence of home nurse visits as part of a hospital protocol did not change the directionality of the results. Results were sensitive to whether differences in health care visits (ie, outpatient or home health nurse) between comparators were assumed, particularly when assuming no difference in both outpatient visits and home health nursing visits. However, in the scenarios that predicted a cost impact with increased adoption of the Skin Closure system, cost offsets were still seen, with the increased material costs associated with use of the Skin Closure System being offset by reduced dressing costs.
Discussion
The model demonstrated that the adoption of a novel wound closure device may provide important cost savings in hip and knee arthroplasty procedures to hospital providers during the critical 90-day postacute care period associated with bundled payments. These findings are a result of reduced healthcare resource utilization, particularly associated with dressing changes and postacute care visits, with increased uptake of the Skin Closure System relative to the current standard of care of sutures and staples. Specifically, the model predicts an annual cost savings of $28,349 to $39,809 per 500 hip or knee arthroplasty related to wound closure and care-related costs when there is a 60% uptake of the Skin Closure System. Our study further contributes to the literature by providing a detailed hospital budget impact assessment of a novel device in hip and knee arthroplasty as there is a dearth of economic literature in this area.
As costs and practices can vary by hospital, a range of sensitivity analyses and alternative scenarios were performed to explore uncertainty within the model. One-way sensitivity analyses highlighted that model results consistently showed cost savings with increased uptake of the Skin Closure System across upper and lower ranges of model parameters. Additional scenario analyses explored variations in model parameters that may reasonably vary across facilities in the USA, including whether sutures, staples or both are used as current practice, whether home health care visits by nurses are part of standard hospital protocol, and the level of uptake of the Skin Closure System in future practice. Many of these alternative scenarios predicted similar results to the original base case assumptions. Finally, several scenarios tested the impact of reducing the benefit of the Skin Closure System on outpatient and/or home health care nurse visits. In some of these scenarios, the incremental results for the future vs current scenario changed from cost saving to cost impact; however, this largely occurred when it was conservatively assumed that the Skin Closure System was associated with no reduction in any type of visit. In these scenarios, the increased costs associated with the Skin Closure System were still offset due to reduced dressing-related costs. The results of these analyses capture some of the potential variability in treatment patterns, resource use, and costs that may occur across hospitals and demonstrate the robustness of the economic benefits of the Skin Closure System.
According to Sharma et al, the ideal dressing for hip and knee arthroplasty wounds is that the dressing should be able to act as a microbial barrier while handling excess wound exudate, enable freedom of movement, accommodate joint flexion, enable wound visibility through the dressing, and allow for atraumatic dressing changes and removal.33 The Skin Closure System has several of these characteristics, that is, it is capable of eliminating the need for dressing changes altogether, and, unlike standard dressings, and is a method for wound closure.34,35 Evidence has shown that products that reduce the number of dressing changes may reduce costs even with increased acquisition costs.36 As wound dressings typically need to be changed three to five times in arthroplasty, reducing dressing changes saves material costs, staff time, reduces the delay in cellular activity for wound healing, and reduces the risk for pathogen exposure during the dressing changes.4,11,13 Reducing potential pathogen exposure can have significant economic benefits by reducing the risk of SSI, which is associated with total costs 3- to 4-fold higher compared to procedures without SSIs.5,37,38 The Skin Closure System provides additional benefits with its significantly greater skin-holding strength and better tension distribution across the wound compared to staples or sutures.39,40 Additionally, the Skin Closure System provides a breadth of patient benefits including the ability to shower immediately following surgery if directed by their health care professional, good cosmetic results, easy self-care since no postsurgical dressings are needed, designed to provide microbial barrier protection, no suture or staple removal, and less pain on removal.14–18,35
Additional evidence has shown the ability of the Skin Closure System to improve knee arthroplasty outcomes in a clinical setting.41 In a recent retrospective study of 1,942 total knee arthroplasty patients, statistically significant reductions were reported in 30-, 60-, 90-day all cause readmission rates, length of hospital stay, and probability of discharge to a skilled nursing facility or other nonhome setting with the Skin Closure System compared with skin staples.41 With a 30-day, all-cause readmission costing $12,839 and penalties of up to 3% of total inpatient Medicare revenue for worse-than-average readmission rates for knee arthroplasty, these results have important implications for total cost savings to US hospitals.42–44 The findings from this study further support the results of our modeling work, indicating postacute care sources of cost-savings with the Skin Closure System.
Given the current health care reform and bundled payment initiatives established by CMS for hospital reimbursement of hip and knee arthroplasty, the Skin Closure System offers a unique opportunity to both reduce health care costs and improve patient outcomes and satisfaction.24,25 With bundled payment, hospitals are reimbursed at a flat rate per episode of care as opposed to reimbursement based on the specific treatments provided. This new system creates an incentive for organizations to become more coordinated in providing the best care possible to patients rather than focusing on the quantity of services provided.45 In the context of all health care reform programs collectively, the adoption of health care technologies that are clinically superior, cost-effective, and patient-focused is critical for hospitals to succeed in meeting the principles of the Triple Aim: improve patient experience/outcomes, improve health, and reduce costs.46
Despite efforts to accurately reflect clinical practices for knee and hip arthroplasties, the model inputs are largely based on clinical opinion from a panel of experts and therefore caution must be taken in generalizing results across US provider situations. However, this methodology was necessary given the lack of published information on the process of wound closure care for these procedures. This need for caution is mitigated through the variability in experience among panel members, as panel members included a mix of those who currently do and do not use the Skin Closure System. The numerous sensitivity and scenario analyses help address this issue by accommodating the potential variety of provider processes of care. The use of expert opinion and surveys is also consistent with the ISPOR guidelines for determining inputs relating to practice patterns.26 Additionally, the methods for obtaining information from the expert panel included a very detailed and progressive set of steps to optimize the completeness and accuracy of the data, including discussion of survey questions during a teleconference as well as an in-person meeting. Future research with an expanded set of clinical experts across regions may help validate our findings.
A further limitation of the study was that the sensitivity analyses used arbitrary thresholds of ±20% to assess impact of lower and upper ranges on parameter values. However, due to the limited literature available, considering the basis of variation in the analysis on known alternative values was not always possible. At a minimum, the use of this method is beneficial for identifying the most impactful parameters which can inform decision-making. As well, additional scenario analyses help to capture the range of variability in a different way by testing the impact of model structural uncertainty and potentially different hospital facility scenarios, such as with the unknown uptake rates of the Skin Closure System. Both one-way sensitivity analyses and scenario analyses on structural uncertainty are recommended when conducting budget impact analyses.26 Another potential source of structural uncertainty was regarding whether all possible parameters were in fact included in the model. Due to limited data, certain parameters, such as risk of infection, could not be modeled. This analysis may therefore be considered conservative in terms of the potential economic benefits the Skin Closure System has relative to standard care. Further data on such outcomes can help to complete the economic assessment of this product in hip and knee arthroplasty.
The current study provides a novel perspective on the cost analysis of hip and knee arthroplasty procedures not currently found in the literature. Despite a wealth of research on skin adhesives, staples and various types of sutures, very little is available regarding devices such as the Skin Closure System, and even less is available concerning their economic benefits. With the inclusion of all currently available cost data in the model and the rigorous sensitivity and scenario analyses conducted, this study demonstrated that the Skin Closure System may have important economic benefits in the postacute care setting.
Acknowledgments
The abstract of this paper was presented at the International Society for Pharmacoeconomics and Outcomes Research 22nd Annual International Meeting as a poster presentation with interim findings. The poster’s abstract was published in “22nd International Abstracts Book” in Value in Health: https://doi.org/10.1016/j.jval.2017.05.005.
Disclosure
KS was an employee of Ethicon Inc., manufacturer of the DERMABOND® PRINEO® Skin Closure System, at the time of manuscript development. JF, JG, ZP, and SW received funding from Ethicon Inc. for their role in the expert panel and preparation of the manuscript. Cornerstone Research Group (NF, AH, and SH) received funding from Ethicon Inc. to conduct the study and prepare the manuscript.
References
Smith TO, Sexton D, Mann C, Donell S. Sutures versus staples for skin closure in orthopaedic surgery: meta-analysis. BMJ. 2010;340:c1199. | ||
Zhang W, Xue D, Yin H, et al. Barbed versus traditional sutures for wound closure in knee arthroplasty: a systematic review and meta-analysis. Sci Rep. 2016;6:19764. | ||
Krishnan R, MacNeil SD, Malvankar-Mehta MS. Comparing sutures versus staples for skin closure after orthopaedic surgery: systematic review and meta-analysis. BMJ Open. 2016;6(1):e009257. | ||
Ravenscroft MJ, Harker J, Buch KA. A prospective, randomised, controlled trial comparing wound dressings used in hip and knee surgery: aquacel and tegaderm versus cutiplast. Ann R Coll Surg Engl. 2006;88(1):18–22. | ||
Patel H, Khoury H, Girgenti D, Welner S, Yu H. Burden of surgical site infections associated with arthroplasty and the contribution of Staphylococcus aureus. Surg Infect. 2016;17(1):78–88. | ||
Varacallo MA, Herzog L, Toossi N, Johanson NA. Ten-year trends and independent risk factors for unplanned readmission following elective total joint arthroplasty at a large urban academic hospital. J Arthroplasty. 2017;32(6):1739–1746. | ||
Bernatz JT, Tueting JL, Anderson PA. Thirty-day readmission rates in orthopedics: a systematic review and meta-analysis. PLoS One. 2015;10(4):e0123593. | ||
Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT. Which clinical and patient factors influence the national economic burden of hospital readmissions after total joint arthroplasty? Clin Orthop Relat Res. 2017;475(12):2926–2937. | ||
Minhas SV, Kester BS, Lovecchio FC, Bosco JA. Nationwide 30-day readmissions after elective orthopedic surgery: reasons and implications. J Healthc Qual. 2017;39(1):34–42. | ||
Wyles CC, Jacobson SR, Houdek MT, et al. The Chitranjan Ranawat award: running subcuticular closure enables the most robust perfusion after TKA: a randomized clinical trial. Clin Orthop Relat Res. 2016;474(1):47–56. | ||
Chowdhry M, Chen AF. Wound dressings for primary and revision total joint arthroplasty. Ann Transl Med. 2015;3(18):268. | ||
Langlois J, Zaoui A, Ozil C, Courpied JP, Anract P, Hamadouche M. Randomized controlled trial of conventional versus modern surgical dressings following primary total hip and knee replacement. Int Orthop. 2015;39(7):1315–1319. | ||
Singh B, Mowbray MAS, Nunn G, Mearns S. Closure of hip wound, clips or subcuticular sutures: does it make a difference? Eur J Orthop Surg Traumatol. 2006;16(2):124–129. | ||
Ethicon US LLC. [webpage on the Internet]. DERMABOND™ PRINEO™ Skin Closure System (22 cm) instructions for use [updated April 2016]. Available from: http://hostedvl106.quosavl.com/cgi-isapi/server.dll?8080?IFUs?.cmt1bWFyMTJAaXRzLmpuai5jb20=?GetOneDocPureFullTxt?p2frdflcj7n4t01muj4u25m7nc?8. Accessed September 26, 2017. | ||
Ethicon US LLC. Su 06TR071 Study report for in vitro evaluation of microbial barrier properties of DERMABOND ProTape. Data on file. | ||
Blondeel PN, Richter D, Stoff A, Exner K, Jernbeck J, Ramakrishnan V. Evaluation of a new skin closure device in surgical incisions associated with breast procedures. Ann Plast Surg. 2014;73(6):631–637. | ||
Richter D, Stoff A, Ramakrishnan V, Exner K, Jernbeck J, Blondeel PN. A comparison of a new skin closure device and intradermal sutures in the closure of full-thickness surgical incisions. Plast Reconstr Surg. 2012;130(4):843–850. | ||
Parvizi D, Friedl H, Schintler MV, et al. Use of 2-octyl cyanoacrylate together with a self-adhering mesh (Dermabond™ Prineo™) for skin closure following abdominoplasty: an open, prospective, controlled, randomized, clinical study. Aesthetic Plast Surg. 2013;37(3):529–537. | ||
Singer AJ, Chale S, Giardano P, et al. Evaluation of a novel wound closure device: a multicenter randomized controlled trial. Acad Emerg Med. 2011;18(10):1060–1064. | ||
Khan RJ, Fick D, Yao F, et al. A comparison of three methods of wound closure following arthroplasty: a prospective, randomised, controlled trial. J Bone Joint Surg Br. 2006;88(2):238–242. | ||
Eggers MD, Fang L, Lionberger DR. A comparison of wound closure techniques for total knee arthroplasty. J Arthroplasty. 2011;26(8):1251–1258. | ||
El-Gazzar Y, Smith DC, Kim SJ, et al. The use of Dermabond® as an adjunct to wound closure after total knee arthroplasty: examining immediate postoperative wound drainage. J Arthroplasty. 2013;28(4):553–556. | ||
Siddiqui M, Bidaye A, Baird E, et al. Wound dressing following primary total hip arthroplasty: a prospective randomised controlled trial. J Wound Care. 2016;25(1):40–45. | ||
Forbes [homepage on the Internet]. Medicare’s bundled fees hit knee, hip replacements. Available from: https://www.forbes.com/sites/brucejapsen/2016/04/01/starting-today-medicares-bundled-fees-hit-hospitals-hard/#6c8d5c3226d9. Accessed November 29, 2018. | ||
CMS [homepage on the Internet]. Comprehensive care for joint replacement model. Updated May 19, 2017. Available from: https://innovation.cms.gov/initiatives/cjr. Accessed June 9, 2017. | ||
Sullivan SD, Mauskopf JA, Augustovski F, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health. 2014;17(1):5–14. | ||
Ethicon US LLC. Premier Perspectives Database. 2016. | ||
Ethicon US LLC. [homepage on the Internet]. Wound closure product ordering page; 2017; Available from: https://www.ethicon.com/na/epc/search/platform/wound%20closure?lang=en-default. Accessed November 29, 2018. | ||
Bozic KJ, Stacey B, Berger A, Sadosky A, Oster G. Resource utilization and costs before and after total joint arthroplasty. BMC Health Serv Res. 2012;12:73. | ||
Centers for Medicare & Medicaid Services [webpage on the Internet]. Home Health Prospective Payment System (HH PPS) rate update for calendar year (CY) 2016: national per-visit amounts for LUPAs. Available from: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM9406.pdf. Accessed September 29, 2017. | ||
Truven Health Analystics Micromedex Solutions [webpage on the Internet]. Red Book Online: Tegaderm HP Transparent. Available from: http://www.micromedexsolutions.com/micromedex2/librarian. Accessed November 29, 2018. | ||
Truven Health Analystics Micromedex Solutions [webpage on the Internet]. Red Book Online: Aquacel Ag Surgical Hydrofiber. Available from: http://www.micromedexsolutions.com/micromedex2/librarian. Accessed September 5, 2017. | ||
Sharma G, Lee SW, Atanacio O, Parvizi J, Kim TK. In search of the optimal wound dressing material following total hip and knee arthroplasty: a systematic review and meta-analysis. Int Orthop. 2017;41(7):1295–1305. | ||
van Nooten F, De Cock E, Fagre J, Tan R. Comparing time and supplies usage associated with a new skin closure device vs. standard of care wound closure for abdominoplasty surgery in the Netherlands. International Society for Pharmacoeconomics and Outcomes Research, 11th Annual European Congress; November 8-11th, 2008; Athens, Greece. | ||
De Cock E, van Nooten F, Mueller K, Tan R. Changing the surgical wound closure management pathway: time and supplies with PRINEO™ vs. standard of care for abdominoplasty surgery in Germany. International Society for Pharmacoeconomics and Outcomes Research, 11th Annual European Congress; November 8-11th, 2008; Athens, Greece. | ||
Bale S, Squires D, Varnon T et al. A comparison of two dressings in pressure sore management. J Wound Care. 1997;6(10):463–466. | ||
Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002;23(4):183–189. | ||
Ando M, Tamaki T, Yoshida M, et al. Surgical site infection in spinal surgery: a comparative study between 2-octyl-cyanoacrylate and staples for wound closure. Eur Spine J. 2014;23(4):854–862. | ||
Ethicon US LLC. Study to compare the tissue holding strength of DERMABOND® PRINEO® 22 cm Skin Closure System (DP22) to conventional wound closure techniques. AST-2014-0246. | ||
Ethicon US LLC. Report for mapping strains in DERMABOND® PRINEO® Skin Closure System 22 cm (DP22) Comparative Study. 100246744. Data on file. | ||
41.Johnston S, Sutton N. Comparison of Economic and Clinical Outcomes between the Dermabond® Prineo® Skin Closure System and Skin Staples in Patients Undergoing Knee Replacement in Real World Clinical Practice. Poster Presented at: ISPOR 22nd Annual International Meeting; May 20-24, 2017; Boston, MA. | ||
Healthcare Cost and Utilization Project (HCUP) [webpage on the Internet]. HCUP statistical briefs by topic [updated September, 2016]. Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sbtopic.jsp. Accessed May 24, 2017. | ||
United States Department of Labor Bureau of Labor Statistics [homepage on the Internet]. Available from: https://www.bls.gov/data/. Accessed November 29, 2018. | ||
CMS [homepage on the Internet]. Readmissions Reduction Program (HRPP) [updated April 18, 2016]. Available from: https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed November 29, 2018. | ||
Centers for Medicare & Medicaid Services [webpage on the Internet]. Bundled Payments for Care Improvement (BPCI) Initiative: general information. Available from: https://innovation.cms.gov/initiatives/bundled-payments/. Accessed November 29, 2018. | ||
Institute for Healthcare Improvement [homepage on the Internet]. The IHI Triple Aim [updated]. Available from: http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx. Accessed November 29, 2018. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.