Back to Journals » Journal of Pain Research » Volume 9
A urinary test procedure for identification of cannabidiol in patients undergoing medical therapy with marijuana
Authors Wertlake P, Henson M
Received 22 September 2015
Accepted for publication 30 November 2015
Published 12 February 2016 Volume 2016:9 Pages 81—85
DOI https://doi.org/10.2147/JPR.S96856
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Michael Schatman
Video abstract presented by Paul T Wertlake.
Views: 506
Paul T Wertlake, Michael D Henson
Pacific Toxicology Laboratories, Chatsworth, CA, USA
Abstract: Marijuana is classified by the Drug Enforcement Agency (DEA) as Schedule I, drugs having no accepted medical value. Twenty-three states and the District of Columbia have legalized medical marijuana. This conflict inhibits physicians from prescribing marijuana and the systematic study of marijuana in medical care. This study concerns the use of the clinical laboratory as a resource for physicians recommending cannabidiol (CBD) to patients, or for patients using medical marijuana. Marijuana containing delta-9-tetrahydrocannabinol (THC) is psychoactive. CBD is not psychoactive. CBD is reported to have medical benefit for seizure control, neurologic disorders including multiple sclerosis, neuropathic pain and pain associated with cancer. Use of opiates leads to increasing dosage over time that may cause respiratory depression. The Medical Board of California has termed this a serious public health crisis of addiction, overdose, and death. Is it feasible that CBD might alleviate persistent, severe pain and therefore diminished opiate use? Further study is needed to determine medical effectiveness of CBD including the effect on concurrent opiate therapy due to competition for receptor sites. This study is the application of a gas chromatography mass spectrometry procedure adapted for use in our laboratory, to detect CBD in urine. The intended use is as a tool for physicians to assess that marijuana being used by a patient is of a composition likely to be medically effective. A law ensuring physicians freedom from federal prosecution would provide confidence essential to formal study of medical uses of marijuana and treatment of clinical problems. Detection of CBD in a urine sample would be a convenient test for such confirmation.
Keywords: laboratory test, assay, medical management
Introduction
Marijuana is classified by the Drug Enforcement Administration as a Schedule I controlled substance. Marijuana is complex, having some 480 natural components and more than 100 cannabinoids. Of the cannabinoids, delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) are the two most prevalent cannabinoids, respectively. The plant, marijuana, and its components are classified as Schedule I. Exceptions are the synthetic cannabinoids, dronabinol (Marinol), a Schedule III compound, and nabilone, which is Schedule II. A Schedule I controlled substance is defined by the Drug Enforcement Administration as a substance having “no currently accepted medical use in the USA, a lack of accepted safety for use under medical supervision, and a high potential for abuse”. A few examples of drugs included in the Schedule I list, in addition to marijuana, are heroin, lysergic acid diethylamide, 3,4-methylenedioxymethylamphetamine (ecstasy), and peyote. Paradoxically, 23 states and the District of Columbia1 have recognized that marijuana has therapeutic benefits and have considered the risk for abuse as an acceptable level of risk. Additionally, 17 states have approved CBD for medical use. This change in the legal status has been substantially driven by voter referendum rather than by scientific studies that have been described as “thin and conflicting”.2 Effectively, this means that these initiatives have been the result of personal choices rather than systematic law based on a substantial body of accepted medical evidence.
Legalization has been heterogeneous.2 The uncertainties of both law and marijuana products inhibit physicians from recommending marijuana for medical care of patients and inhibit the systematic study of the use of marijuana in medical care.3 The physician’s position is problematic in this conundrum, which has been called a “natural experiment”.4
However, as Leung5 has depicted by two case scenarios, it is inevitable that marijuana has already entered into the practices of physicians, whether disclosed by patients or not. The number of patients entering into the practices of physicians may increase since it is likely “marijuana use will rise under legalization”.4
In the interests of supporting physicians and their patients in the use of medically effective forms of marijuana,6 as distinguished from recreational interests, we have adapted a gas chromatography mass spectrometry (GC/MS) procedure for the detection of CBD in urine. The intended use is as a tool for physicians to determine the major components of marijuana being used by a patient and whether that composition is primarily THC, CBD, or a combination of THC and CBD.
Materials and methods
The assay adapted for use in our laboratory was reported by Bergamaschi et al.7 The sample is voided urine without preservative. The volume for testing is 2 mL. Samples are tested undiluted and diluted 10×. The method employs overnight (minimum 12 hours) hydrolysis by B-glucuronidase buffered with potassium phosphate at pH 6. This hydrolysis accounts for Phase II metabolism of CBD to CBD-glucuronide or CBD sulfate. The hydrolysis is followed by liquid–liquid extraction into hexane. The extract is concentrated, followed by derivatization by N,O-bis (trimethylsilyl) trifluoroacetamide (BSTFA) to produce the trimethylsilyl derivatives.
The detection method is a GC/MS procedure performed on an Agilent 6890 GC (gas chromatography) coupled with an Agilent 5973 Mass Selective Detector (Agilent Technologies, Santa Clara, CA, USA). The GC is equipped with a Zebron ZB-5 capillary column (5% phenyl-95% dimethylpolysiloxane liquid phase), 15 m, 0.25 mm internal diometer, 0.25 μm film thickness (Agilent Technologies). The GC uses a temperature ramp of 160°C–250°C at 25°C/min held for 1 minute. Quantitation occurs using the internal standard method.
The following ions are used to quantitate and identify (qualify) the compounds: internal standard (CBD-D3): quantitation: 393, qualifier: 461; CBD: quantitation: 390, qualifiers: 458, 443. The linearity of the assay is 2–100 ng/mL. The limit of detection of the assay is 2 ng/mL. Results are normalized to urine creatinine determined using the Jaffe method.
Two different groups were studied. Group I consisted of specimens from individuals who were submitted for drug screening and confirmation if positive. Forty depersonalized samples were randomly selected from the confirmed positives. The study of the samples in this group was intended to demonstrate that the assay for urine CBD was negative for individuals using THC-rich marijuana. Group II consisted of the study of 15 volunteers who used CBD or CBD-rich marijuana as follows: 12 marijuana using volunteers who agreed to a one time use of a CBD-rich oil capsule; one volunteer used a CBD-rich, THC-poor cigarette; one volunteer used a commercially produced CBD-rich oil capsule; one volunteer used commercially produced herbal (hemp) extract. The study of samples in this group was intended to demonstrate that the assay for urine CBD was positive for individuals known to use CBD-rich marijuana. All samples were also tested for THC by assaying for the metabolite, carboxy-THC.
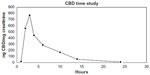
A single volunteer was studied to develop a time profile of the detection time of urinary CBD postdose.
Results
All (40) urine samples in the Group I tested negative for urine CBD. It is likely that this group represented individuals who had used marijuana for recreational purposes. All (40) tested positive for the THC metabolite, carboxy-THC.
The Group II consisted of 15 volunteers dosed with CBD-rich marijuana in different forms: oil, capsule, and cigarette. Urine samples were collected 2 hours postdose. All volunteers tested positive for CBD. Thirty-five urine samples were provided by these 15 volunteers; all urine samples (35) tested positive for CBD. Fourteen out of the 15 volunteers tested positive for carboxy-THC as well as CBD.
This was indicative that the CBD preparation used contained THC and CBD, or there was residual marijuana present from previous marijuana used by the participant. One volunteer smoked a CBD-rich, THC-poor cigarette. This volunteer (1) tested positive for CBD and negative for carboxy-THC, indicative that the cigarette was CBD-rich and low in THC.
One volunteer dosed morning and night for 6 consecutive days. Urine samples were collected 2 hours postdose. All samples (12) tested positive for CBD and carboxy-THC, indicating that the herbal preparation contained CBD and THC. These results indicate that the assay is reliable and useful for identifying the absence or the presence of CBD. In combination with an assay for carboxy-THC, the major cannabinoids present in marijuana used were disclosed.
A time profile was developed for a single volunteer following dosing. Urinary CBD was detected for a 24-hour period (Figure 1).
The results indicate that the assay is applicable to medical marijuana. The study is limited by a small number of individuals studied and also by an absence of information as to the concentration of CBD and THC present in marijuana used by a majority of the volunteers.
Discussion
Patients coming to a physician bring their medical problems as well as their lifestyles including the use of marijuana. It may be helpful in the therapeutic management of patients being treated with marijuana or marijuana extracts, for the physician to have knowledge of the major cannabinoids present in the marijuana used by the patient. This information may not be forthcoming from the patient and the patient who discloses marijuana use may not have specific information with regard to the cannabinoid content of the marijuana used. This assay, particularly in combination with an assay for the THC metabolite, informs the physician of the principle cannabinoids present in the marijuana used. This information may be helpful to the physician in seeking the balance of benefits vs risks6 for a patient using, or wishing to use marijuana for medical therapy. The patient using marijuana for relief of chronic pain may have an altered response to opioids prescribed for pain relief. Opioid sparing has been reported and there may be opportunity to achieve lowered dosage of opioids or avoiding the use of opioids. This is important since opioid therapy may have serious consequences up to and including death due to respiratory depression. Marijuana receptors are not present in the brainstem where the center for respiration is located and for this reason marijuana does not cause respiratory death.8 The presence of CBD or the combination of CBD and carboxy-THC in voided urine is consistent with primary medical intent for use of marijuana. Presence of carboxy-THC is consistent with either primary recreational intent or medical intent. It remains for the physician to determine the significance of marijuana use in medical management of the patient with consideration of the cannabinoids present in urine.
Other confounding factors for the physician include the diverse forms of marijuana used and the variable potency of the marijuana cannabinoids in the different products. The potency of the psychoactive component of marijuana (THC) has increased over time. The physician’s position in this conundrum is problematic. The physician may not prescribe marijuana since that is illegal. In states where legalized, the physician may provide a recommendation that the patient “qualifies” for medical marijuana therapy. Such a recommendation is only a stipulation that the patient may, in essence, self-prescribe. The patient will select the marijuana used from many offerings, perhaps guided by a dispensary. An assay for CBD is an added resource for physicians to identify a marijuana form that may be medically valuable. Further, CBD, although pharmacologically active, is not psychotropic. Strains of marijuana in which CBD is the major cannabinoid have been named Hippie’s disappointment. Such a strain is also known as Charlotte’s Web, named after a young child with intractable seizures alleviated by CBD. Reports of medical benefit include seizures, multiple sclerosis, neurologic disorders with spasms and neurologic pain, pain associated with cancer, rheumatoid arthritis, fibromyalgia, Crohn’s disease, and other autoimmune disorders. Marijuana provides control of nausea and stimulation of appetite in immunosuppressed patients. Migraine headaches, insomnia, and glaucoma are benefitted by medical marijuana.
Marijuana may have anti-inflammatory and neuroprotective properties.
Unfortunately, properly conducted clinical trials are limited. The preponderance of reports are anecdotal or small studies. Patients have used, and will continue to use marijuana for relief of their medical problems. They will seek marijuana from legal dispensaries that predominantly provide psychotropic forms of marijuana. Perhaps 90% or more of these offerings are primarily for recreational use. Patients and physicians need facts to inform their choices among marijuana products. Formal study is needed in the clinical management of patients including evaluation of anti-inflammatory effectiveness, as well as pain alleviation. Use of opiates for chronic pain has led to increasing dosage over time; this may cause respiratory depression that can be fatal. In recognition of dangers associated with opiate treatment of chronic pain, the Medical Board of California offers physicians a course9 in the use of opiates for severe persistent pain for what the Medical Board termed a serious public health crisis of addiction, overdose, and death. Is it feasible that the use of CBD or an optimal concentration of CBD and THC might have significant value in alleviating persistent, severe pain and therefore a diminished need for opiate use, either totally or in lower dosages? It is a responsibility that the medical community holds to provide such a benefit should studies determine marijuana can effectively relieve such pain with opioid sparing. The need for additional study is further indicated by reports of CBD competition for opiate receptor sites.10
Limitations of this study include its small size and the lack of knowing the concentrations of the cannabinoids, THC, and CBD in the marijuana used.
Conclusion
This CBD assay is reliable, and is performed on standard laboratory equipment. The assay is suitable as a convenient test to provide an assessment as to whether CBD is a cannabinoid in marijuana currently being used. Coupled with as assay for urinary carboxy-THC, testing discloses the principle cannabinoids and whether that composition is CBD only, THC only, or a combination of CBD and THC. The physician is provided information that enables a judgment as to the value of marijuana therapy in the patient. Legislative changes, as distinguished from a policy preference by the Department of Justice, that ensured that physicians complying with state laws were not at risk for Federal prosecution would provide confidence; a confidence that is essential to increased formal study of medical uses of marijuana as well as use of medical marijuana as an effective agent for clinical problems.
Legislature that distinguishes medical marijuana from recreational marijuana would inure to the benefit of patients and society as a whole.11
Acknowledgments
Dr Wertlake made a presentation of interim results with abstract at the annual meeting of the American Association for the Advancement of Science, Pacific Region (San Francisco State University, June 15, 2015) and a poster presentation of interim results and abstract at PAINWeek, 2015 (September 2015, Las Vegas, NV).
Disclosure
The authors report no conflicts of interest in this work.
References
ProCon.org. 23 Legal Medical States and DC. Available from: http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881. Accessed January 17, 2016. | |
Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Policy Anal Manage. 2015;34(1):7–31. | |
Bostwick JM. Blurred boundaries: the therapeutics and politics of medical marijuana. Mayo Clin Proc. 2012;87(2):172–186. | |
Pacula RL, Sevigny EL. Marijuana liberalizations policies: why we can’t learn much from policy still in motion. J Policy Anal Manage. 2014;33(1):212–221. | |
Leung L. Cannabis and its derivatives: review of medical use. J Am Board Fam Med. 2011;24(4):452–462. | |
Volkow ND, Baier RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–2227. | |
Bergamaschi M, Barnes A, Queiroz RHC, Hurd YL, Huestis MA. Impact of enzymatic and alkaline hydrolysis on CBD concentration in urine. Anal Bioanal Chem. 2013;405(14):4679–4689. | |
Cannabis and Cannabinoids for Health Professions (PDQ®). August 28, 2015. Available from: http://www.cancer.gov/about-cancer/treatment/cam/hp/cannabis-pdq#section/-3. Accessed January 6, 2016. | |
Medical Board of California. Extended-release and long-acting opioid analgesics risk evaluation and mitigation strategy; 2014. Available from: http://www.fda.gov/downloads/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/UCM311290.pdf. Accessed January 17, 2016. | |
Yamaori S, Koeda K, Kushihara M, Hada Y, Yamamoto I, Watanabe K. Comparison in the in vitro inhibitory effects of major phytocannabinoids and polycyclic aromatic hydrocarbons contained in marijuana smoke on cytochrome P450 2C9 activity. Drug Metab Pharmacokinet. 2012;27(3):294–300. | |
Schatman ME. Medical marijuana: the state of the science. Available from: http://www.medscape.com. 2015. Available from: http://www.topsfield-ma.gov/health/documents/MedicalMarijuana-TheScience.pdf. Accessed January 17, 2016. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.