Back to Journals » Open Access Emergency Medicine » Volume 14
A Retrospective Analysis of Serum D-Dimer Levels for the Exclusion of Acute Aortic Dissection
Authors Zitek T , Hashemi M , Zagroba S , Slane VH
Received 11 May 2022
Accepted for publication 18 July 2022
Published 28 July 2022 Volume 2022:14 Pages 367—373
DOI https://doi.org/10.2147/OAEM.S373335
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Tony Zitek,1 Mani Hashemi,2 Sara Zagroba,2 Valori H Slane2
1Department of Emergency Medicine, Mount Sinai Medical Center, Miami Beach, FL, USA; 2Department of Emergency Medicine, Kendall Regional Medical Center, Miami, FL, USA
Correspondence: Tony Zitek, Department of Emergency Medicine, Mount Sinai Medical Center, 4300 Alton Road, Miami Beach, FL, 33140, USA, Tel +1-305-674-2121 Ext 56632, Email [email protected]
Purpose: Acute aortic dissection (AAD) is a highly fatal disorder if not promptly diagnosed. Some international studies have suggested that serum d-dimer levels may be used to exclude AAD, but data are limited. We sought to confirm that d-dimer levels are elevated in American patients with AAD. Additionally, we sought to estimate the test characteristics of the d-dimer for AAD.
Patients and Methods: We performed a retrospective analysis of patients in the Hospital Corporation of America database who arrived at the hospital between 2015 and 2019. We queried the database to find patients who had a diagnosis of AAD or (nonspecific) chest pain, and who also had a d-dimer performed within 24 hours of arrival at the hospital. The median d-dimer was compared in those diagnosed with AAD versus chest pain. We estimated the test characteristics of d-dimer for AAD at the standard cutoff value of 500 ng/mL.
Results: In total, 48,902 patients met the criteria for analysis, including 572 with AAD and 48,330 with chest pain. The median d-dimers were 2455 ng/mL and 385 ng/mL for the AAD and chest pain groups, respectively (p < 0.0001). Using a cutoff of 500 ng/mL, the sensitivity of the d-dimer was 91.1% and the specificity was 71.4%.
Conclusion: Serum d-dimer values are higher in patients with AAD than in those with nonspecific chest pain. At the standard cutoff of 500 ng/mL, the serum d-dimer has a high sensitivity for AAD, but not high enough that d-dimer levels alone can be used in isolation to exclude AAD.
Keywords: aorta, dissection, d-dimer, diagnosis
Plain Language Summary
Aortic dissection (a splitting of the wall of the aorta) is a rapidly fatal disease if not promptly diagnosed. Currently, aortic dissection is primarily diagnosed with computed tomography angiography of the chest, which is expensive and carries a risk of radiation. Some prior studies have demonstrated that blood levels of a protein fragment called d-dimer are elevated in patients with aortic dissection, but these studies have not been definitive. The authors therefore performed a study to further assess whether blood d-dimer levels may be useful in assessing patients for possible aortic dissection.
The authors used a database from a large hospital system to find patients who had a d-dimer performed and who were either diagnosed with aortic dissection or nonspecific chest pain. In total, the authors analyzed 48,902 patients, including 572 with AAD and 48,330 with nonspecific chest pain. The median d-dimers were 2455 ng/mL and 385 ng/mL for the aortic dissection and chest pain groups, respectively.
Ultimately, blood d-dimer levels were found to be elevated in the vast majority of patients (91%) with aortic dissection, but not all of them. This indicates that a normal blood d-dimer level makes it unlikely that the patient has an aortic dissection, but it does not fully rule out the disease.
Introduction
Acute aortic dissection (AAD) is a highly fatal disorder if not promptly diagnosed, with the rate of mortality reaching 1% to 2% per hour without treatment.1,2 Aortic dissection is primarily diagnosed with computed tomography (CT) angiography of the chest,3 which is expensive, time consuming, and carries a risk of radiation.4 A universal, rapid screening biomarker could thus be very useful to exclude the diagnosis of AAD.
To date, there are several published studies that have evaluated the use of D-dimer to rule-out the diagnosis of AAD,5–15 and there are also systematic reviews and meta-analyses that have aggregated the data.16–20 These publications have reported higher d-dimer levels in patients with AAD as compared to controls, and they have reported that an elevated d-dimer level has a higher sensitivity for AAD. However, some studies have reported as many 12–18% of patients with AAD have a normal d-dimer level.7,9 Additionally, all published studies to date have included relatively small numbers of patients with AAD with the largest having 241 such patients,15 and only one published study has included patients from the United States.5
Some recent publications with European and Asian populations have suggested that the combination of a clinical evaluation and a normal d-dimer value can rule out AAD.14,15 However, as d-dimer values are known to vary by race,21 the d-dimer may have different test characteristics for AAD in an American population. We therefore believe additional American data are needed on this topic.
We performed a retrospective analysis of d-dimer values in a large sample of American patients with AAD and controls. We sought to determine if the standard d-dimer cutoff (500 ng/mL) continues to have a high sensitivity for ruling out AAD, and secondarily we attempted to find a different d-dimer cutoff value that might be more effective in ruling out AAD.
Materials and Methods
Study Design and Setting
This was a retrospective case–control study of patients in the Healthcare Corporation of America (HCA) database. At the time the database was searched, data were available from 118 HCA hospitals, including a variety of hospital types (small, large, community, academic, trauma centers, etc.). These hospitals are located in 19 different states: California, Colorado, Florida, Georgia, Idaho, Indiana, Kansas, Kentucky, Louisiana, Missouri, Mississippi, New Hampshire, Nevada, Oklahoma, South Carolina, Tennessee, Texas, Utah, and Virginia. This study was determined to be exempt from full review by the HCA Healthcare institutional review board (#2020-274). As such, we did not require informed consent; patient data confidentiality was maintained in accordance with the Declaration of Helsinki.
Selection of Participants
Patients who presented to the emergency department (ED) at one of the hospitals in the HCA database between January 1, 2015 and December 31, 2019 were eligible for inclusion in this study. We queried the HCA database to find patients for whom a d-dimer test was performed within 24 hours of arrival at the ED. We then searched among these patients for those who were ultimately diagnosed with an acute aortic dissection (the case group), and for those diagnosed with (nonspecific) chest pain (the control group). Patients who were found to have other diagnoses that might explain their symptoms or cause a d-dimer elevation (such as those with pulmonary embolism or myocardial infarction) were excluded. Any types of AAD according to the DeBakey classification and the Stanford classification were regarded as AAD.22
Data Analysis
D-dimer values were abstracted from the database. Different hospitals in the database use different d-dimer assays; some hospitals report d-dimer values in fibrinogen equivalent units (FEU) and some report in D-dimer units (DDU). We converted all units to FEU by multiplying all values reported in DDU by two.
The median and the following quantiles were calculated for both the AAD and chest pain groups: 1%, 5%, 10%, 25%, 50%, 75%. The d-dimer values in the AAD group were compared to those in the chest pain group using the Wilcoxon Rank Sum Test.
Given that d-dimer values are known to increase with age,23 we wanted to adjust for differences in age between the chest pain and d-dimer groups. Thus, the greedy method of propensity score matching (a technique that can balance covariates) was used to identify a subset of chest pain patients of the same age as the patients in the d-dimer group. After age-matching, a t-test was performed to compare the mean d-dimer values in each group.
The sensitivity and specificity of the standard d-dimer cutoff value (500 ng/mL) were estimated using the final hospital diagnosis as the gold standard. Additionally, we determined the positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio of the cutoff value of 500 ng/mL for AAD. In an attempt to find a d-dimer cutoff value that might be more useful in ruling out an aortic dissection than the standard cutoff value, we calculated the sensitivity and specificity for cutoff values ranging from 200 to 500 ng/mL. Finally, we generated a receiver operating characteristic curve as another means of assessing the utility of the d-dimer value in the diagnostic evaluation of AAD.
Results
Overall, we found 572 patients who met criteria for inclusion in the AAD group, and we found 48,330 patients who met criteria for inclusion in the chest pain group. The demographic characteristics of each group are demonstrated in Table 1. As shown, patients in the AAD group were older and more likely to be male than those in the chest pain group.
 |
Table 1 Demographic Characteristics of Patients in Each Group |
The median d-dimer in the AAD group was 2455 ng/mL (IQR 5827) as compared to 385 ng/mL (IQR 330) in the chest pain group. The difference between the groups of 2070 ng/mL is statistically significant (p < 0.0001). Additional quantiles of d-dimer values for each group are shown in Table 2.
 |
Table 2 A Comparison of the Quantiles for the d-Dimer Values for the AAD Group and the Chest Pain Group |
Using the greedy method, we identified 572 patients in the chest pain group equal in mean age and distribution to the 572 patients in the AAD group. In comparing these groups, the mean d-dimer of AAD patients was 6338 ng/mL and the average d-dimer of chest pain patients was 802 ng/mL (p < 0.0001).
Using a standard cutoff of 500 ng/mL, we found the sensitivity of the d-dimer to be 91.1% (95% CI 88.4–93.3%) and the specificity to be 71.4% (95% CI 71.0–71.8%). The positive predictive value was 3.6% (95% CI 3.5–3.7), and the negative predictive value was 99.9% (95% CI 99.8–99.9%). The positive likelihood ratio was 3.2 (95% CI 3.1 to 3.3), and the negative likelihood ratio was 0.12 (95% CI 0.10–0.16).
The sensitivity and specificity of d-dimer at some other cutoff values are listed in Table 3. The area under the receiver-operating characteristic curve was 0.91 (95% CI 0.89 to 0.92); see Figure 1.
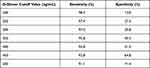 |
Table 3 The Test Characteristics of Various d-Dimer Values for Acute Aortic Dissection |
 |
Figure 1 Receiver operating characteristic curve for d-dimer values and acute aortic dissection. |
Discussion
Limitations
When interpreting the results of this study, there are some limitations to consider. First, we compared patients with AAD to those diagnosed with (nonspecific) chest pain. It is possible that a small percentage of these patients who were diagnosed with nonspecific chest pain had a missed AAD as we did not require patients to have had a gold standard imaging test. If some of those chest pain patients did not get a gold standard imaging test because they had a normal d-dimer value, we may have overestimated the sensitivity of the d-dimer for AAD.
Second, because of the limitations of the HCA database, we did not assess the duration of symptoms of the included patients. Symptom duration is inconsistently documented. The blood d-dimer value is known to decrease with time,24 and so some of the patients in the AAD group may have had a normal d-dimer value if their dissection had already been present for several days. This may have resulted in our estimated sensitivity being lower than it would have been if we restricted d-dimer use to a shorter duration of symptoms.
Finally, our study compared only patients who were ultimately diagnosed with nonspecific chest pain to those with AAD, while all other patients who might have presented with chest pain (such as those with myocardial infarction, pneumonia, and pulmonary embolism) were not included. This may have artificially increased the specificity of the d-dimer for AAD.
Analysis with Respect to Other Studies
This is the first study to evaluate blood d-dimer levels in acute aortic dissection in an exclusively American population. The only other study to include American patients included only a total of 87 patients with AAD, a minority of whom were from the United States.5 This study thus adds value as d-dimer levels are known to vary by race.21 Additionally, this study is unique in that we performed an age-adjusted analysis, and confirmed that the elevations in AAD are independent of age. In general, the data from this study support that from other countries where serum d-dimer values are elevated in the vast majority of patients with AAD.5–15
In our study, the sensitivity of the d-dimer for AAD (91.1%) was a little lower than the 94–95% reported in previous meta-analyses.16,18 Meanwhile, the specificity (71.4%) was a bit higher than the 60% reported in a prior meta-analysis.18 As explained in the limitations section above, these differences are, at least in part, due to differences in methods.
As noted in Table 3, the sensitivity of the d-dimer for AAD could be increased by reducing the cutoff value. However, in doing so, the gains in sensitivity would be small, while the reductions in specificity would be large. Reducing the cutoff would thus minimize any potential benefit the d-dimer could have in avoiding advanced imaging tests in patients for whom AAD was considered. At the current cutoff, the d-dimer could have utility in ruling out AAD as described below.
In our sample, AAD was present in 1.2% of patients. Previous data also demonstrate that AAD is found in only a tiny fraction of patients who present to the ED with chest pain.25 In a sample where AAD is only 1.2% prevalent, the post-test probability of AAD with a d-dimer <500 ng/mL (based on our estimated sensitivity of 91.1%) is 0.1%, a value that most clinicians would consider sufficiently low to rule out AAD. Thus, while a d-dimer is not always elevated in AAD, if a physician can use their clinical evaluation to identify a group of patients with a pre-test probability of AAD around 1%, a d-dimer could potentially be used to rule out AAD. One possible clinical tool to identify a very low-risk group of patients is the aortic dissection detection risk score.26 This tool has performed well in patient populations in Europe and Brazil.15,27,28 Pending validation of the aortic dissection risk score in an American population, the combination of the aortic dissection detection risk score and the d-dimer value could be used to rule out AAD.
Conclusion
In conclusion, patients with acute aortic dissection have higher d-dimer values than those with nonspecific chest pain. The vast majority of (but not all) patients with AAD have a d-dimer value >500 ng/mL. Thus, when used in isolation, a normal d-dimer value does not rule out AAD, but when used with other clinical data, the probability of AAD could be sufficiently low to rule out AAD.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mészáros I, Mórocz J, Szlávi J, et al. Epidemiology and clinicopathology of aortic dissection. Chest. 2000;117(5):1271–1278. doi:10.1378/chest.117.5.1271
2. Asha SE, Miers JW. A systematic review and meta-analysis of D-dimer as a rule-out test for suspected acute aortic dissection. Ann Emerg Med. 2015;66(4):368–378. doi:10.1016/j.annemergmed.2015.02.013
3. Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease - a report of the American College of Cardiology Foundation/American Heart Association Task Force On Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010;121(13):e266–369. doi:10.1161/CIR.0b013e3181d4739e
4. Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med. 2009;169:2078–2086. doi:10.1001/archinternmed.2009.427
5. Suzuki T, Distante A, Zizza A, et al. Diagnosis of acute aortic dissection by D-Dimer The International Registry of Acute Aortic Dissection Substudy on Biomarkers (IRAD-Bio) experience. Circulation. 2009;119(20):2702–2707.
6. Weber T, Högler S, Auer J, et al. D-dimer in acute aortic dissection. Chest. 2003;123(5):1375–1378. doi:10.1378/chest.123.5.1375
7. Paparella D, Malvindi PG, Scrascia G, et al. D-dimers are not always elevated in patients with acute aortic dissection. J Cardiovasc Med. 2009;10(2):212. doi:10.2459/JCM.0b013e32831c849e
8. Sbarouni E, Georgiadou P, Marathias A, Geroulanos S, Kremastinos DT. D-dimer and BNP levels in acute aortic dissection. Int J Cardiol. 2007;122(2):170. doi:10.1016/j.ijcard.2006.11.056
9. Wiegand J, Koller M, Bingisser R. Does a negative D-dimer test rule out aortic dissection? Swiss Med Wkly. 2007;137(31–32):462.
10. Ohlmann P, Faure A, Morel O, et al. Diagnostic and prognostic value of circulating D-Dimers in patients with acute aortic dissection. Crit Care Med. 2006;34(5):1358. doi:10.1097/01.CCM.0000216686.72457.EC
11. Hazui H, Fukumoto H, Negoro N, et al. Simple and useful tests for discriminating between acute aortic dissection of the ascending aorta and acute myocardial infarction in the emergency setting. Circ J. 2005;69(6):677. doi:10.1253/circj.69.677
12. Akutsu K, Sato N, Yamamoto T, et al. A rapid bedside D-dimer assay (cardiac D-dimer) for screening of clinically suspected acute aortic dissection. Circ J. 2005;69(4):397. doi:10.1253/circj.69.397
13. Eggebrecht H, Naber CK, Bruch C, et al. Value of plasma fibrin D-dimers for detection of acute aortic dissection. J Am Coll Cardiol. 2004;44(4):804. doi:10.1016/j.jacc.2004.04.053
14. Nazerian P, Morello F, Vanni S, et al. Combined use of aortic dissection detection risk score and D-dimer in the diagnostic workup of suspected acute aortic dissection. Int J Cardiol. 2014;175:78–82. doi:10.1016/j.ijcard.2014.04.257
15. Nazerian P, Mueller C, Soeiro AM, et al; ADvISED Investigators. Diagnostic accuracy of the aortic dissection detection risk score plus D-Dimer for acute aortic syndromes: the ADvISED prospective multicenter study. Circulation. 2018;137(3):250–258. doi:10.1161/CIRCULATIONAHA.117.029457
16. Marill K. Serum D-Dimer is a sensitive test for the detection of acute aortic dissection: a pooled meta-analysis. J Emerg Med. 2008;34(4):367–376. doi:10.1016/j.jemermed.2007.06.030
17. Shimony A, Filion KB, Mottillo S, Dourian T, Eisenberg MJ. Meta-analysis of usefulness Of D-Dimer To diagnose acute aortic dissection. Am J Cardiol. 2011;107(8):1227–1234. doi:10.1016/j.amjcard.2010.12.027
18. Watanabe H, Horita N, Shibata Y, et al. Diagnostic test accuracy of D-dimer for acute aortic syndrome: systematic review and meta-analysis of 22 studies with 5000 subjects. Sci Rep. 2016;6:26893. doi:10.1038/srep26893
19. Sodeck G, Domanovits H, Schillinger M, et al. D-dimer in ruling out acute aortic dissection: a systematic review and prospective cohort study. Eur Heart J. 2007;28(24):3067–3075. doi:10.1093/eurheartj/ehm484
20. Yao J, Bai T, Yang B, Sun L. The diagnostic value of D-dimer in acute aortic dissection: a meta-analysis. J Cardiothorac Surg. 2021;16(1):343. doi:10.1186/s13019-021-01726-1
21. Pieper CF, Rao KM, Currie MS, Harris TB, Cohen HJ. Age, functional status, and racial differences in plasma D-dimer levels in community-dwelling elderly persons. J Gerontol a Biol Sci Med Sci. 2000;55(11):M649–57. doi:10.1093/gerona/55.11.M649
22. Criado FJ. Aortic dissection: a 250-year perspective. Tex Heart Inst J. 2011;38(6):694–700.
23. Harper PL, Theakston E, Ahmed J, Ockelford P. D-dimer concentration increases with age reducing the clinical value of the D-dimer assay in the elderly. Intern Med J. 2007;37(9):607–613. doi:10.1111/j.1445-5994.2007.01388.x
24. Chapman CS, Akhtar N, Campbell S, et al. The use of D-Dimer assay by enzyme immunoassay and latex agglutination techniques in the diagnosis of deep vein thrombosis. Clin Lab Haematol. 1990;12:37–42. doi:10.1111/j.1365-2257.1990.tb01108.x
25. Alter SM, Eskin B, Allegra JR. Diagnosis of aortic dissection in emergency department patients is rare. West J Emerg Med. 2015;16(5):629–631. doi:10.5811/westjem.2015.6.25752
26. Tsutsumi Y, Tsujimoto Y, Takahashi S, et al. Accuracy of aortic dissection detection risk score alone or with D-dimer: a systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care. 2020;9(3_suppl):S32–S39. doi:10.1177/2048872620901831
27. Nazerian P, Giachino F, Vanni S, et al. Diagnostic perfor- mance of the aortic dissection detection risk score in patients with suspected acute aortic dissection. Eur Heart J Acute Cardiovasc Care. 2014;3:373–381. doi:10.1177/2048872614527010
28. Gorla R, Erbel R, Kahlert P, et al. Accuracy of a diagnostic strategy combining aortic dissection detection risk score and D-dimer levels in patients with suspected acute aortic syndrome. Eur Heart J Acute Cardiovasc Care. 2017;6:371–378. doi:10.1177/2048872615594497
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
