Back to Journals » Clinical Interventions in Aging » Volume 13
A randomized-controlled trial pilot study examining the effect of extracorporeal magnetic innervation in the treatment of stress urinary incontinence in women
Authors Weber-Rajek M , Radzimińska A , Strączyńska A , Podhorecka M, Kozakiewicz M , Perkowski R, Jarzemski P , Kędziora-Kornatowska K , Goch A
Received 17 July 2018
Accepted for publication 23 October 2018
Published 4 December 2018 Volume 2018:13 Pages 2473—2480
DOI https://doi.org/10.2147/CIA.S176588
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Magdalena Weber-Rajek,1 Agnieszka Radzimińska,1 Agnieszka Strączyńska,1 Marta Podhorecka,2 Mariusz Kozakiewicz,3 Radosław Perkowski,2 Piotr Jarzemski,4 Kornelia Kędziora-Kornatowska,2 Aleksander Goch1
1Department of Physiotherapy, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Toruń, Toruń, Poland; 2Department of Geriatrics, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Toruń, Toruń, Poland; 3Department of Food Chemistry, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Toruń, Toruń, Poland; 4Clinic of Urology, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Toruń, Toruń, Poland
Introduction: Peri- and postmenopausal women frequently suffer from urinary incontinence (UI). Generally, UI becomes more severe with age. It impacts physical, mental, and social functioning as well as the quality of life, often leading to depression. Extracorporeal magnetic innervation (ExMI) is a relatively new conservative treatment method for UI.
Objective: The aim of the study was to assess the effectiveness of ExMI in the treatment of stress UI in women.
Methods: A total of 52 women were included in the analysis: 28 participants were allocated to the experimental group (EG) and 24 to the control group (CG). The average age was 65.41 years (±SD 4.08). EG patients completed ExMI therapy. The treatment sessions lasted for 15 minutes, and occurred three times a week, for 4 weeks. No therapeutic intervention was applied to the CG. To objectify the treatment outcomes in both groups before and after the treatment, we measured myostatin concentration and performed the UI severity assessment (The Revised Urinary Incontinence Scale), perceived self-efficacy assessment (General Self-Efficacy Scale), and depression severity assessment (Beck Depression Inventory).
Results: The authors compared the EG results at the initial and final assessments and found a statistically significant improvement in severity of UI (P=0.001) and depression severity (P=0.006), and a decrease in myostatin concentration (P≤0.001). The authors did not find any statistically significant differences between all measured variables for the CG at the initial and final assessments. Furthermore, there were no statistically significant differences between all measured variables for the EG and the CG at the final assessment.
Conclusion: Further trials are needed to determine optimal treatment protocols for various UI types and to evaluate long-term outcomes of the ExMI treatment.
Keywords: stress urinary incontinence, Extracorporeal Magnetic Innervation
Introduction
The International Continence Society (ICS) and the International Urogynecological Association objectively define urinary incontinence (UI) as any involuntary leakage of urine reported by an individual.1 UI is a relatively common condition in peri- and postmenopausal women. According to the Standardization Steering Committee, there are three main UI types: urge urinary incontinence (UUI), stress urinary incontinence (SUI), and mixed urinary incontinence (MUI).2 SUI is considered to be the most common form of UI. The condition itself is caused by pelvic floor muscle weakness, which affects urethral closure. During the peri- and postmenopausal period, various mechanisms can lead to pelvic floor muscle weakness. Among these are hormonal changes, type II myofiber atrophy, inflammatory mediators, reduced supply of calories and proteins, limited physical activity, and alterations in protein synthesis, including myostatin.3,4 Myostatin concentration increases during skeletal muscle inactivity, whereas the inhibition of serum myostatin contributes to an increase in muscle mass and strength.5,6 Therapeutic interventions can suppress myostatin signaling to ameliorate the effects of advancing age on skeletal muscle function and mass.7 Certain studies suggest that myostatin inhibits human urethral rhabdosphincter satellite cell proliferation. Consequently, the inhibition of myostatin function might be considered an effective strategy in SUI treatment.8
In addition to somatic symptoms, UI can contribute to serious social and psychological consequences, such as social isolation, anxiety, depression, and low self-esteem. Therefore, delivering a holistic approach and seeking potential mental resources required for people to actively care for and improve their own health is particularly important. One of the important mental resources is general self-efficacy. Ralf Schwarzer emphasizes the importance of self-efficacy in adopting health behaviors, as it plays a paramount role in anticipating preventive actions, modification of harmful habits, and adherence to health behaviors. Individuals with high self-efficacy use their mental resources better, and they are more eager to modify their behavior and adhere to the changes.9 The higher self-efficacy beliefs people have, the more likely they are to adhere to health-related behaviors, as they strongly believe that they can overcome obstacles and achieve their goals. Self-efficacy beliefs are considered a key predictor of adherence to health-related behaviors.10 There are some studies that demonstrate a relationship between self-efficacy beliefs, depression, and quality of life of patients with UI. Depression correlates negatively with self-efficacy beliefs, which means that low self-efficacy is conducive to the occurrence of depression. On the other hand, self-efficacy beliefs correlate positively with quality of life, and higher self-efficacy promotes better quality of life.11–13
According to the 2017 European Association of Urology guidelines on the assessment and nonsurgical management of UI, the available therapies are pelvic floor muscle training (PFMT), bladder training (BT), electrical stimulation, magnetic stimulation, and posterior tibial nerve stimulation.14
Extracorporeal magnetic innervation (ExMI) is a noninvasive treatment option. In ExMI, the patient sits on a special chair, in which the seat is equipped with a therapy head. The chair produces a magnetic field which penetrates the pelvis minor organs, acting directly on the motor fibers of visceral and pudendal nerves. The induction values are greater than those compared with conservative magnetotherapy, and therefore, the patient feels distinct pelvic floor muscle contractions. Once active sodium–potassium pump and depolarized motor neurons induce impulses which reach the neuromuscular plates, the muscles respond by contracting.15,16
There is relatively little scientific evidence assessing the therapy’s efficacy in UI treatment. Hence, the authors decided to explore the idea further and conduct the following study.
Objective
The aim of the study was to assess the effectiveness of ExMI therapy in the treatment of SUI in women.
Methods
Study design
Between March and May 2017, 71 participants suffering from SUI and UUI were enrolled into a randomized, double-blind, controlled study. The following was conducted in accordance with the principles of the Declaration of Helsinki. The authors of this study obtained an approval from the Bioethics Committee of the Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Torun (768/2016 CM UMK). Moreover, a statement confirming written informed consent was obtained from all the participants. All deidentified data included in this are contained within this report. The researchers used a simple method to ensure stratified randomization. All the subjects were allocated to respective groups by picking envelopes with a random, computer-generated group allocation number. The main investigator was blinded to the intervention group allocation. Of the 16 women excluded from the study, 14 patients did not meet the inclusion criteria and 2 patients refused to participate. Then, each of the 55 participants was randomly assigned to the experimental group (EG) or the control group (CG). Of the three women who did not complete the study, two women withdrew from the EG during the 4-week treatment program, while one woman from the CG missed the final study visit. As a result, 52 women (aged 61–76 years) have successfully completed the study (EG, n=28; CG, n=24). The RCT reporting quality was improved using the CONSORT statement (Consolidated Standards of Reporting Trials; Figure 1).17
  | Figure 1 The study flow diagram. |
Prior to the treatment, each study participant was asked to provide information about the circumstances of urine loss, contraindications to the treatment, and the presence of comorbid conditions. Additionally, the type of UI was determined using the Questionnaire for Urinary Incontinence Diagnosis (QUID). The QUID is a six-item UI symptom questionnaire used to diagnose SUI and UUI. Because of acceptable psychometric characteristics, the QUID can be used in clinical trials as a UI outcome measure.18
Study inclusion criteria were as follows: diagnosed SUI, and no contradictions to the ExMI treatment (pregnancy, recent pelvic fractures, fever, acute inflammations, active malignancy, uterine tumors and myomas, stage 3 uterine prolapse, hemorrhoids, urinary or genital tract infections, suspected urethral and/or vesical fistula, severe urethral sphincter weakness and/or defect, deep vein thrombosis, acute infections, cardiac arrhythmia, cardiac pacemaker, and neurological diseases). Study exclusion criteria were as follows: presence of contraindications to the ExMI treatment, diagnosed MUI and UUI, recent therapeutic interventions in UI within 3 months prior to the study (PFMT, magnetotherapy, electrostimulation, and biofeedback).
Measurements
To objectify the results, the authors measured myostatin concentration for the EG and CG before and after the treatment and also performed the perceived self-efficacy assessment (The General Self-Efficacy Scale [GSES]), the urinary incontinence severity assessment (The Revised Urinary Incontinence Scale [RUIS]), and depression severity assessment (Beck Depression Inventory [BDI]).
Myostatin concentration
The study design follows the procedure for the determination of myostatin in human serum and plasma included in the Myostatin ELISA manual (Immundiagnostik AG, Bensheim, Germany; cat. no: K 1012). Six milliliters of blood was collected from each participant on empty stomach into Vacuette tubes with EDTA anticoagulant. Afterward, the collected samples were centrifuged at 3,000 rpm for 15 minutes to obtain plasma, which was then pipetted into smaller samples of about 500 μL, and frozen at −80°C. Then, the authors used the BMG Labtech ELISA absorbance reader with a monochromator to read the results. Consequently, the assay allowed for quantitative determination of myostatin in EDTA plasma and serum samples. Firstly, the researchers added a biotinylated myostatin tracer to the samples, controls, and standards. Next, they transferred and incubated aliquots of the treated preparations into microtiter plate wells coated with polyclonal anti-myostatin antibodies. Once the incubation phase commences, the free target antigen in the samples competes with the biotinylated myostatin tracer, and afterward it binds with the polyclonal anti-myostatin antibodies immobilized on the microtiter plate wells. At the washing step, the researchers removed the unbound components. During the second incubation step, each microtiter well received a streptavidin-labeled peroxidase antibody, which binds to the biotinylated myostatin tracer. After removing the unbound components at the washing step, the researchers added peroxidase substrate tetramethylbenzidine (TMB). In the final step, the acidic stop solution terminated the enzymatic reaction and changed the sample color from blue to yellow. It is essential to note that the yellow color intensity is inversely proportional to myostatin concentration. The sample color intensity was measured at 450 nm. The weaker photometric signal is the consequence of high myostatin concentration, which affects the sample by lowering the concentration of the biotinylated myostatin tracer bound to the immobilized anti-myostatin antibodies.
The Revised Urinary Incontinence Scale
The authors used the RUIS, which is a valid five-item scale that is designed to assess UI and to monitor posttreatment outcomes. A score of 0–3 represents non-UI, 4–8 represents mild UI, and 9–12 represents moderate UI, and a score of ≥13 is considered severe UI.19
BDI-II
Since its original publishing date, the BDI questionnaire has been the most widely used self-report depression scale. The tool is used in research on mental disorders and to assess the mood of patients suffering from various medical conditions, including oncological, urological, gynecological, and neurological diseases. The BDI-II questionnaire is a 21-item scale with individual item scores ranging from 0 (no symptoms) to 3 (severe symptoms). A total score of 0–8 is considered as no depression, 9–18 indicates moderate depression, and a score of 18+ is considered as severe depression.20
The General Self-Efficacy Scale developed by Matthias Jerusalem and Ralf Schwarzer
The scale evaluates one psychometric characteristic – the general self-efficacy belief in one’s ability to effectively deal with a wide array of situations. The raw scores are afterward transformed into standardized sten scores. The higher the score, the higher are self-efficacy beliefs. Score ranges are defined as follows: 1–4 sten, low scores; 5–6 sten, average scores; and 7–10 sten, high scores.21
Intervention
EG patients completed the therapy. The treatment sessions lasted 15 minutes each, and occurred three times a week, for 4 weeks. Therapy was performed using the NeoControl chair (Neotonus Inc., Marietta, GA, USA). The following magnetic field parameters were used: 2.0 Tesla at 50 Hz, delivered for 8 seconds with a dwell time of 4 seconds. The intensity increased from 20% to 100% during consecutive treatment sessions. Also, the strength of electromagnetic stimulation matched the highest patient-tolerated level.
Statistical analyses
The authors analyzed the collected data using the Statistica 13.1 software. Also, the Shapiro–Wilk test was implemented to check the normality distribution of measured variables. The mean and SD were calculated for variables that showed normal distribution. Differences between the two groups were estimated using the independent variable Student’s t-test. Whereas, the dependent variable Student’s t-test was used to check differences within one group. The statistical significance level was defined as P<0.05.
Results
Table 1 includes Student’s t-test results and descriptive statistics for all measured variables for the EG and the CG, obtained at the initial assessment.
After comparing the Student’s t-test P-value with the significance level of α=0.05, the authors discovered that there are no statistically significant differences between the EG and CG results obtained at the initial assessment. This finding confirmed the homogeneity of the study groups.
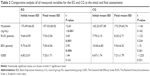
Student’s t-test results and descriptive statistics for all measured variables for the EG and the CG at the initial and final assessments are presented in Table 2. After comparing the Student’s t-test P-value with the significance level of α=0.05, the authors found a statistically significant decrease in myostatin concentration, improvement in severity of UI, and depression severity between the EG results at the initial and final assessments. Then, the authors compared the Student’s t-test P-value with the significance level of α=0.05 and they did not notice any statistically significant differences in perceived self-efficacy between the EG results at the initial and final assessments. The authors also compared the Student’s t-test P-value with the significance level of α=0.05, and they did not notice any statistically significant differences in all measured variables between the CG results at the initial and final assessments.
Table 3 includes Student’s t-test results and shows descriptive statistics for all measured variables for the EG and the CG at the final assessment. After comparing the Student’s t-test P-value with the significance level of α=0.05, the authors did not notice any statistically significant differences between all measured variables for the EG and the CG at the final assessment.
Discussion
ExMI is a relatively new conservative treatment method for UI. By comparing the EG results at the initial and final assessments, we found a statistically significant improvement in the severity of UI (P=0.001) and depression (P=0.006), and a decrease in myostatin concentration (P≤0.001).
The available evidence and few studies incorporating various research designs confirm the efficacy of ExMI. Nevertheless, it seems that researchers have not determined optimal parameters of the magnetic field. In their study, Gilling et al22 randomly assigned 70 patients with urodynamically confirmed SUI into two groups: the EG (n=35) and the sham group (n=35). All study participants were assessed using the following tools: 20-minute provocative pad-test, 3-day bladder diary, 24-hour pad test, pelvic floor muscle contraction analysis, the quality of life scale in patients with UI (I-QOL), the King’s Health Questionnaire, and video-urodynamic studies. The following stimulation parameters were used: 10 Hz for 10 minutes, 3 minutes rest, 50 Hz for 10 minutes. The magnetic field intensity matched the highest patient-tolerated level. Patients from the sham group followed the same treatment schedule. Nonetheless, the chair used during their therapy sessions contained a thin deflective aluminum plate. The inserted plate prevented the magnetic field from penetrating the patient’s body, and it also simulated the sensation and noise typically present during active treatment sessions. The therapy lasted for 6 weeks. Overall, significant improvements were observed in each of the primary and secondary outcome measures in the study group of 70 women. Furthermore, the authors found significant improvements in primary and secondary outcome measures after comparing the active treatment group results with the baseline measures. It should be noted that compared with the sham treatment group, these improvements were deemed statistically insignificant.
Yokoyama et al23 enrolled 20 patients with UUI and 17 women with SUI into their study. Treatment sessions lasted for 20 minutes each, and occurred twice a week, for 8 weeks. The authors applied the following frequency of the pulsed magnetic field:10 Hz for 10 minutes, 2 minutes rest, 50 Hz for 10 minutes. Women were assessed using the following tools: urodynamic study, 5-day bladder diary, Visual Analog Scale, and the quality-of-life survey (I-QOL). Among patients with UUI, 5 women were cured (25.0%), 12 women improved (60.0%), and 3 women felt that there was no improvement (15.0%). Among patients with SUI, nine women were cured (52.9%), seven women improved (41.1%), and one woman showed no improvement (6%).
Hoşcan et al24 examined a group of 30 patients with SUI. To objectify the treatment outcomes before and after the treatment, the researchers used a dynamic pad weight test, 3-day bladder diary, urodynamic study, and a validated quality of life survey. Treatment sessions lasted for 20 minutes each, and occurred twice a week, for 6 weeks. The following frequency of the pulsed magnetic field was used: 5 Hz intermittently for 10 minutes, 1–5 minutes rest, followed by a second treatment at 50 Hz intermittently for 10 minutes. Once the ExMI therapy was completed, 8 out of the 27 women were cured (29.7%), whereas 13 women were improved (48.1%) at 3 months. Overall, the ExMI treatment had a cumulative success rate of 77.8%. It should be noted that six patients showed no improvement after the treatment.
Vadala et al25 studied 20 patients with various types of UI (SUI, UUI, and MUI) who were exposed to magnetic stimulation. The following treatment parameters were used: 10 Hz for 10 minutes, 35 Hz for another 10 minutes, 6 seconds rest (active time and pause time). Treatment sessions lasted for 20 minutes each, and occurred twice a week, for 3 weeks (six sessions total). All patients were assessed using the following: a urodynamic test, urinary diaries, the Overactive Bladder Symptom Questionnaire (OAB-q), Incontinence Impact Questionnaire-Short Form (IIQ-7), and the Urogenital Distress Inventory Questionnaire-Short Form (UDI-6). Significant reductions in nocturia and micturition number were observed after the magnetic treatment. The researchers assessed changes in UI symptoms by comparing life stress scores and urodynamic test results obtained before functional magnetic stimulation with those obtained at 3 weeks after the treatment. During urodynamic tests, the authors noted a substantial increase in maximum urethral closure pressure, cystometric capacity, urethral functional length, and pressure transmission ratio when compared with baseline. There was a statistically significant improvement in patients’ responses from all life stress questionnaires.
In this study, we used RUIS to objectify the treatment outcomes and UI severity in both groups at the initial and final assessments. The EG results at the initial assessment were as follows: mild UI in eleven study participants (39%), moderate UI in nine study participants (32%), and severe UI in eight study participants (29%). The EG results at the final assessment were as follows: non-UI in 5 study participants (18%), mild UI in 9 study participants (32%), and moderate UI in 14 study participants (50%). The CG results at the initial assessment were as follows: mild UI in 18 study participants (75%) and moderate UI in 6 study participants (25%). The CG results at the final assessment were as follows: mild UI in 14 study participants (59%) and moderate UI in 10 study participants (41%). These results confirm the effectiveness of the treatment and also indicate that the lack of therapeutic intervention can contribute to worsening of UI symptoms.
The BDI was used to assess depression severity among the patients. The EG results at the initial assessment were as follows: no depression in 14 patients (50%), moderate depression in 10 patients (36%), and severe depression in 4 patients (14%). The EG results at the final assessment were as follows: no depression in 18 patients (65%), moderate depression in 9 patients (32%), and severe depression in 1 patient (3%). The CG results at the initial assessment were as follows: no depression in 12 patients (50%), moderate depression in 10 patients (42%), and severe depression in 2 patients (8%). The CG results at the final assessment were as follows: no depression in 12 patients (50%), moderate depression in 9 patients (38%), and severe depression in 3 patients (12%). The literature lists various comorbid conditions that are associated with UI, among which depression continues to be the most common psychiatric condition.26,27 Psychological factors play a crucial role in the prevention and treatment of UI. The ICS takes great care, in its definition of UI, to embrace its association with psychological and psychosocial factors.28
The other parameter measured was the myostatin concentration, which increases during skeletal muscle inactivity. Moreover, the inhibition of serum myostatin contributes to an increase in muscle mass and strength. The authors observed a statistically significant decrease in myostatin concentration (P<0.001) in the EG at the final assessment. Whereas, no statistically significant differences in myostatin concentration were reported for the CG (P=0.162) at the final assessment. To our knowledge, this is the first study that assesses myostatin concentration after ExMI.
In this study, the authors also examined self-efficacy beliefs. No statistically significant differences in the GSES score were observed at the initial and final assessments. However, it should be noted that the EG and CG reported relatively high self-efficacy before the treatment (6.82 sten vs 6.67 sten). We can assume that high self-efficacy in women from both groups encouraged them to take action and face the problem of UI. Numerous studies demonstrated a relationship between positive adherence rates, high self-efficacy, and discussed treatment method for UI.29–32 An additional aim of our study was to maintain high self-efficacy beliefs both in the EG and the CG. Contact details were collected to inform participants about future UI studies. Furthermore, the CG was qualified for a treatment program at a later date.
It should be noted that the presented study protocol is not ideal due to several factors present in this study as well as in a series of small studies. Many women volunteered for this study; however, we could gather a relatively small EG due to numerous ExMI exclusion criteria. Because of the nature of the treatment (patients feel pelvic floor muscle contractions), it is difficult to design a double-blind, sham-controlled trial. Moreover, it would be necessary to evaluate long-term treatment outcomes. We also found that patients who felt noticeable pelvic floor muscle contractions were more aware of that muscle group. As a result, the studied patients were better prepared to PFMT.
Conclusion
This study found that ExMI can be an effective treatment method for SUI. ExMI decreases myostatin concentration, UI symptoms, and depression symptoms in women with SUI. This is a pilot study. Thus, the authors plan to perform further studies on a larger EG and assess long-term treatment outcomes. Moreover, further trials are needed to determine optimal treatment protocols for different UI types.
Disclosure
The authors report no conflicts of interest in this work.
References
Bo K, Frawley HC, Haylen BT, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Neurourol Urodyn. 2017;36(2):221–244. | ||
National Collaborating Centre for Women’s and Children’s Health (UK). Urinary Incontinence in Women: The Management of Urinary Incontinence in Women. London: Royal College of Obstetricians and Gynaecologists; 2006:1–389. | ||
McGrother CW, Donaldson MM, Hayward T, et al; Leicestershire MRC Incontinence Study Team. Urinary storage symptoms and comorbidities: a prospective population cohort study in middle-aged and older women. Age Ageing. 2006;35(1):16–24. | ||
Doherty TJ. Invited review: aging and sarcopenia. J Appl Physiol. 2003;95(4):1717–1727. | ||
Joulia-Ekaza D, Cabello G. Myostatin regulation of muscle development: molecular basis, natural mutations, physiopathological aspects. Exp Cell Res. 2006;312(13):2401–2414. | ||
Whittemore LA, Song K, Li X, et al. Inhibition of myostatin in adult mice increases skeletal muscle mass and strength. Biochem Biophys Res Commun. 2003;300(4):965–971. | ||
Lynch GS. Emerging drugs for sarcopenia: age-related muscle wasting. Expert Opin Emerg Drugs. 2004;9(2):345–361. | ||
Akita Y, Sumino Y, Mori K, Nomura T, Sato F, Mimata H. Myostatin inhibits proliferation of human urethral rhabdosphincter satellite cells. Int J Urol. 2013;20(5):522–529. | ||
Schwarzer R. Self-efficacy in the adoption and maintenance of health behaviors: theoretical approaches and a new model. In: Schwarzer R, editor. Self-efficacy: Thought Control of Action. Washington, DC: Hemisphere Publishing Corp.;1992:217–243. | ||
Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–164. | ||
Bandura A. Aevolução da teoria social cognitiva. In: Bandura A, Azzi RG, Polydoro S, editors. Teoria Social Cognitiva: Conceitos Básicos. Artmed: Porto Alegre; 2008:176. | ||
Yusaf SO, Kavanagh DJ. Mechanisms of improvement in treatment for depression: test of a self-efficacy and performance model. J Cogn Psychother. 1990;4:51–70. | ||
Broome BA. Development and testing of a scale to measure self-efficacy for pelvic muscle exercises in women with urinary incontinence. Urol Nurs. 1999;19(4):258–268. | ||
Nambiar AK, Bosch R, Cruz F, et al. EAU Guidelines on Assessment and Nonsurgical Management of Urinary Incontinence. Eur Urol. 2018;73(4):596–609. | ||
Galloway NT, El-Galley RE, Sand PK, Appell RA, Russell HW, Carlan SJ. Extracorporeal magnetic innervation therapy for stress urinary incontinence. Urology. 1999;53(6):1108–1111. | ||
Galloway NT, El-Galley RE, Sand PK, Appell RA, Russell HW, Carlin SJ. Update on extracorporeal magnetic innervation (EXMI) therapy for stress urinary incontinence. Urology. 2000;56(6 Supp 1):82–86. | ||
Diallo S, Cour F, Josephson A, et al. Evaluating single-incision slings in female stress urinary incontinence: the usefulness of the CONSORT statement criteria. Urology. 2012;80(3):535–541. | ||
Bradley CS, Rahn DD, Nygaard IE. The questionnaire for urinary incontinence diagnosis (QUID): validity and responsiveness to change in women undergoing non-surgical therapies for treatment of stress predominant urinary incontinence. Neurourol Urodyn. 2010;29(5):727–734. | ||
Sansoni J, Hawthorne G, Marosszeky N. The Technical Manual for the Revised Incontinence and Patient Satisfaction Tools. NSW, Australia: University of Wollongong; 2011. | ||
Beck AT, Steer RA, Brown GK. BDI-II. Beck Depression Inventory. Manual. San Antonio: The Psychological Corporation; 1996. | ||
Schwarzer R, Jerusalem M. Generalized Self-Efficacy Scale. In: Weinman J, Wright S, Johnston M, editors. Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs. Windsor, UK: NFER-NELSON;1995:35–37. | ||
Gilling PJ, Wilson LC, Westenberg AM, et al. A double-blind randomized controlled trial of electromagnetic stimulation of the pelvic floor vs sham therapy in the treatment of women with stress urinary incontinence. BJU Int. 2009;103(10):1386–1390. | ||
Yokoyama T, Fujita O, Nishiguchi J, et al. Extracorporeal magnetic innervation treatment for urinary incontinence. Int J Urol. 2004;11(8):602–606. | ||
Hoşcan MB, Dilmen C, Perk H, et al. Extracorporeal magnetic innervation for the treatment of stress urinary incontinence: results of two-year follow-up. Urol Int. 2008;81(2):167–172. | ||
Vadala M, Palmieri B, Malagoli A, Laurino C. High-power magnetotherapy: a new weapon in urinary incontinence? Low Urin Tract Symptoms. 2018;10(3):266–270. | ||
van Gerwen M, Schellevis F, Lagro-Janssen T. Comorbidities associated with urinary incontinence: a case-control study from the Second Dutch National Survey of General Practice. J Am Board Fam Med. 2007;20(6):608–610. | ||
Steers WD, Lee KS. Depression and incontinence. World J Urol. 2001;19(5):351–357. | ||
Abrams P, Cardozo L, Fall M, et al; Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21(2):167–178. | ||
Tannenbaum C, Brouillette J, Michaud J, et al. Responsiveness and clinical utility of the geriatric self-efficacy index for urinary incontinence. J Am Geriatr Soc. 2009;57(3):470–475. | ||
Messer KL, Hines SH, Raghunathan TE, Seng JS, Diokno AC, Sampselle CM. Self-efficacy as a predictor to PFMT adherence in a prevention of urinary incontinence clinical trial. Health Educ Behav. 2007;34(6):942–952. | ||
Chen SY, Tzeng YL. Path analysis for adherence to pelvic floor muscle exercise among women with urinary incontinence. J Nurs Res. 2009;17(2):83–92. | ||
Sacomori C, Cardoso FL, Porto IP, Negri NB. The development and psychometric evaluation of a self-efficacy scale for practicing pelvic floor exercises. Braz J Phys Ther. 2013;17(4):336–342 English, Portuguese. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.