Back to Journals » Risk Management and Healthcare Policy » Volume 14
A Quantitative Evaluation of Evidence-Based Beliefs and Implementation Among Community Pharmacists: Findings and Impact from United Arab Emirates
Authors Jairoun AA , Al-Hemyari SS , Shahwan M , El-Dahiyat F , Jairoun M, AL-Tamimi SK , Mothana RA , Khattab AH
Received 28 September 2020
Accepted for publication 27 January 2021
Published 9 March 2021 Volume 2021:14 Pages 967—977
DOI https://doi.org/10.2147/RMHP.S283068
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Marco Carotenuto
Ammar Abdulrahman Jairoun,1,2 Sabaa Saleh Al-Hemyari,2,3 Moyad Shahwan,4,5 Faris El-Dahiyat,6 Maimona Jairoun,4 Saleh Karamah AL-Tamimi,7 Ramzi A Mothana,8 Ahmed Husham Khattab4
1Health and Safety Department, Dubai Municipality, Dubai, United Arab Emirates; 2Discipline of Social and Administrative Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, Penang, 11500, Malaysia; 3Department of Pharmacy, Ministry of Health and Prevention, Dubai, United Arab Emirates; 4Department of Clinical Sciences, College of Pharmacy and Health Sciences, Ajman University, Ajman, 346, United Arab Emirates; 5Center of Medical and Bio-allied Health Sciences Research, Ajman University, Ajman, Ajman, 346, United Arab Emirates; 6College of Pharmacy, Al Ain University, Al Ain, United Arab Emirates; 7Faculty of Pharmacy, Aden University, Aden, Yemen; 8Department of Pharmacognosy, College of Pharmacy, King Saud University, Riyadh, Saudi Arabia
Correspondence: Ammar Abdulrahman Jairoun
Health and Safety Department, Dubai Municipality, Dubai, 67, United Arab Emirates
Tel +971558099957
Email [email protected]
Background: The flux of pharmaceutical data can have a negative impact on the complexity of a pharmacist’s decision-making process, which will demand an extensive evaluation from healthcare providers trying to choose the most suitable therapeutic plans for their patients.
Objective: The current study aimed to assess the beliefs and implementations of community pharmacists in the UAE regarding evidence-based practice (EBP) and to explore the significant factors governing their EBP.
Setting: Community pharmacies in Dubai and the Northern Emirates, UAE.
Methods: A descriptive cross-sectional study was conducted over six months between December 2017 and June 2018. Community pharmacists who had three months’ professional experience or more and were registered with one of three regulatory bodies (Ministry of Health, Health Authority Abu Dhabi, or Dubai Health Authority) were interviewed by three trained final-year pharmacy students. Face-to-face interviews were then carried out and a structured questionnaire was used.
Metrics: The average beliefs score was 36% (95% CI: [34%, 39%]) compared to an implementation score of 35% (95% CI: [33%, 37%]).
Results: A total of 505 subjects participated in the study and completed the entire questionnaire. On average, participants scored higher in beliefs score than implementation score. The results of the statistical modelling showed that younger, female, higher-position pharmacists with more experience and with low percentages of full-time working, and graduates from international/regional universities were more likely to believe in and implement the concept of EBP.
Conclusion: A gap was identified between the beliefs and implementation of EBP. Developing educational EBP courses in undergraduate pharmacy curricula is of high importance, not only to increase knowledge levels but also to encourage commitment in those pharmacists to strive for professionalism and to support the provided patient care with evidence.
Keywords: evidence-based practice, beliefs, practice, community pharmacist
Introduction
With the increasing numbers and types of medications on the market, alongside the abundance of information about the medications and their corresponding diseases, the reliability of the evidence is of the utmost importance. The flux of these pharmaceutical data can have a negative impact on the complexity of a pharmacist’s decision-making process, which will demand an extensive evaluation from healthcare providers to choose the most suitable therapeutic plans for their patients.1 The major objective of any healthcare is to weigh the benefits obtained from the treatment against the risk this treatment might have on the patient’s health, both in the short and long terms.2 Even though treatments are designed to improve a patient’s overall quality of life, there have been many examples over the years of treatments that actually worsened a patient’s health status after treatment compared to their overall health before starting it, which goes against everything pharmaceutical care intends to achieve.3,4 The definition of pharmaceutical care was first introduced in 1990 by Doug Hepler and Linda Strand as the responsibility of a healthcare provider to supervise and provide an accurate drug therapy that serves the purpose of eliminating the patient’s set of symptoms, eradicating a present illness, slowing it down, or preventing an expected illness while inducing minimal side effects associated with the drug therapy.5
The implementation of pharmaceutical care provides a supplementary value to the clinical outcome by reinforcing active involvement in the treatment journey. For the proper application of pharmaceutical care, high-quality training of pharmacists must be in line with the establishment of skills in patient management, assessment, counselling, and education. The elemental principle of evidence-based medicine is to perform all the needed clinical decisions based on literature. This process is integrated with the creation of patient-specific pharmacist care outlines, treatment guidelines, dosage interventions, selection of appropriate therapeutic alternatives, and preventive measures. Evidence-based medicine is not easy to implement in daily practice, and there is a vital need to compensate for the gaps in pharmacists’ basic knowledge by recommending supportive information systems that can help to minimize errors, i.e., there is a true need to make a curriculum that is sensitive to the development of evidence-based pharmacy skills.3
A pharmaceutical care plan will be considered based on evidence supporting the effectiveness of the chosen plan. The use of evidence in making the best-individualized therapeutic decision for patient care management is called evidence-based practice (EBP), which is a terminology that was introduced in 1992.6,7 EBP integrates clinical expertise with the best evidence collected from the seven study designs in research: meta-analysis, systemic reviews, randomized controlled trials, cohort studies, case-control studies, case series and case reports, and editorials and expert opinions. The list is ordered according to the importance and the strength of the evidence.8 EBP must go through multiple steps for it to provide a tailored treatment, starting with asking the right clinical questions, navigating through the available resources for the best evidence, critically appraising the chosen evidence, comparing the evidence with a practitioner’s experience, considering the patient’s values and preferences, and lastly, evaluating the outcome of the chosen approach, which might also include changes that were made during the practised decision.9
EBP aims to support all the decisions taken in a patient’s therapy with evidence available in the literature.10 Due to the practical challenges of implementing EBP, improving the supportive information systems is important to support the knowledge and hence the decisions of health care providers.11 A new curriculum that assesses the required skills and improves those skills is needed to fulfil the demands of pharmaceutical care.6 A recent study found that 80% of the included pharmacists supported the claim that EBP can provide improved patient care, while at the same time acknowledging the limited knowledge of EBP as the main barrier to implementing it.12 Even though EBP is presented in curricula across UAE pharmacy schools as a part of the clinical subjects, there are no courses integrated into undergraduate programs that focus completely on EBP.13
Aim of the Study
Overall, studies on EBP evaluation are very limited, considering how important it is to consider EBP and the positive outcomes its use will have on the overall level of pharmaceutical care. The current study aimed to assess the beliefs and implementation of community pharmacists in the UAE regarding EBP and to explore the significant factors that govern their EBPs.
Ethics Approval
Approval for this study was given by the Ajman University Institutional Ethical Review Committee (Reference Number: P-F-H-2019-Nov-28). Moreover, letters of approval were issued to all researchers charged with distributing or collecting questionnaires. The respondents taking part in this study did so voluntarily and received no remuneration of any kind. All respondents were informed of the purpose of the study before data collection began, and all gave their informed consent.
Methods
Study Design and Setting
This study aimed to evaluate the beliefs concerning EBP and the implementation of EBP among community pharmacists in the UAE using a cross-sectional study. Over the six months between December 2017 and June 2018, three trained final-year pharmacy students visited community pharmacies in Dubai and the Northern Emirates. During the pilot survey, all the interviewers were trained properly on the questionnaire and the scientific terminology included within the survey. This training program improved the surveyors’ skills and minimized the errors related to the survey.
Target Population
The study subjects were chosen based on the following inclusion and exclusion criteria. Inclusion criteria: community pharmacists who had three months’ professional experience or more and were registered with one of three regulatory bodies (Ministry of Health, Health Authority Abu Dhabi (HAAD), or Dubai Health Authority). Exclusion criteria: pharmacists who were not registered with the above regulatory bodies or who had less than three months’ experience (i.e., recently joined or still serving their probation period).
Data Collection
Selected community pharmacies across Dubai and the Northern Emirates were visited between 2 December 2017 and 25 June 2018. The researchers explained the purpose of the research to the pharmacists and noted their email addresses. Face-to-face interviews were then carried out and a structured questionnaire was used.
Sample Size Calculation
A review of the literature revealed that no research has yet been carried out evaluating the use of EBP by the target population of this study. However, the prevalence rate is expected to be approximately 35%. The current study set the alpha level at 5%, giving a 95% confidence interval (CI) with the precision set at 5% and thus a maximum width of 10%. Given an assumed non-response rate of approximately 30%, a minimum of 501 respondents were needed. Ultimately, the sample size was set at n = 505.
Sampling Technique
To ensure representativeness, this study used a stratified random sampling technique. In 2010, it was estimated that a total of 2000 community pharmacies are practising across the UAE.14 The contact details and locations of community pharmacies in the areas chosen for study were taken from local business directories and the Yellow Pages.
The stratification in the current study involved the division of the community pharmacies that are practising across the UAE into groups or strata based on the community pharmacies’ locations. Accordingly, three strata were identified, as follows: community pharmacies located in Abu Dubai, community pharmacies located in Dubai, and community pharmacies located in the Northern Emirates.
Once pharmacies had been selected, Excel software was used to record all related data to serve as a sampling frame, reporting the name, type, location, email address, and phone number of each pharmacy. Each pharmacy was given an ID number, after which all the listed pharmacies were subjected to a simple random sample selection process. Pharmacies selected for inclusion were then categorized by type and location.
Research Instrument
The research instrument consisted of a structured questionnaire covering 40 items. The questionnaire was designed based on a literature review15–17 and reviewed by experts in the field to ensure that the content relevance and design were of an acceptable standard. Furthermore, content relevance and appropriateness were approved by four faculty members from the Faculty of Medicine and Clinical Pharmacy at Ajman University. Small changes were made on the advice of the experts consulted. The questionnaire’s quantitative content validity was also tested against Lawshe’s content validity,18 with all items reporting a content validity ratio (CVR) of 0.71. Under Lawshe’s method,18 any items scoring a CVR of ≥0.78 are acceptable; items not meeting this threshold are usually removed from the research instrument. A content validity index (CVI) is then calculated from the mean of all items used in the final research instrument with acceptable CVR values. The questionnaire designed for the current study had a final CVI of 0.879 and therefore passed the threshold.19 A pilot study was then carried out to test the face validity with 10 community pharmacists whose data were excluded from the final analysis. Cronbach’s α value was calculated to analyse the research instrument’s reliability, with a score of 0.73, indicating that internal consistency was acceptable. Figure 1 shows the process used for validating the questionnaire.
 |
Figure 1 Process used for validating the study questionnaire. |
Research Instrument Sections
Respondents were given the choice of questionnaires written in English or Arabic. The questionnaire was divided into three parts, covering
- – Six questions to elicit demographic information, covering age, gender, position held in the pharmacy, whether working full-time or part-time, number of years’ experience, and which university they had graduated from.
- – Sixteen questions designed to assess beliefs concerning EBP. These beliefs were further broken down into four classes, knowledge of EBP, value of EBP, type and availability of resources, and obstacles and time pressures. Respondents were asked to rate their answers to each item on a 5-point Likert scale where 0 = “strongly disagree” and 4 = “strongly agree”.
- – Eighteen questions designed to assess the extent to which EBP has been implemented in practice in the last eight weeks. Respondents were asked to rate the frequency of implementation concerning each item on a 5-point Likert scale, where 0 = “0 times”; 1 = “1–3 times”, 2 = “4–6 times”; 3 = “6–8 times”; and 4 = “>8 times”.
Statistical Analysis
SPSS Version 24 was used to analyse the data collected. Frequencies (stated as percentages) were used to summarize qualitative variables, whereas ± standard deviation (±SD) was used to summarize quantitative variables. EBP beliefs and implementation were assessed using two scores, each of which was calculated by totalling the response codes across all items rated by the respective Likert scales. The scoring range for EBP beliefs was 64–0, with scores at the higher end indicating a higher level of belief in EBP. The scoring range for EBP implementation was 72–0 and, likewise, scores at the higher end indicated a better level of EBP implementation. To test average cross-group differences in quantitative variables, unpaired Student’s t-tests, non-parametric versions, and one-way ANOVA were all applied. Shapiro Wilk tests were carried out to test the normality of the EBP beliefs and EBP implementation scores. The results showed that there were no statistically significant differences from the normal distribution for the EBP beliefs and EBP implementation scores, P = 0.88 and P = 0. 68, respectively. Logistic regression models were used to investigate the association between EBP and other significant factors. Pearson’s correlation was used to examine the association between EBP beliefs and EBP implementation scores. A p-value <0.05 was chosen as the cut-off for statistical significance.
Results
Baseline Characteristics of Community Pharmacies Included in the Study
A total of 505 subjects participated in the study and completed the entire questionnaire. Of those, there were 49.9% (n = 252) aged 20–25 years, 15.6% (n = 79) aged 26–30 years, 18% (n = 91) aged 31–40 years, and 16.4% (n = 83) aged ˃ 40 years. In-charge pharmacists constitute 39.6% of the sample; 56.4% were staff pharmacists, and 4% were assistant pharmacists. Table 1 displays the baseline characteristics of the participants.
 |
Table 1 Demographic and Socioeconomic Features (n = 505) |
Evaluation of EBP Beliefs and Implementation Among Community Pharmacists
On average, participants scored higher in their beliefs score than implementation score. The average beliefs score was 36% (95% CI: [34%, 39%]), compared to an average implementation score of 35% (95% CI: [33%, 37%]).
Table 2 shows the distribution of beliefs and implementation scores according to demographic and socioeconomic status. The table also provides the 95% CI for the estimates along with p-values. Participants with female gender, international/regional graduates, and those with higher positions scored relatively higher in EBP beliefs. However, no significant difference was found in beliefs scores according to age group, years of experience, or percentage of full-time work.
 |
Table 2 Belief and Implementation Scores According to Demographic and Socioeconomic Situation |
Participants with higher positions, more experience, and lower percentages of full-time working and international/regional graduates were more likely to score better in EBP implementation. There was no significant difference in EBP implementation score according to gender or age group. For more details comparing the two scores according to demographic and socioeconomic factors, see Table 2. The results of each of the questions related to EBP beliefs and EBP implementation were analysed using frequency and percentage (Tables 3 and 4).
 |
Table 3 Frequency Table for EBP Beliefs |
 |
Table 4 Frequency Table for EBP Implementation |
Factors Associated with EBP Beliefs and EBP Implementation
Table 5 presents a logistic regression analysis to assess the associated factors of EBP beliefs and EBP implementation. Accordingly, the characteristics of female gender, older age, higher position, more experience, lower percentage of full-time working, and graduating from international/regional universities were correlated with a higher likelihood to believe and implement the concept of EBP. For more details, see Table 5.
 |
Table 5 Logistic Regression Model Applied Separately to Each Demographic and Socioeconomic Variable |
Correlation Between EBP Beliefs and EBP Implementation
There was a statistically significant positive correlation (r) between beliefs towards EBP and implementation of EBP (r = 0.55, p ˂ 0.001). See Figure 2.
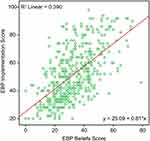 |
Figure 2 Correlation between EBP beliefs and EBP implementation. |
Discussion
The results of this study reveal that age, gender, pharmacist position, years of experience as a pharmacist, percentage of full-time working compared to total experience, and the location of the graduating university are strong determinants of the beliefs and implementation of EBP among community pharmacists. Moreover, this study showed that the characteristics of female gender, younger age, higher position, more experience, lower percentage of full-time working, and graduating from international/regional universities were correlated with a higher likelihood to believe and implement the concept of EBP.
Although the study results show that pharmacists have a positive perception of EBP, practising EBP was executed only to a small degree. Pharmacists who were exposed to EBP and held higher positions, graduated from international or regional universities, and were female scored higher in belief in the value of EBP. Due to the lack or absence of pharmacy EBP-related studies, most of our results are reflected in other healthcare-related professions, including nursing.
Our scale analysis of EBP showed that 36% of the sample believed in the benefits of EBP. When it comes to EBP steps, only 9.7% found them clear, which, in comparison to a similar study conducted on nurses, resulted in a higher percentage of 23.7%. Similar to the previous study, 25.7% of pharmacists included in our study had difficulty in searching and finding the best evidence.20 The main barrier to implementing EBP was the pharmacists’ lack of confidence in their own knowledge, where only 11% indicated an ability to implement EBP in their workplace, which parallels previous studies.21–23 Furthermore, pharmacists scored low in the availability of resources for EBP. A significant positive correlation was found between belief and implementation of EBP, which corresponds to a previous study .15
Despite the slightly lower EBP implementation score, 80% have implemented EBP through navigating and critically appraising clinical research studies. When it came to assessing their own practices, half of the study sample did not evaluate the outcome of changes in practice even once. Hence, pharmacists should be aware of self-critique and not shy away from updating their therapeutic plans to improve patient care, which is a strategy proven effective in a study by Ivers et al.24
In its mission to achieve excellence in the UAE healthcare sector, HAAD holds training for healthcare professionals to ensure valuable contributions to patients’ care that comply with international standards. HAAD extended pharmacists’ role not only to medication counselling but also included other services in the scope of what pharmacists can carry out in the UAE, like adult vaccination and medicine and lifestyle management strategies.25 However, when it comes to the gulf region, patients exhibit more trust in physicians than they do in pharmacists, as many of them do not have a clear understanding of the important role pharmacists have in health management. One study carried out in the UAE stated that pharmacists received only 5–20 inquiries per month from patients consulting the pharmacists for drug-related recommendations, which is equivalent to 0.1–0.66 inquiries per day.26
The literature supports the positive impact pharmaceutical care has on better and more professional pharmacy practice to accomplish the goals of the health care service.27–29 However, a shift in pharmacy practice from merely dispensing medications to providing care supported by evidence requires training pharmacists early and continuing their education throughout their career. To bridge the gap between EBP beliefs and implementation, workshops and group studies should be conducted for pharmacists. Community pharmacists have shown positive impressions of EBP beliefs and implementation.13 To summarize the findings in the current study, pharmacists tend to believe in the importance of EBP implementation, yet they practise it to a much lesser extent.
For that, developing the education system that students of pharmacy receive during their undergraduate studies becomes of high importance, not only to increase their knowledge level but also to encourage commitment in those pharmacists to strive for professionalism and to support the provided patient care with evidence. However, teaching EBP to students might be challenging when there are not enough pharmacists that use EBP in their practice, as shown by our study, because a survey found that mentorship can play a role in facilitating the implementation of EBP among other pharmacists and nurses.30,31 Furthermore, the results of our survey can help in developing educational campaigns that can help to raise the awareness, knowledge, and beliefs of pharmacists towards EBP. They can play a role in setting the platform for which the educational programs can be tailored to enhance the awareness of UAE and even Gulf Cooperation Council pharmacists regarding the proper EBPs, leading to higher health service quality in the region, because knowing the real status and figuring out the gaps is the first step in the improvement process.
There are certain limitations to this study. A self-administered questionnaire was used and this gives a potential for recall bias that could lead to an underestimation of the true figures. Additionally, when study questionnaires were distributed, they were labelled as relating to EBP, so there is a possibility that pharmacists who accepted enrolment in our study have preconceived ideas about EBP. Thus, our study findings are not to be generalized over all the population of pharmacists in the UAE. However, with the fact of the limited literature from UAE on this subject, we believe that this study results would be helpful in providing positive future guidance. Future studies can incorporate similar aspects of the study design in different topics to target a less focused group.
Implications of the Study
Pharmacy colleges should conduct competent programs on the changing role of the pharmacist. The education must enhance the ability of critical thinking and boost problem-solving skills as well as evidence-based decision-making in pharmacotherapy. In this way, students will be trained to establish, transmit, and even apply the newly acquired knowledge based on frontline research. They must collaborate with other health care team members and learn how to improve the quality of life of patients.3 Deeper research is suggested to understand pharmacists’ needs and expectations in a better and deeper way and to develop appropriate strategies to enhance the integration of EBP into their daily real practice. Currently, with the artificial intelligence and informatics revolution, it is recommended that smart systems be used in pharmacy computers. This can help in guiding pharmacists to the appropriate evidence-based approach in every case. Such systems can incorporate smart clinical decision support that enables automatic and even patient-specific mapping together with clinical pathways based on evidence-based guidelines.
Conclusions
A gap was identified between EBP beliefs and EBP implementation. Developing an educational EBP course in the undergraduate pharmacy curriculum, as well as continuous post-graduate education, is of high importance, not only to increase the knowledge level but also to encourage commitment in those pharmacists to strive for professionalism and to support the provided patients’ care with evidence.
Acknowledgments
The authors extend their appreciation to the Researchers Supporting Project number (RSP-2020/119), King Saud University, Riyadh, Saudi Arabia for funding this work. We would like to thank Dr Nasir A. Siddiqui and Mohamed Husham Khattab for their support of the work and to obtain results in a better quality.
Funding
Funded by Researchers Supporting Project number (RSP-2020/119), King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors have no conflicts of interest to declare.
References
1. Albanese NP, Rouse MJ, Schlaifer M. Scope of contemporary pharmacy practice: roles, responsibilities, and functions of pharmacists and pharmacy technicians. J Am Pharm Assoc. 2010;50(2):e35–e69. doi:10.1331/JAPhA.2010.10510
2. World Health Organization. The world health report 2008: primary health care now more than ever. 2008. Available from: http://www.who.int/whr/2008/whr08_en.pdf.
3. Toklu HZ. Rational use of medicine in pharmacy practice. Turk Klin J Pharmacol Spl Top. 2015;3:74–83.
4. Linsley P, Kane R, Barker JH. Evidence-Based Practice for Nurses and Healthcare Professionals. London, UK: SAGE Publications Limited; 2019.
5. Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47:533–543.
6. Wiffen P, Eriksson T, Lu H. Introduction to evidence-based practice in evidence-based pharmacy 2nd edition. Eur J Hosp Pharm. 2013;20:324–327. doi:10.1136/ejhpharm-2013-000415
7. Guyatt G, Evidence-Based Medicine Working Group. Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992;268(17):2420–2425. doi:10.1001/jama.1992.03490170092032
8. Albrecht S. Evidence-based medicine in pharmacy practice. US Pharm. 2009;34:HS14–HS18.
9. Melnyk BM, Fineout-Overholt E. Evidence-Based Practice in Nursing & Healthcare: A Guide to Best Practice.
10. Schindler B, Gointher J, Suter K. Evidence-based pharmacy–assessment of study quality. Med Monatsschr Pharm. 2014;37:413–418.
11. Bates DW, Kuperman GJ, Wang S, et al. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J Am Med Inform Assoc. 2003;10(6):523–530. doi:10.1197/jamia.M1370
12. Abu Farha R, Alefishat E, Suyagh M, Elayeh E, Mayyas A. Evidence-based medicine use in pharmacy practice: a cross-sectional survey. J Eval Clin Pract. 2014;20:786–792. doi:10.1111/jep.12212
13. Abu-Gharbieh E, Khalidi DA, Baig MR, Khan SA. Refining knowledge, attitude and practice of evidence-based medicine (EBM) among pharmacy students for professional challenges. Saudi Pharm J. 2015;23(2):162–166. doi:10.1016/j.jsps.2014.07.006
14. UAE has over 2000 private pharmacies, 4000 professionals. Available from: http://wam.ae/en/details/1395228626943.
15. Stokke K, Olsen NR, Espehaug B, Nortvedt MW. Evidence based practice beliefs and implementation among nurses: a cross-sectional study. BMC Nurs. 2014;13:8. doi:10.1186/1472-6955-13-8
16. Dessie G, Jara D, Alem G, et al. Evidence-based practice and associated factors among health care providers working in public hospitals in Northwest Ethiopia during 2017. Curr Ther Res. 2020;93:100613. doi:10.1016/j.curtheres.2020.100613
17. Burkiewicz JS, Zgarrick DP. Evidence-based practice by pharmacists: utilization and barriers. Ann Pharmacother. 2005;39(7–8):1214–1219. doi:10.1345/aph.1E663
18. Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–575. doi:10.1111/j.1744-6570.1975.tb01393.x
19. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30:459–467. doi:10.1002/nur.20199
20. Al-Quteimat OM, Amer AM. Evidence-based pharmaceutical care: the next chapter in pharmacy practice. Saudi Pharm J. 2016;24(4):447–451. doi:10.1016/j.jsps.2014.07.010
21. Melnyk BM, Fineout-Overholt E, Mays MZ. The evidence-based practice beliefs and implementation scales: psychometric properties of two new instruments. Worldviews Evid Based Nurs. 2008;5:208–216. doi:10.1111/j.1741-6787.2008.00126.x
22. Varnell G, Haas B, Duke G, Hudson K. Effect of an educational intervention on attitudes toward and implementation of evidence-based practice. Worldviews Evid Based Nurs. 2008;5:172–181. doi:10.1111/j.1741-6787.2008.00124.x
23. Mariano KD, Caley LM, Eschberger L, et al. Building evidence-based practice with staff nurses through mentoring. J Neonatal Nurs. 2009;15:81–87. doi:10.1016/j.jnn.2009.01.005
24. Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259.
25. Sadek MM, Elnour AA, Al Kalbani NM, et al. Community pharmacy and the extended community pharmacist practice roles: the UAE experiences. Saudi Pharm J. 2016;24:563–570. doi:10.1016/j.jsps.2015.03.023
26. Hamoudi NM, Shirwaikar AA, Ali HS, Al Ayoubi EI. Pharmaceutical consultation in UAE community pharmacies. Indian J Pharm Sci. 2011;73:404–408. doi:10.4103/0250-474X.95621
27. Chisholm-Burns MA, Kim Lee J, Spivey CA, et al. US pharmacists’ effect as team members on patient care: systematic review and meta-analyses. Med Care. 2010;48:923–933. doi:10.1097/MLR.0b013e3181e57962
28. Weng YH, Kuo KN, Yang CY, Lo HL, Chen C, Chiu YW. Implementation of evidence-based practice across medical, nursing, pharmacological and allied healthcare professionals: a questionnaire survey in nationwide hospital settings. Implement Sci. 2013;8:112. doi:10.1186/1748-5908-8-112
29. Shekelle PG, Wachter RM, Pronovost PJ, et al. Making health care safer II: an updated critical analysis of the evidence for patient safety practices. Evid Rep Technol Assess. 2013;Mar(211):1.
30. Gonzalez-Torrente S, Pericas-Beltran J, Bennasar-Veny M, Adrover-Barcelo R, Morales-Asencio JM, De Pedro-gomez J. Perception of evidence-based practice and the professional environment of primary health care nurses in the Spanish context: a cross-sectional study. BMC Health Serv Res. 2012;12(1):227. doi:10.1186/1472-6963-12-227
31. Polit DF, Beck CT. Nursing Research: Generating and Assessing Evidence for Nursing Practice. Philadelphia, PA: Lippincott Williams & Wilkins; 2008.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
