Back to Journals » Drug Design, Development and Therapy » Volume 9
A pharmacokinetic comparison of two voriconazole formulations and the effect of CYP2C19 polymorphism on their pharmacokinetic profiles
Authors Chung H, Lee H , Han H, An H, Lim KS, Lee Y, Cho J , Yoon SH, Jang I , Yu K
Received 30 December 2014
Accepted for publication 18 February 2015
Published 13 May 2015 Volume 2015:9 Pages 2609—2616
DOI https://doi.org/10.2147/DDDT.S80066
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Shu-Feng Zhou
Hyewon Chung,1,* Howard Lee,1,2,* HyeKyung Han,1 Hyungmi An,1 Kyoung Soo Lim,1,3 YongJin Lee,4 Joo-Youn Cho,1 Seo Hyun Yoon,1 In-Jin Jang,1 Kyung-Sang Yu1
1Department of Clinical Pharmacology and Therapeutics, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Republic of Korea; 2Department of Transdisciplinary Studies, Graduate School of Convergence Science and Technology, Seoul National University, Seoul, Republic of Korea; 3Department of Clinical Pharmacology and Therapeutics, CHA University School of Medicine and CHA Bundang Medical Center, Seongnam, Republic of Korea; 4Medical and Regulatory Affairs Team, Samyang Biopharmaceuticals Corporation, Seoul, Republic of Korea
*These authors contributed equally to this work
Purpose: SYP-1018 is a lyophilized polymeric nanoparticle formulation of voriconazole that is under development for intravenous dosing. This study compared the pharmacokinetic and tolerability profiles of SYP-1018 with those of Vfend®, the marketed formulation of voriconazole. The effect of CYP2C19 polymorphism on the voriconazole pharmacokinetics was also evaluated.
Methods: An open-label, two-treatment, two-period, two-sequence crossover study was conducted in 52 healthy male volunteers, who randomly received a single intravenous infusion of either of the two voriconazole formulations at 200 mg. Blood samples were collected up to 24 hours after drug administration for pharmacokinetic analysis. The plasma concentrations of voriconazole were determined using liquid chromatography with tandem mass spectrometry, and the pharmacokinetic parameters were estimated using a noncompartmental method. CYP2C19 genotype was identified in 51 subjects.
Results: The geometric mean ratio (90% confidence interval) of SYP-1018 to Vfend® was 0.99 (0.93–1.04) for the maximum plasma concentrations (Cmax) and 0.97 (0.92–1.01) for the area under the concentration–time curve (AUC) from dosing to the last quantifiable concentration (AUClast). Nineteen homozygous extensive metabolizers (EMs, *1/*1), 19 intermediate metabolizers (IMs, *1/*2 or *1/*3), and ten poor metabolizers (PMs, *2/*2, *2/*3, or *3/*3) were identified, and the pharmacokinetic comparability between SYP-1018 and Vfend® was also noted when analyzed separately by genotype. The systemic exposure to voriconazole was greatest in the PM group, followed by the IM, and then the EM groups. Furthermore, the intrasubject variability for Cmax and AUClast was greater in IMs and PMs than in EMs. No serious adverse event occurred, and both treatments were well tolerated.
Conclusion: SYP-1018 had comparable pharmacokinetic and tolerability profiles to Vfend® after a single intravenous infusion. CYP2C19 genotype affected not only the pharmacokinetics of voriconazole, but its intrasubject variability. SYP-1018 can be further developed as a clinically effective alternative to Vfend®.
Keywords: voriconazole, pharmacokinetics, pharmacogenetics, CYP2C19
Introduction
Voriconazole is a triazole antifungal agent, indicated for the treatment of invasive aspergillosis, candidiasis, and serious infection caused by Scedosporium apiospermum and Fusarium spp.1 Voriconazole is extensively metabolized in the liver, with only 2% excreted in urine unchanged.1 An in vitro study revealed that CYP2C19 enzyme plays a key role in the N-oxidation of voriconazole, with CYP2C9 and CYP3A4 involved to a lesser extent.2 Furthermore, the genetic polymorphism of CYP2C19 influences the pharmacokinetics of voriconazole. The *2 and *3 alleles are deficient alleles,3,4 whereas the *17 allele, a recently identified allelic variant, is associated with ultra-rapid metabolism of voriconazole.5
Because voriconazole is poorly dissolved in aqueous media, Vfend® (Pfizer Inc, New York, NY, USA), the currently marketed intravenous formulation of voriconazole, contains sulfobutyl ether beta cyclodextrin sodium (SBECD) as a solubilizer. As the clearance (CL) of SBECD is decreased in a linear fashion as renal function is diminished, SBECD is accumulated in renally impaired patients.6 In a preclinical study, repeated doses of intravenous SBECD resulted in dose-dependent histologic changes such as renal tubule vacuolation and pulmonary foam cell foci.7 Although there is some evidence that these histologic changes do not exert toxic clinical effects in humans,8–10 the accumulation of SBECD in patients with impaired renal function may limit the use of intravenous voriconazole in this population.1
SYP-1018 is a novel lyophilized polymeric nanoparticle formulation of voriconazole for intravenous administration developed by Samyang Biopharmaceuticals Corporation (Seoul, Republic of Korea). SYP-1018 is composed of a low molecular weight, biodegradable, amphiphilic diblock copolymer, and methoxy-poly(ethylene glycol)-block– poly(d,l-lactide) (mPEG-PDLLA). Additionally, sodium salt of polylactic acid (d,l-PLACOONa) is used as a solubilizer instead of SBECD. Based on several preclinical studies, drugs containing mPEG-PDLLA appear to be safe.11–13 Furthermore, a polymeric micelle formulation of paclitaxel with mPEG-PDLLA (Genexol-PM®) was approved in Korea in 2006, and the clinical data showed that the polymeric micelle formulation was safe and well tolerated.14–16
Based on this understanding, the present study compared the pharmacokinetic and tolerability profiles of SYP-1018 with those of Vfend® after a single intravenous administration in healthy subjects. Furthermore, the effect of CYP2C19 polymorphism on the pharmacokinetics and bioequivalence of the two formulations of voriconazole was evaluated.
Materials and methods
Subjects and study design
A randomized, open-label, two-treatment, two-period, two-sequence, crossover study was performed with a washout period of 7 days. In each period, subjects randomly received a single intravenous dose of SYP-1018 (voriconazole-loaded polymeric nanoparticle) or Vfend®, a reference voriconazole formulation currently available in the market. After written informed consent was obtained, healthy male volunteers of 20–45 years underwent screening, which included medical history, physical examination, laboratory tests (hematology, blood chemistry, coagulation, and urinalysis), 12-lead electrocardiogram (ECG), and vital signs. Subjects were excluded if their alanine aminotransferase (ALT) or aspartate aminotransferase (AST) exceeded 1.25 times the upper limit of normal.
Eligible subjects were admitted to the Clinical Trials Center at Seoul National University Hospital (SNUH), Seoul, Korea, a day before study drug administration in each period. On the 1st day in each period, subjects received SYP-1018 or Vfend® at 200 mg intravenously for 1.5 hours according to their randomized sequence. Serial blood samples of 4 mL for pharmacokinetic analysis were taken at 0 (ie, pre-dose), 0.25, 0.5, 0.75, 1, 1.5, 2, 3, 4, 6, 8, 12, and 24 hours post dose. Additionally, 4 mL of blood was collected for genotyping (period 1 only). Physical examination, vital signs, laboratory tests, and 12-lead ECGs were conducted at the study protocol-specified times. Adverse events were collected during the entire study period.
This study was conducted in compliance with the declaration of Helsinki, Good Clinical Practices, and other regulatory guidelines (ClinicalTrials.gov: NCT01657201). The study protocol and informed consent form were approved by the institutional review board at SNUH.
Determination of voriconazole plasma concentrations
Blood samples were centrifuged at 2,000× g for 10 minutes and the separated plasma were stored below −70°C until voriconazole concentration was determined using high performance liquid chromatography (1260 series; Agilent Technologies, Santa Clara, CA, USA) with mass spectrometer (API4000 QTRAP; SCIEX, Framingham, MA, USA). Voriconazole-d3 (Santa Cruz Biotechnology Inc, Dallas, TX, USA) was used as an internal standard, and the sample was protein precipitated with acetonitrile. Kinetex 2.6 μm C18, 100×2.10 mm (Phenomenex, Torrance, CA, USA) was used as the analytical column, and the mobile phase consisted of 0.1% formic acid in 10 mM ammonium formate and 100% acetonitrile. The flow rate was 0.3 mL/min. The lower limit of quantification (LLOQ) was 25 ng/mL, and the calibration range was 25 ng/mL–4,000 ng/mL. The intrabatch and interbatch coefficient of variation (CV) was less than 2.911% and 5.609%, respectively. Likewise, the intrabatch and interbatch accuracy ranged between 91.38% and 105.1%, and 87.83% and 97.17%, respectively.
Pharmacokinetic analysis
Pharmacokinetic parameters were calculated using a noncompartmental method implemented in Phoenix® WinNonlin® 6.3 (Certara, St Louis, MO, USA). Maximum plasma concentration (Cmax) and time to reach Cmax (Tmax) were determined directly from the observed individual time–concentration profiles. Terminal elimination half-life (t1/2) was calculated as the natural logarithm of 2 divided by λz, which is the terminal elimination rate constant estimated in the linear decline portion of the natural logarithmic transformed individual plasma concentrations. Area under the concentration–time curve (AUC) from dosing to the last quantifiable concentration (AUClast) was calculated using the linear-up/log-down trapezoidal method, and AUC from dosing to infinity (AUCinf) was calculated as the sum of AUClast and Clast/λz, where Clast was the last measurable concentration. CL was also derived as the administered dose divided by AUCinf.
Genotyping
Various allelic variants for CYP2C19, such as the *2 (681G>A, rs4244285, assay ID: C_25986767_70), *3 (636G>A, rs4986893, assay ID: C_27861809_10), and *17 (-806C>T, rs12248560, assay ID: C_469857_10) alleles were genotyped using the TaqMan allelic discrimination assays on an ABI Prism 7500 Sequence Detection System (Thermo Fisher Scientific). Based on the genotype analysis, subjects were identified as extensive metabolizers (EMs) for *1/*1, intermediate metabolizers (IMs) for *1/*2 and *1/*3, or poor metabolizers (PMs) for *2/*2, *2/*3, and *3/*3. Subjects with allelic variant *17 were not classified into specific phenotype.
Statistical analysis
It was estimated that enrolling 52 subjects would yield an 80% power that the 90% confidence interval (CI) of the geometric mean ratio (GMR) for the pharmacokinetic parameters between the two treatments, a CI that falls in the range of (0.8–1.25) at a significance level of 0.05, based on an intrasubject CV of 35% obtained from a previous study in a Korean population (Clinicaltrials.gov, NCT01080651). The demographic characteristics according to the sequence of administered study drug were compared using the Student’s t-test.
The GMR and its 90% CI of SYP-1018 to Vfend® was derived for Cmax, AUClast, and AUCinf using a linear mixed model, where period, sequence, treatment, and CYP2C19 genotype were fixed effects, and subject nested in sequence was random effect. The interaction term between treatment and CYP2C19 genotype was also entered into the model when analyzed separately for CYP2C19 genotype. The pharmacokinetics of SYP-1018 and Vfend® were considered comparable if the 90% CI fell entirely within the conventional bioequivalence range of 0.80–1.25 for both Cmax and AUClast.
The number of subjects with adverse events and frequency of adverse events were compared between treatments using the chi-square test. All the statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA), and P-values ≤0.05 were regarded as statistically significant. Using the intraindividual variability by genotypes, the number of subjects required to meet the conventional bioequivalence criteria was calculated based on a two one-sided tests procedure.17
Results
Subjects and genotyping
This study enrolled 59 subjects, six of whom were dropped prior to drug administration in period 1 due to withdrawal of consent (N=2), pre-treatment events (N=3, two chest discomforts, one eye swelling), and a no-show (N=1). The remaining 53 subjects received at least one study drug, with 52 subjects completing the study. One subject was dropped because of an adverse event that had occurred in period 1, after administration of Vfend®. Age, height, and body weight did not significantly differ between the two sequences. Of the 52 subjects who completed the study, 51 subjects were genotyped: EM (N=19), IM (N=19), PM (N=10), and unclassified (N=3), the latter of which included *1/*17 (N=1) and *2/*17 (N=2). The demographic characteristics of the 52 subjects who completed the study are summarized in Table 1, and there were no differences between the two sequences of study drug administration.
Pharmacokinetics of voriconazole
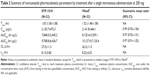
The pharmacokinetic parameters of voriconazole were similar between SYP-1018 and Vfend®, which resulted in the 90% CI for the GMR of SYP-1018 to Vfend® falling within the conventional bioequivalence range of 0.8–1.25 for both Cmax and AUClast (Table 2). The pharmacokinetic comparability between SYP-1018 and Vfend® was also seen when analyzed separately by CYP2C19 genotype, except for Cmax in the PM group, for which the upper bound of the 90% CI was still very close to 1.25 (ie, 1.26, Table 3). Furthermore, the mean plasma concentration–time profiles of the two formulations overlapped almost entirely when compared to each other (Figure 1).
The systemic exposure to voriconazole and its peak as assessed by AUClast and Cmax, respectively, were greatest in the PM group, followed by the IM group, with the EM group having the smallest values (Table 3). For example, the AUClast of both SYP-1018 and Vfend® (GMR and 90% CI) in the PM and IM groups were 2.35 (1.98–2.78) and 1.27 (1.10–1.46) fold greater, respectively, than that in the EM group. The AUClast and AUCinf in the subject with *1/*17 allelic variant were close to those in the EM group (Table 3). On the other hand, subjects with *2/*17 had comparable mean AUClast and AUCinf values to those in the IM group (Table 3).
The intrasubject CV for Cmax in the PM and IM groups was 44% and 22% larger, respectively, than that in the EM group (Table 4, Figure 2). Likewise, the intrasubject CV for AUClast in the PM and IM groups was 71% and 135% larger, respectively, than that in the EM group (Table 4, Figure 2). Consequently, the number of subjects required to meet the conventional bioequivalence criteria between SYP-1018 and Vfend® (ie, two-sided 90% CI for the GMR of SYP-1018 to Vfend® falling entirely within the range of [0.8-1.25]) with an 80% power at a significance level of 0.05 in a 2×2 crossover study was 80% and 40% greater in the PM and IM groups, respectively, for Cmax, and 33% and 100% greater, respectively, for AUClast than in the EM group (Table 4).
Tolerability
There was no significant difference in the number of drug-related adverse events between the two treatments (five and nine cases after SYP-1018 and Vfend®, respectively, P=0.424, chi-square test). Likewise, the number of subjects with at least one drug-related adverse event were five and eight cases for SYP-1018 and Vfend®, respectively, which was not significantly different, either (P=0.555, chi-square test). One subject was dropped after the administration of Vfend® in period 1 because ALT was elevated to 2.7 times the upper limit of normal at 7 days post-dose.
All of the adverse events were mild except for one subject, who presented moderate intensity of multiple musculoskeletal pain accompanying erythema, heating sense, and pruritus after infusion of SYP-1018 in period 2. This case, and the other adverse events, however, resolved spontaneously without any medical intervention. Likewise, no clinically significant abnormality was noted in laboratory tests, 12-lead ECGs, vital signs, or physical examination throughout the entire study period.
Discussion
This study demonstrated that the pharmacokinetic and tolerability profiles of SYP-1018 were comparable to those of Vfend® after a single intravenous administration in healthy subjects. The concentration–time profiles of the two formulations matched almost entirely (Figure 1), and the GMR and its 90% CIs for Cmax and AUClast satisfied the conventional regulatory criteria of bioequivalence (Table 2).The pharmacokinetic comparability for voriconazole between SYP-1018 and Vfend® was also noted even when analyzed separately by different CYP2C19 genotype (Table 3), except for Cmax in the PM group, which might have been due to the small sample size (N=10) relative to its large intrasubject CV of 20.8% (Table 4). Furthermore, both formulations were well tolerated without any serious adverse events. There were no newly reported adverse events in the present study, and the frequency of drug-related adverse events was not significantly different between the two formulations.
We found that CYP2C19 polymorphism influenced the pharmacokinetics of voriconazole in a similar way as previously reported including Korean, Caucasian, and Chinese subjects,3,18,19 ie, the systemic exposure to voriconazole was greatest in the PM group, followed by the IM, and then the EM groups (Table 3). Unlike the *2 and *3 alleles of CYP2C19, which have been known to be associated with nonfunctional poor metabolism, the classification of the *17 allele is still controversial. For example, subjects with *1/*17 can be regarded as ultra-extensive metabolizers, whereas those with *2/*17 are difficult to classify into any phenotype, because the *17 allele could be in cis with either the wild type or deficiency allele.20 Weiss et al reported the pharmacokinetic profiles of voriconazole in those with *2/*17 allelic variants were perfectly matched with those with *1/*17.4 In contrast, the pharmacokinetic parameters in those with *2/*17 in the present study were more or less close to those in the IM group (Table 3, Figure 2). Because only a limited number of subjects were with *2/*17 in the present study (N=2), however, no firm conclusion can be drawn about the effect of the *17 allele on the pharmacokinetics of voriconazole yet, and further studies are warranted.
Besides CYP2C19 *2 and *3, other alleles such as *4 and *8 have also been associated with poor metabolism. However, their allelic frequency is very low compared to *2 and *3 alleles in variety of ethnicity.20 Furthermore, a complete concordance between phenotype and genotype has been reported previously when using only the *2 and *3 alleles in the Oriental population.21 Therefore, although not tested in the present study, those minor alleles including *4 and *8 would unlikely have affected our results.
Voriconazole has highly variable pharmacokinetics, for which CYP2C19 is a major contributing factor.4 In the present study, not only the extent of exposure to voriconazole, but also intrasubject variability was different among CYP2C19 genotypes. For example, intrasubject CV was greater in the PM and IM groups than in the EM group, resulting in a greater number of subjects required to meet the conventional bioequivalence criteria at the same power and significance level (Table 4). Greater intrasubject variability in the CYP3A5 PM group than in the EM group was reported for tacrolimus.22 In contrast, subjects with no active genes of CYP2D6 showed less intrasubject variability for mirtazapine.23 Because the relative frequency of CYP2C19 genotypes can be different among not only various ethnic groups, but also different study populations at hand, information on the composition of CYP2C19 polymorphism and the intrasubject variability by genotype in the study population could be of help in designing a future comparative pharmacokinetic study of voriconazole.
Although we could not conclude if the comparable pharmacokinetic profile for voriconazole between SYP-1018 and Vfend® will be maintained after repeated administration, it is very likely so given that the elimination phase pharmacokinetic parameters for voriconazole at steady state are not different from elimination phase pharmacokinetic parameters after a single dose.24 Furthermore, it is well known that plasma concentration of voriconazole is closely associated with clinical outcomes.25,26 Taken together, SYP-1018 is expected to show a similar efficacy profile to that of Vfend® after repeated administration in patients with fungal infections, and further studies may be warranted in various populations (eg, women, elderly, children, etc). Therefore, SYP-1018 can be further developed as an effective alternative to Vfend®, particularly for patients with decreased renal function.
Conclusion
In conclusion, the pharmacokinetic and tolerability profiles of SYP-1018 were comparable to those of Vfend® after a single intravenous infusion. CYP2C19 genotype affected not only the pharmacokinetics of voriconazole, but also affected its intrasubject variability. SYP-1018 can be further developed as a clinically effective alternative to Vfend®, particularly in patients with renal impairment.
Disclosure
This study was sponsored by Samyang Biopharmaceuticals Corporation (Seoul, Republic of Korea). YongJin Lee is an employee of Samyang Biopharmaceuticals Corporation. Otherwise, the authors declare no conflicts of interest in this work.
References
Vfend® (voriconazole) [package insert]. New York, NY: Pfizer Inc; 2014. Available from: http://labeling.pfizer.com/ShowLabeling.aspx?id=618. Accessed April 30, 2014. | ||
Hyland R, Jones BC, Smith DA. Identification of the cytochrome P450 enzymes involved in the N-oxidation of voriconazole. Drug Metab Dispos. 2003;31(5):540–547. | ||
Lee S, Kim BH, Nam WS, et al. Effect of CYP2C19 polymorphism on the pharmacokinetics of voriconazole after single and multiple doses in healthy volunteers. J Clin Pharmacol. 2012;52(2):195–203. | ||
Weiss J, Ten Hoevel MM, Burhenne J, et al. CYP2C19 genotype is a major factor contributing to the highly variable pharmacokinetics of voriconazole. J Clin Pharmacol. 2009;49(2):196–204. | ||
Wang G, Lei HP, Li Z, et al. The CYP2C19 ultra-rapid metabolizer genotype influences the pharmacokinetics of voriconazole in healthy male volunteers. Eur J Clin Pharmacol. 2009;65(3):281–285. | ||
von Mach MA, Burhenne J, Weilemann LS. Accumulation of the solvent vehicle sulphobutylether beta cyclodextrin sodium in critically ill patients treated with intravenous voriconazole under renal replacement therapy. BMC Clin Pharmacol. 2006;6:6. | ||
Luke DR, Tomaszewski K, Damle B, Schlamm HT. Review of the basic and clinical pharmacology of sulfobutylether-beta-cyclodextrin (SBECD). J Pharm Sci. 2010;99(8):3291–3301. | ||
Lilly CM, Welch VL, Mayer T, Ranauro P, Meisner J, Luke DR. Evaluation of intravenous voriconazole in patients with compromised renal function. BMC Infect Dis. 2013;13:14. | ||
Neofytos D, Lombardi LR, Shields RK, et al. Administration of voriconazole in patients with renal dysfunction. Clin Infect Dis. 2012;54(7):913–921. | ||
Abel S, Allan R, Gandelman K, Tomaszewski K, Webb DJ, Wood ND. Pharmacokinetics, safety and tolerance of voriconazole in renally impaired subjects: two prospective, multicentre, open-label, parallel-group volunteer studies. Clin Drug Investig. 2008;28(7):409–420. | ||
Shi J, Zhang J, Shen Y, et al. Arginine-stabilized mPEG-PDLLA (50/50) polymeric micelles of docetaxel by electrostatic mechanism for tumor-targeted delivery. Drug Deliv. 2015;22(2):168–181. | ||
Kim SC, Kim DW, Shim YH, et al. In vivo evaluation of polymeric micellar paclitaxel formulation: toxicity and efficacy. J Control Release. 2001;72(1–3):191–202. | ||
Lee SW, Yun MH, Jeong SW, et al. Development of docetaxel-loaded intravenous formulation, Nanoxel-PM™ using polymer-based delivery system. J Control Release. 2011;155(2):262–271. | ||
Lee JL, Ahn JH, Park SH, et al. Phase II study of a cremophor-free, polymeric micelle formulation of paclitaxel for patients with advanced urothelial cancer previously treated with gemcitabine and platinum. Invest New Drugs. 2012;30(5):1984–1990. | ||
Kim DW, Kim SY, Kim HK, et al. Multicenter phase II trial of Genexol-PM, a novel Cremophor-free, polymeric micelle formulation of paclitaxel, with cisplatin in patients with advanced non-small-cell lung cancer. Ann Oncol. 2007;18(12):2009–2014. | ||
Lee KS, Chung HC, Im SA, et al. Multicenter phase II trial of Genexol-PM, a Cremophor-free, polymeric micelle formulation of paclitaxel, in patients with metastatic breast cancer. Breast Cancer Res Treat. 2008;108(2):241–250. | ||
Liu JP, Chow SC. Sample size determination for the two one-sided tests procedure in bioequivalence. J Pharmacokinet Biopharm. 1992;20(1):101–104. | ||
Shi HY, Yan J, Zhu WH, et al. Effects of erythromycin on voriconazole pharmacokinetics and association with CYP2C19 polymorphism. Eur J Clin Pharmacol. 2010;66(11):1131–1136. | ||
Mikus G, Schöwel V, Drzewinska M, et al. Potent cytochrome P450 2C19 genotype-related interaction between voriconazole and the cytochrome P450 3A4 inhibitor ritonavir. Clin Pharmacol Ther. 2006;80(2):126–135. | ||
Strom CM, Goos D, Crossley B, et al. Testing for variants in CYP2C19: population frequencies and testing experience in a clinical laboratory. Genet Med. 2012;14(1):95–100. | ||
Goldstein JA, Ishizaki T, Chiba K, et al. Frequencies of the defective CYP2C19 alleles responsible for the mephenytoin poor metabolizer phenotype in various Oriental, Caucasian, Saudi Arabian and American black populations. Pharmacogenetics. 1997;7(1):59–64. | ||
Chung JY, Lee YJ, Jang SB, Lim LA, Park MS, Kim KH. CYP3A5*3 genotype associated with intrasubject pharmacokinetic variation toward tacrolimus in bioequivalence study. Ther Drug Monit. 2010;32(1):67–72. | ||
González-Vacarezza N, Abad-Santos F, Carcas-Sansuan A, et al. Use of pharmacogenetics in bioequivalence studies to reduce sample size: an example with mirtazapine and CYP2D6. Pharmacogenomics J. Oct 2013;13(5):452–455. | ||
Purkins L, Wood N, Greenhalgh K, Eve MD, Oliver SD, Nichols D. The pharmacokinetics and safety of intravenous voriconazole – a novel wide-spectrum antifungal agent. Br J Clin Pharmacol. 2003;56(Suppl 1):2–9. | ||
Pascual A, Calandra T, Bolay S, Buclin T, Bille J, Marchetti O. Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin Infect Dis. 2008;46(2):201–211. | ||
Trifilio S, Singhal S, Williams S, et al. Breakthrough fungal infections after allogeneic hematopoietic stem cell transplantation in patients on prophylactic voriconazole. Bone Marrow Transplant. 2007;40(5):451–456. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.