Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
A meta-analysis of lipid peroxidation markers in major depression
Authors Mazereeuw G, Herrmann N , Andreazza A, Khan M, Lanctôt KL
Received 5 June 2015
Accepted for publication 24 July 2015
Published 29 September 2015 Volume 2015:11 Pages 2479—2491
DOI https://doi.org/10.2147/NDT.S89922
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Graham Mazereeuw,1,2 Nathan Herrmann,1,3 Ana C Andreazza,2–4 Maisha M Khan,1 Krista L Lanctôt1–3
1Hurvitz Brain Sciences Program, Sunnybrook Research Institute, Sunnybrook Health Sciences Centre, Toronto, ON, Canada; 2Department of Pharmacology and Toxicology, University of Toronto, Toronto, ON, Canada; 3Department of Psychiatry, University of Toronto, 4Centre for Addiction and Mental Health, Toronto, ON, Canada
Background: Major depressive disorder (MDD) may be associated with oxidative damage to lipids, which can potentially affect mood-regulating pathways. This meta-analysis summarizes current knowledge regarding lipid peroxidation markers in clinical samples of MDD and the effects of antidepressant pharmacotherapy on those markers.
Methods: MEDLINE, EMBASE, CINAHL, PsycINFO, and Cochrane Collaboration were searched for original, peer-reviewed articles measuring markers of lipid peroxidation in patients with MDD and nondepressed healthy controls up to April 2015. Standardized mean differences (SMDs) were generated from random effects models summarizing mean (± standard deviations) concentrations of selected markers.
Results: Lipid peroxidation was greater in MDD than in controls (studies =17, N=857 MDD/782 control, SMD =0.83 [0.56–1.09], z=6.11, P<0.01, I2=84.0%) and was correlated with greater depressive symptom severity (B=0.05, df=8, P<0.01). Antidepressant treatment was associated with a reduction in lipid peroxidation in MDD patients (studies=5, N=222, SMD=0.71 [0.40–0.97], P<0.01; I2=42.5%).
Limitations: Lipid peroxidation markers were sampled from peripheral blood, included studies comparing MDD to controls were all cross-sectional, and only five antidepressant treatment studies were eligible for inclusion.
Conclusion: Increased lipid peroxidation was associated with MDD and may be normalized by antidepressants. Continued investigation of lipid peroxidation in MDD is warranted.
Keywords: antidepressant treatment, biomarker, malondialdehyde, depressive episode, reactive oxygen species, lipid peroxidation
Introduction
Major depressive disorder (MDD) is a serious psychiatric illness with a lifetime prevalence of 12% in the adult population.1 MDD confers substantial reductions in psychological and physical well-being,2 and is associated with a significant socioeconomic burden.3 Treatment of MDD with selective serotonin or norepinephrine reuptake inhibitors or other currently available antidepressants is modestly effective (response rates of 26%–63%);4,5 however, relapse frequently occurs and several antidepressant trials may be needed in order for symptom remission to be achieved.4,5 As such, the elucidation of novel therapeutic targets for MDD is an active area of research (reviewed in Sibille and French6).
Oxidative stress is emerging as a relevant mechanism as it is related to the overarching inflammatory/immune activations associated with MDD.7–9 Oxidative stress begins when the production of reactive oxygen species is not sufficiently balanced by antioxidant species, which neutralize them (reviewed in Andreazza10). For example, the generation of a superoxide anion, a powerful reactive oxygen species, is typically neutralized by the antioxidant enzyme superoxide dismutase to protect the cell from oxidative stress; however, excessive concentrations of superoxide may overwhelm superoxide dismutase and form a hydroxyl radical after reacting with water.10
Lipid peroxidation begins with the addition of a hydroxyl radical to an unsaturated lipid, generating a lipid hydroperoxide (early-stage lipid peroxidation).11 Lipid hydroperoxides may be neutralized by lipid-specific antioxidants such as glutathione peroxidase or vitamin E, or general antioxidants such as vitamin C, glutathione, vitamin A, and other carotenoids. If lipid hydroperoxides overwhelm the antioxidant system, they may continue reacting to form late-stage lipid peroxidation products such as 4-hydroxynonenal, malondialdehyde, or 8-isoprostane.11 Peroxidated lipids may not only exacerbate oxidative stress directly, they may also influence a shift in lipid signaling, monoamine regulation, inflammatory pathways, and autoimmune activity through the formation of immunogenic neoepitopes, which may collectively contribute to the pathophysiology of MDD.9,12–14
The roles of lipid peroxidation markers in the etiology of clinically-defined MDD uncomplicated by comorbid illnesses, as well as the effects of antidepressant pharmacotherapy on those markers, have yet to be quantitatively summarized at the group or individual marker level, which may help to clarify mechanisms. This meta-analysis summarizes the differences in lipid peroxidation markers between MDD patients and healthy controls, as well as the effects of antidepressant pharmacotherapy on those markers in patients with MDD.
Methods
Data sources
Methodology was consistent with PRISMA guidelines.15 MEDLINE, EMBASE, PsycINFO, Cochrane Collaboration, AMED, and CINAHL were searched up to April 2015. The search strategy is detailed in Table S1. Briefly, lipid peroxidation markers (malondialdehyde, lipid hydroperoxides, 4-hydroxynonenal, isoprostanes, etc) were itemized and searched for in the context of depression. Data that could not be retrieved from reports were sought through contact with study authors. Reference lists of retrieved studies were searched for additional reports.
Study selection
The literature search provided a comprehensive list of studies, which collectively enabled the meta-analysis of lipid peroxidation markers in MDD and the effects of antidepressant pharmacotherapies on those markers in MDD patients. Inclusion criteria for this meta-analysis were: 1) studies reporting quantifiable measurements of lipid peroxidation in plasma, serum, or cell membrane (details in Table S1); 2) the inclusion of a depressed group as diagnosed by recognized criteria such as the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV or V)16,17 or the International Classification of Diseases 10 Classification of Mental and Behavioural Disorders;18 and 3) the inclusion of a medically and psychiatrically healthy control group. Studies comparing lipid peroxidation in depressed patients and healthy controls cross-sectionally as well as studies comparing those markers at the baseline visit of a longitudinal interventional study were captured by our search strategy and were included in this meta-analysis. Studies were excluded if they did not confirm the presence of a unipolar depressive episode using standardized criteria (as mentioned earlier), and/or if they reported on depression secondary to another psychiatric disorder (eg, depressive symptoms in those with bipolar disorder or schizophrenia), neurological disorder (eg, depressive symptoms in those with dementia, Parkinson’s disease, stroke, etc), or medical disorder (eg, depressive symptoms in those with coronary artery disease, diabetes mellitus, etc). Studies were not limited by language.
Data extraction
Two independent reviewers examined each retrieved article for eligibility. Results were compared between reviewers and disagreements were settled by consensus with a third reviewer. The methods and results sections of each included article were analyzed: plasma, serum, or cell-membrane concentrations of lipid peroxidation markers (mean ± standard deviation) for both the depressed and healthy control groups were extracted as well as participant characteristics (mean age, percentage male, depression severity, smoking, and antidepressant use), tissue sampled (plasma, serum, or cell), and marker species (malondialdehyde, lipid hydroperoxides, 4-hydroxynonenal, isoprostanes, etc).
In a subanalysis of relevant included studies, the effects of antidepressant pharmacotherapy on lipid peroxidation markers over time were explored. Studies included in the subanalysis were required to provide pre- and post-treatment concentrations of a lipid peroxidation marker. Study characteristics (antidepressant class, specific medication, duration of treatment, etc) and depressive symptom severity scores pre- and post-treatment were also collected. Markers measured by two or more studies were meta-analyzed.
Statistical analyses
Standardized mean differences (SMDs) and 95% confidence intervals were calculated using random effects models.19 Random effects models adjust for variable underlying effects in estimates of uncertainty, including both within- and between-studies variance, and are preferable if significant heterogeneity is expected and/or observed across studies. If concentrations of oxidative stress markers were reported from more than one source (plasma, serum, and/or cell membrane), the mean and standard deviations for each sample were pooled20 and the resultant pooled mean and standard deviation were included as that study’s contribution to the meta-analysis of that particular marker.
Heterogeneity across included studies was summarized by a Q statistic, calculated in chi-square analysis. A significant Q statistic indicates heterogeneity in the characteristics of the included studies. An inconsistency statistic, assessed using an I2 index,21 determined the impact of heterogeneity on meta-analytic findings. To identify potential sources of heterogeneity, subgroup analyses were carried out based on participant characteristics, sample source, and intervention characteristics for those studies with antidepressant interventions. Study level inverse variance weighted metaregression analyses were conducted to investigate relationships between SMDs and population characteristics (eg, mean age, percentage male, depressive symptom severity). Regression data were summarized using unstandardized regression coefficients (B) and 95% confidence intervals.
Risk of publication bias was assessed visually using funnel plots and quantitatively using Egger’s test.22,23 Study quality items were assessed using items selected from the Newcastle–Ottawa Scale and the Cochrane Collaboration’s risk of bias assessment tool to address key methodological criteria relevant to included studies. Studies not meeting the majority of reporting quality items were excluded from analyses in a subanalysis to identify potential sources of heterogeneity. SMDs, heterogeneity, metaregression, and bias were determined using Stata (Release 10.1; StataCorp LP, College Station, TX, USA).
Results
Literature search results
The search strategy was not limited by language and identified 1,523 unique articles of which 17 met the inclusion criteria (Figure S1). Study designs and participant characteristics of the meta-analyzed studies are summarized in Table 1.
All included studies provided accessible means and standard deviations for at least one lipid peroxidation marker in both depressed and nondepressed groups. In keeping with the inclusion and exclusion criteria of this meta-analysis, none of the included studies consisted of depressed patients with psychiatric, neurological, or medical comorbidities and controls were all free of those illnesses as well.
In the meta-analysis of depressed patients compared to controls, the majority of studies measured malondialdehyde (14 studies), one measured 4-hydroxynonenal, one measured oxidized low-density lipoprotein, and two measured F2-isoprostane. Lipid peroxidation markers were most often measured from plasma (nine studies), although five studies measured from serum, two measured from cell membranes, and two measured from multiple tissues and concentrations were therefore pooled (mixed). Across included studies, six studies included antidepressant-naive patients, four studies included patients using antidepressant medications at the time of study, two studies included patients with prior exposure to antidepressant medications but who had completed a washout phase (durations of 4 weeks and 12 weeks), and there were six studies for which prior exposure to antidepressant medication could not be clearly determined.
Of the five studies, which reported an antidepressant intervention component, all measured malondialdehyde and four-sampled plasma. Selective serotonin reuptake inhibitors were the most common intervention (three studies), although two studies used several classes of antidepressant as prescribed for individual patient needs.
MDD vs healthy controls
Lipid peroxidation data from 17 studies24–40 (one with two depressed and two control groups36) were meta-analyzed. Depressed patients demonstrated significantly greater concentrations of lipid peroxidation markers than healthy controls; however, significant heterogeneity was detected (Figure 1). A funnel plot and Egger’s test also indicated a potential risk of publication bias (t=4.08, P<0.01). However, the observed elevation in the concentrations of lipid peroxidation markers in depressed patients remained significant after adjusting for potential publication bias using a trim and fill procedure (adjusted SMD =0.49 [0.22–0.77], z=3.51, P<0.01).
Potential sources of heterogeneity were investigated. Subdividing groups of studies by the lipid peroxidation marker species, tissue sampled, and prior exposure to antidepressant medications did not account for the heterogeneity across all studies, although heterogeneity was eliminated in certain subgroups (Table 2). No associations were observed between SMD and age (B=−0.00, df=16, P=0.99), percentage male (B=0.01, df=16, P=0.52), or percentage smokers (B=−0.00, df=9, P=0.76). However, as nine of the 16 included studies reported depressive symptom severity using the same scale (the Hamilton Depression Rating Scale [HAM-D]41), we could detect a significant association between greater depressive symptom severity (HAM-D score) in the depressed group and larger study SMDs (B=0.05, df=8, P<0.01), such that an increase in lipid peroxidation by 1 standard deviation corresponded with a 20-point increase in HAM-D score (Figure 2). This relationship appeared to account for the majority of between-studies heterogeneity (adjusted R2=1.00, residual I2=36.7%). Despite the heterogeneity, significant differences in concentrations of lipid peroxidation markers between depressed patients and controls were observed in all subgroups.
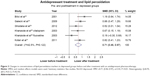
Effects of antidepressants
A subset of five studies25,28–31 (one study with two treatment groups30) investigated the effect of antidepressant pharmacotherapy on markers of lipid peroxidation in depressed patients. Lipid peroxidation was significantly reduced after antidepressant treatment in depressed patients and significant heterogeneity was not detected (Figure 3). No potential publication bias was indicated (t=−0.27, P=0.80). No differences in treatment effects were observed between antidepressant classes or tissue sampled (Table 2). No associations between SMD and age (B=−0.01, df=5, P=0.79), percentage male (B=−0.01, df=4, P=0.44), baseline depression severity (B=0.22, df=4, P=0.59), or duration of treatment (B=0.01, df=5, P=0.73) were observed. Changes in lipid peroxidation marker concentrations were not correlated with changes in depressive symptom severity due to antidepressant treatment (B=−0.02, df=4, P=0.47).
Assessment of study reporting quality
Fifteen of the 17 meta-analyzed studies satisfied the majority of reporting quality items (Table S2). Of the studies that included a treatment component, four of the five satisfied the majority of reporting quality items (Table S2). Repeating the analyses in a subgroup of studies judged to be of higher reporting quality did not change the SMDs or heterogeneity in the comparison of lipid peroxidation markers between those with MDD and controls (SMD =0.99 [0.78–1.20], df=12, z=9.24, P<0.01, I2=59.9%) or in the comparison of lipid peroxidation markers before and after antidepressant treatment in those with MDD (SMD =0.75 [0.45–1.05], df=5, z=4.90, P<0.01, I2=50.4%).
Discussion
This meta-analysis suggests an association between increased lipid peroxidation in peripheral blood samples and the presence of MDD. This finding is consistent with a general increase in oxidative stress in those with depressive symptoms7,42 and provides evidence for a specific elevation of lipid peroxidation. However, inferences from our results differ from those of previous meta-analyses because of our particular study design. While previous meta-analyses included a wide-range of studies measuring depression using both standardized and nonstandardized scales, and/or included patient populations with comorbid psychiatric or medical illnesses, conditions that by themselves have all been implicated with increased oxidative stress,43–46 our meta-analysis focused exclusively on clinically-defined unipolar depression as a primary disorder, measured using standardized criteria, rather than in conjunction with a comorbid illness. As such, the results of this meta-analysis pertain specifically to the potential role of lipid peroxidation markers in a more homogeneous set of patients with depression. This enables us to make inferences regarding lipid peroxidation as part of depression pathophysiology more directly and builds on the positive findings of previous meta-analyses.
Beyond a collective increase in lipid peroxidation markers among patients with major depression, this study identified a linear relationship between greater depressive symptom severity and a greater degree of lipid peroxidation in patients with MDD, which accounted for a large portion of the variability across studies. This finding suggests that lipid peroxidation may be particularly relevant to the management of more severely depressed patients.
Elevated lipid peroxidation in peripheral blood may indicate a systemic elevation of oxidative stress and a failure of the antioxidant system to sufficiently neutralize the increased production of reactive oxygen species in MDD.11 Accordingly, oxidative stress may be a plausible link between MDD and several consistently comorbid medical conditions which are also characterized by oxidative stress, such as coronary artery disease, diabetes mellitus, and other chronic physical disabilities.2 Whether oxidative stress generally, and lipid peroxidation specifically, in MDD originates in the periphery or in the central nervous system is unclear, and likely not consistent across cases. Nevertheless, evidence increasingly suggests that MDD pathophysiology may be related to aberrant inflammatory/immune/oxidative activity in the periphery.9 The link between the presence of elevated peripheral concentrations of lipid peroxidation markers and neuropathological abnormalities on magnetic resonance imaging is also becoming clearer,47 supporting a role for peripheral concentrations of lipid peroxidation markers in MDD and its associated neuropathology.
The presence of lipid peroxidation in MDD may have important mechanistic implications. Specific markers of lipid peroxidation may indicate nuances in the pathways that led to the peroxidation of that lipid. Inflammatory and, more recently, neurodegenerative lipid mediators are emerging as relevant to MDD pathophysiology12 and may confer changes to the activity and regulation of relevant pathophysiological components such as the monoamines,48 inflammatory cytokines,49 and/or neurotrophins.50 Consistent evidence also demonstrates that lipid peroxidation and other oxidative species can generate immunogenic neoepitopes, which can activate autoimmune responses associated with MDD pathophysiology.9,32,51 Collectively, those changes can not only disrupt mood-regulating neural circuits6 but also lead to activation of neurodegenerative processes.12,13 Neurodegenerative processes may, in turn, contribute to increased sensitization to depressive episodes, leading to an increased episode frequency and duration.13 The majority of included studies measured malondialdehyde, which is a later-stage lipid peroxidation product that results from peroxidation of polyunsaturated fatty acids. Not only may malondialdehyde indicate ongoing oxidative stress processes, but it may also indicate ongoing production of proinflammatory lipids derived from arachidonic acid metabolism, both of which are relevant to MDD pathophysiology.52 Unfortunately, few other markers were measured by the included studies, precluding the exploration, and therefore interpretation, of marker differences related to MDD.
Of relevance to the interaction between oxidative stress and polyunsaturated fatty acids is the emerging potential role for omega-3 fatty acid supplements as a treatment for depressive symptoms.53 Omega-3 fatty acids are vulnerable to nonenzymatic peroxidation, which can result in the production of oxidative lipids such as 4-hydroxyhexenal. Though such omega-3 fatty acid peroxidation may increase resilience to oxidative free radicals, and possibly contribute to the purported antidepressant efficacy of omega-3 fatty acid supplements, it has been suggested that continued peroxidation of supplements in the context of persistent oxidative stress and long-term supplement use may be ultimately harmful to those with depression.54 Characterization of the antidepressant metabolites of omega-3 fatty acid supplements and the long-term effects of supplement use in those with depression may substantiate this potential harm and provide mechanistic insight into supplement efficacy.
This meta-analysis also found that treatment with antidepressant medications is associated with a consistent reduction in concentrations of lipid peroxidation markers over time. Those reductions did not appear to be related to the class of antidepressant medication used or to the duration of treatment. Although a significant correlation between the reduction in concentrations of lipid peroxidation markers and a reduction in depressive symptom severity was not observed, it is possible that the two may still be mechanistically linked, but may not be temporally synchronized. Collectively, these findings are concordant with qualitative reviews describing antidepressant benefits for lowering oxidative stress generally55,56 as well as individual studies describing antidepressant effects on lipid peroxidation markers in the brain and periphery in animal models,57–59 which may stem from reductions to the production of initial free radical species such as hydroxyl radicals and superoxide anions.60
Limitations
The presence of significant heterogeneity across included studies required the use of random effects models, which produce wider confidence intervals, and thus a more conservative measure of statistical significance. It is therefore possible that this meta-analysis did not detect truly significant relationships between certain study variables due to the conservative nature of the random effects models used. This meta-analysis attempted to limit the variance among included depressed groups by including only studies with MDD patients identified using standardized criteria (rather than community screening scale cut-offs) and those, which excluded patients with comorbid psychiatric and medical illnesses. Despite these efforts, interpretation of the meta-analytic findings was limited by inconsistent reporting of participant medical, medication, and/or dietary characteristics in the included studies. For example: not all of the included studies sufficiently reported demographic information, particularly related to the history, subtype, and/or treatment history of depression, and as such, interpretations of the relevance of lipid peroxidation to different presentations of MDD could not be attempted. It is important that these sample characteristics be reported by future studies using a depressed sample so that the influence of disease heterogeneity on biomarker results can be better understood. Of particular interest for future meta-analyses would be investigation of potential differences in lipid peroxidation between recurrent and first-episode depression, as this distinction might elucidate the oxidative stress – antioxidant dynamic after several recurrent depressive episodes as compared to a first episode. In keeping with this, measuring the concentrations of lipid peroxidation markers at different stages (severities) of oxidative stress would also enhance the mechanistic understanding of oxidative stress to lipids in MDD, and ought to be considered in future studies.
The inconsistent reporting of the change in depressive symptoms after antidepressant treatment limited the exploration of the correlation between change in lipid peroxidation and change in depressive symptoms to only four studies. As such, we were unable to fully address the question of whether the change in lipid peroxidation observed with antidepressant use is meaningfully associated with a change in depressive symptoms. Furthermore, inclusion of nonrandomized treatment studies may have introduced bias in the determination of that association, although the lack of randomized studies is a limitation of the literature rather than of this meta-analysis per se. Further exploration of this relationship may be needed for clarification.
This meta-analysis was also limited by the potential for the unreported inclusion of patients with comorbid psychiatric and/or medical disorders, which, if present, may have inflated the concentrations of lipid peroxidation markers in those with depression. However, the study findings remained significant in the subgroup of studies with a low risk of reporting bias, supporting our overall conclusions. The included studies were limited to the examination of peripheral differences in lipid peroxidation and therefore could not confirm a role for lipid peroxidation in the central nervous system in MDD. However, as mentioned, peripheral markers of lipid peroxidation have previously been shown to correlate with neuropathology in psychiatric disorders,47 indicating their relevance to illness-related processes. Additionally, two of the included studies measured lipid peroxidation markers from more than one sample source, and therefore pooled means and standard deviations were computed for each study. The formula recommended for pooling results in a slight underestimate of the standard deviation, which may have slightly inflated the potential for a significant finding for those studies. However, as only two studies were affected by this, it is unlikely to have influenced the overall finding. Finally, the cross-sectional nature of each included study comparing concentrations of lipid peroxidation markers between those with MDD and controls limited interpretation of causality between the two.
Despite these limitations, the results of this meta-analysis support the continued investigation of lipid peroxidation in the pathophysiology of MDD as well as the potential mechanisms underlying reductions in lipid peroxidation associated with antidepressant pharmacotherapy.
Conclusion
This meta-analysis found that concentrations of lipid peroxidation markers were significantly elevated in patients with MDD, consistent with a medium to large effect size, and that greater depressive symptom severity was associated with a greater degree of lipid peroxidation. Importantly, antidepressant treatment was associated with a significant reduction in concentrations of lipid peroxidation markers in patients with MDD. These findings support the involvement of oxidative stress generally and lipid peroxidation specifically in MDD. Continued investigation of oxidative stress to lipids and its downstream lipid mediators in MDD pathophysiology is warranted and may be best carried out in antidepressant-naive individuals.
Acknowledgments
This study was supported by the Ontario Mental Health Foundation (NH and KLL) and the Canadian Institutes of Health Research (number MOP-114913) (NH and KLL). GM was supported by an Institute of Aging and Canadian Institutes of Health Research Training Program in Neurodegenerative Lipidomics graduate award. ACA was supported by the Canadian Institutes of Health Research CIHR (number 133439) and the Brain and Behavior Foundation (number 19129). The authors would like to acknowledge Maureen Pakosh for library support.
Disclosure
The authors report no conflicts of interest in this work.
References
Patten SB, Wang JL, Williams JV, et al. Descriptive epidemiology of major depression in Canada. Can J Psychiatry. 2006;51(2):84–90. | ||
Sato S, Yeh TL. Challenges in treating patients with major depressive disorder: the impact of biological and social factors. CNS Drugs. 2013;27 Suppl 1:S5–S10. | ||
Judd LL, Paulus MP, Wells KB, Rapaport MH. Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. Am J Psychiatry. 1996;153(11):1411–1417. | ||
Pigott HE, Leventhal AM, Alter GS, Boren JJ. Efficacy and Effectiveness of Antidepressants: Current Status of Research. Psychother Psychosom. 2010;79(5):267–279. | ||
Gartlehner G, Hansen RA, Morgan LC, et al. Comparative benefits and harms of second-generation antidepressants for treating major depressive disorder: an updated meta-analysis. Ann Intern Med. 2011;155(11):772–785. | ||
Sibille E, French B. Biological substrates underpinning diagnosis of major depression. Int J Neuropsychopharmacol. 2013;16(8):1893–1909. | ||
Palta P, Samuel LJ, Miller ER 3rd, Szanton SL. Depression and oxidative stress: results from a meta-analysis of observational studies. Psychosom Med. 2014;76(1):12–19. | ||
Maes M, Yirmyia R, Noraberg J, et al. The inflammatory & neurodegenerative (I&ND) hypothesis of depression: leads for future research and new drug developments in depression. Metab Brain Dis. 2009;24(1):27–53. | ||
Moylan S, Berk M, Dean OM, et al. Oxidative & nitrosative stress in depression: why so much stress? Neurosci Biobehav Rev. 2014;45:46–62. | ||
Andreazza AC. Combining redox-proteomics and epigenomics to explain the involvement of oxidative stress in psychiatric disorders. Mol Biosyst. 2012;8(10):2503–2512. | ||
Sultana R, Perluigi M, Allan Butterfield D. Lipid peroxidation triggers neurodegeneration: a redox proteomics view into the Alzheimer disease brain. Free Radic Biol Med. 2013;62:157–169. | ||
Mazereeuw G, Herrmann N, Bennett SA, et al. Platelet activating factors in depression and coronary artery disease: a potential biomarker related to inflammatory mechanisms and neurodegeneration. Neurosci Biobehav Rev. 2013;37(8):1611–1621. | ||
Moylan S, Maes M, Wray NR, Berk M. The neuroprogressive nature of major depressive disorder: pathways to disease evolution and resistance, and therapeutic implications. Mol Psychiatry. 2013;18(5):595–606. | ||
Chalon S. Omega-3 fatty acids and monoamine neurotransmission. Prostaglandins Leukot Essent Fatty Acids. 2006;75(4–5):259–269. | ||
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed, Text Revision. Washington, DC: American Psychiatric Association; 2000. | ||
World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization; 1992. http://apps.who.int/classifications/icd10/browse/2015/en#/V. Accessed on April 4, 2014. | ||
Harris RJ, Bradburn MJ, Deeks JJ, Harbord RM, Altman DG, Sterne JAC. Metan: fixed- and random-effects meta-analysis. Stata J. 2008;8:3–28. | ||
Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2011. Available from: http://handbook.cochrane.org/. Accessed on April 4, 2014. | ||
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. | ||
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. | ||
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. | ||
Bal N, Acar ST, Yazici A, Yazici K, Tamer L. Altered levels of malondialdehyde and vitamin E in major depressive disorder and generalized anxiety disorder. Dusunen Adam. 2012;25(3):206–211. | ||
Bilici M, Efe H, Köroğlu MA, Uydu HA, Bekaroğlu M, Değer O. Antioxidative enzyme activities and lipid peroxidation in major depression: Alterations by antidepressant treatments. J Affect Disord. 2001;64(1):43–51. | ||
Dimopoulos N, Piperi C, Psarra V, Lea RW, Kalofoutis A. Increased plasma levels of 8-iso-PGF2alpha and IL-6 in an elderly population with depression. Psychiatry Res. 2008;161(1):59–66. | ||
Fadillioglu E, Kaya B, Uz E, Emre MH, Ünal S. Effects of moderate exercise on mild depressive mood, antioxidants and lipid peroxidation. Klinik Psikofarmakol Bülteni. 2000;10(4):194–200. | ||
Galecki P, Szemraj J, Bieńkiewicz M, Florkowski A, Galecka E. Lipid peroxidation and antioxidant protection in patients during acute depressive episodes and in remission after fluoxetine treatment. Pharmacol Rep. 2009;61(3):436–447. | ||
Ghodake SR, Suryakar AN, Kulhalli PM, Padalkar RK, Shaikh AK. A study of oxidative stress and influence of antioxidant vitamins supplementation in patients with major depression. Curr Neurobiol. 2012;3(2):107–111. | ||
Khanzode SD, Dakhale GN, Khanzode SS, Saoji A, Palasodkar R. Oxidative damage and major depression: the potential antioxidant action of selective serotonin re-uptake inhibitors. Redox Rep. 2003;8(6):365–370. | ||
Kotan VO, Sarandol E, Kirhan E, Ozkaya G, Kirli S. Effects of long-term antidepressant treatment on oxidative status in major depressive disorder: a 24-week follow-up study. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(5):1284–1290. | ||
Maes M, Kubera M, Mihaylova I, et al. Increased autoimmune responses against auto-epitopes modified by oxidative and nitrosative damage in depression: implications for the pathways to chronic depression and neuroprogression. J Affect Disord. 2013;149(1–3):23–29. | ||
Maes M, Mihaylova I, Kubera M, Uytterhoeven M, Vrydags N, Bosmans E. Increased plasma peroxides and serum oxidized low density lipoprotein antibodies in major depression: markers that further explain the higher incidence of neurodegeneration and coronary artery disease. J Affect Disord. 2010;125(1–3):287–294. | ||
Selley ML. Increased (E)-4-hydroxy-2-nonenal and asymmetric dimethylarginine concentrations and decreased nitric oxide concentrations in the plasma of patients with major depression. J Affect Disord. 2004;80(2–3):249–256. | ||
Stefanescu C, Ciobica A. The relevance of oxidative stress status in first episode and recurrent depression. J Affect Disord. 2012;143(1–3):34–38. | ||
Vargas HO, Nunes SO, de Castro MR, et al. Oxidative stress and inflammatory markers are associated with depression and nicotine dependence. Neurosci Lett. 2013;544:136–140. | ||
Yager S, Forlenza MJ, Miller GE. Depression and oxidative damage to lipids. Psychoneuroendocrinology. 2010;35(9):1356–1362. | ||
Baek D, Park Y. Association between erythrocyte n-3 polyunsaturated fatty acids and biomarkers of inflammation and oxidative stress in patients with and without depression. Prostaglandins Leukot Essent Fatty Acids. 2013;89(5):291–296. | ||
Rybka J, Kedziora-Kornatowska K, Banaś-Leżańska P, et al. Interplay between the pro-oxidant and antioxidant systems and proinflammatory cytokine levels, in relation to iron metabolism and the erythron in depression. Free Radic Biol Med. 2013;63:187–194. | ||
Bajpai A, Verma AK, Srivastava M, Srivastava R. Oxidative stress and major depression. J Clin Diagn Res. 2014;8(12):CC04–CC07. | ||
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. | ||
Black CN, Bot M, Scheffer PG, Cuijpers P, Penninx BW. Is depression associated with increased oxidative stress? A systematic review and meta-analysis. Psychoneuroendocrinology. 2015;51:164–175. | ||
Brown NC, Andreazza AC, Young LT. An updated meta-analysis of oxidative stress markers in bipolar disorder. Psychiatry Res. 2014;218(1–2):61–68. | ||
Tsutsui H, Kinugawa S, Matsushima S. Oxidative stress and heart failure. Am J Physiol Heart Circ Physiol. 2011;301(6):H2181–H2190. | ||
Rasool M, Farooq S, Malik A, et al. Assessment of circulating biochemical markers and antioxidative status in acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) patients. Saudi J Biol Sci. 2015;22(1):106–111. | ||
Kondo S, Toyokuni S, Iwasa Y, et al. Persistent oxidative stress in human colorectal carcinoma, but not in adenoma. Free Radic Biol Med. 1999;27(3–4):401–410. | ||
Versace A, Andreazza AC, Young LT, et al. Elevated serum measures of lipid peroxidation and abnormal prefrontal white matter in euthymic bipolar adults: toward peripheral biomarkers of bipolar disorder. Mol Psychiatry. 2014;19(2):200–208. | ||
Szelényi J, Vizi ES. The catecholamine cytokine balance: interaction between the brain and the immune system. Ann N Y Acad Sci. 2007;1113:311–324. | ||
Sadik CD, Luster AD. Lipid-cytokine-chemokine cascades orchestrate leukocyte recruitment in inflammation. J Leukoc Biol. 2012;91(2):207–215. | ||
Eyre H, Baune BT. Neuroplastic changes in depression: a role for the immune system. Psychoneuroendocrinology. 2012;37(9):1397–1416. | ||
Maes M, Mihaylova I, Kubera M, Leunis JC, Geffard M. IgM-mediated autoimmune responses directed against multiple neoepitopes in depression: new pathways that underpin the inflammatory and neuroprogressive pathophysiology. J Affect Disord. 2011;135(1–3):414–418. | ||
Dinan T, Siggins L, Scully P, O’Brien S, Ross P, Stanton C. Investigating the inflammatory phenotype of major depression: focus on cytokines and polyunsaturated fatty acids. J Psychiatr Res. 2009;43(4):471–476. | ||
Grosso G, Pajak A, Marventano S, et al. Role of omega-3 fatty acids in the treatment of depressive disorders: a comprehensive meta-analysis of randomized clinical trials. PLoS One. 2014;9(5):e96905. | ||
Assies J, Mocking RJ, Lok A, Ruhé HG, Pouwer F, Schene AH. Effects of oxidative stress on fatty acid- and one-carbon-metabolism in psychiatric and cardiovascular disease comorbidity. Acta Psychiatr Scand. 2014;130(3):163–180. | ||
Leonard B, Maes M. Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosci Biobehav Rev. 2012;36(2):764–785. | ||
Behr GA, Moreira JC, Frey BN. Preclinical and clinical evidence of antioxidant effects of antidepressant agents: implications for the pathophysiology of major depressive disorder. Oxid Med Cell Longev. 2012;2012:609421. | ||
Abdel Salam OM, Mohammed NA, Sleem AA, Farrag AR. The effect of antidepressant drugs on thioacetamide-induced oxidative stress. Eur Rev Med Pharmacol Sci. 2013;17(6):735–744. | ||
Abdel-Salam OM, Youness ER, Khadrawy YA, Sleem AA. Brain and liver oxidative stress after sertraline and haloperidol treatment in mice. J Basic Clin Physiol Pharmacol. 2013;24(2):115–123. | ||
Zafir A, Banu N. Antioxidant potential of fluoxetine in comparison to Curcuma longa in restraint-stressed rats. Eur J Pharmacol. 2007;572(1):23–31. | ||
Kirkova M, Tzvetanova E, Vircheva S, Zamfirova R, Grygier B, Kubera M. Antioxidant activity of fluoxetine: studies in mice melanoma model. Cell Biochem Funct. 2010;28(6):497–502. |
Supplementary materials
  | Table S1 Detailed search strategy |
  | Figure S1 Literature search results. |
References
Bilici M, Efe H, Köroğlu MA, Uydu HA, Bekaroğlu M, Değer O. Antioxidative enzyme activities and lipid peroxidation in major depression: Alterations by antidepressant treatments. J Affect Disord. 2001;64(1):43–51. | ||
Galecki P, Szemraj J, Bieńkiewicz M, Florkowski A, Galecka E. Lipid peroxidation and antioxidant protection in patients during acute depressive episodes and in remission after fluoxetine treatment. Pharmacol Rep. 2009;61(3):436–447. | ||
Ghodake SR, Suryakar AN, Kulhalli PM, Padalkar RK, Shaikh AK. A study of oxidative stress and influence of antioxidant vitamins supplementation in patients with major depression. Curr Neurobiol. 2012;3(2):107–111. | ||
Khanzode SD, Dakhale GN, Khanzode SS, Saoji A, Palasodkar R. Oxidative damage and major depression: the potential antioxidant action of selective serotonin re-uptake inhibitors. Redox Rep. 2003;8(6):365–370. | ||
Kotan VO, Sarandol E, Kirhan E, Ozkaya G, Kirli S. Effects of long-term antidepressant treatment on oxidative status in major depressive disorder: a 24-week follow-up study. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(5):1284–1290. | ||
Baek D, Park Y. Association between erythrocyte n-3 polyunsaturated fatty acids and biomarkers of inflammation and oxidative stress in patients with and without depression. Prostaglandins Leukot Essent Fatty Acids. 2013;89(5):291–296. | ||
Bajpai A, Verma AK, Srivastava M, Srivastava R. Oxidative stress and major depression. J Clin Diagn Res. 2014;8(12):CC04–CC07. | ||
Bal N, Acar ST, Yazici A, Yazici K, Tamer L. Altered levels of malondialdehyde and vitamin E in major depressive disorder and generalized anxiety disorder. Dusunen Adam. 2012;25(3):206–211. | ||
Dimopoulos N, Piperi C, Psarra V, Lea RW, Kalofoutis A. Increased plasma levels of 8-iso-PGF2alpha and IL-6 in an elderly population with depression. Psychiatry Res. 2008;161(1):59–66. | ||
Fadillioglu E, Kaya B, Uz E, Emre MH, Ünal S. Effects of moderate exercise on mild depressive mood, antioxidants and lipid peroxidation. Klinik Psikofarmakol Bülteni. 2000;10(4):194–200. | ||
Maes M, Mihaylova I, Kubera M, Uytterhoeven M, Vrydags N, Bosmans E. Increased plasma peroxides and serum oxidized low density lipoprotein antibodies in major depression: markers that further explain the higher incidence of neurodegeneration and coronary artery disease. J Affect Disord. 2010;125(1–3):287–294. | ||
Maes M, Kubera M, Mihaylova I, et al. Increased autoimmune responses against auto-epitopes modified by oxidative and nitrosative damage in depression: implications for the pathways to chronic depression and neuroprogression. J Affect Disord. 2013;149(1–3):23–29. | ||
Rybka J, Kedziora-Kornatowska K, Banaś-Leżańska P, et al. Interplay between the pro-oxidant and antioxidant systems and proinflammatory cytokine levels, in relation to iron metabolism and the erythron in depression. Free Radic Biol Med. 2013;63:187–194. | ||
Selley ML. Increased (E)-4-hydroxy-2-nonenal and asymmetric dimethylarginine concentrations and decreased nitric oxide concentrations in the plasma of patients with major depression. J Affect Disord. 2004;80(2–3):249–256. | ||
Stefanescu C, Ciobica A. The relevance of oxidative stress status in first episode and recurrent depression. J Affect Disord. 2012;143(1–3):34–38. | ||
Vargas HO, Nunes SO, de Castro MR, et al. Oxidative stress and inflammatory markers are associated with depression and nicotine dependence. Neurosci Lett. 2013;544:136–140. | ||
Yager S, Forlenza MJ, Miller GE. Depression and oxidative damage to lipids. Psychoneuroendocrinology. 2010;35(9):1356–1362. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.