Back to Journals » International Medical Case Reports Journal » Volume 13
A Huge Hydatid Pulmonary Cyst
Authors Azulay AA , Refaely Y, Ruderman L, Nesher L , Semionov M
Received 25 August 2019
Accepted for publication 13 December 2019
Published 24 February 2020 Volume 2020:13 Pages 61—64
DOI https://doi.org/10.2147/IMCRJ.S228657
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Ronald Prineas
Aviel Avraham Azulay,1,2 Yael Refaely,1,2 Leonid Ruderman,1,2 Lior Nesher,1,3 Michael Semionov1,4
1Soroka University Medical Center, Faculty of Health Sciences, Ben-Gurion University of the Negev, Beer-Sheva, Israel; 2Department of Cardiothoracic Surgery, Soroka University Medical Center, Faculty of Health Sciences, Ben-Gurion University of the Negev, Beer-Sheva, Israel; 3Infectious Diseases Unit, Soroka University Medical Center, Faculty of Health Sciences, Ben-Gurion University of the Negev, Beer-Sheva, Israel; 4Division of Anesthesiology and Critical Care, Soroka University Medical Center, Faculty of Health Sciences, Ben-Gurion University of the Negev, Beer-Sheva, Israel
Correspondence: Aviel Avraham Azulay
Department of Cardiothoracic Surgery, Soroka University Medical Center, Faculty of Health Sciences, Ben-Gurion University of the Negev, 151 Yitzhak Rager Blvd, Beer-Sheva, Israel
Tel +972 8-6400962
Fax +972 8-6400961
Email [email protected]
Abstract: This case report describes a patient with an unusually large pulmonary hydatid cyst and discusses important management issues.
Keywords: hydatid disease, lung infection, surgery complications, anesthesia, re-expansion pulmonary edema
Introduction
Hydatid cyst is caused by infection with the Echinococcus granulosus tapeworm.
Humans are incidental hosts of Echinococcus. The definitive hosts are dogs and other canines, while the intermediate hosts are most commonly sheep and occasionally other livestock. Human infection occurs mainly from contact with infected dogs or from ingesting fresh produce contaminated with parasite eggs. The infection is often asymptomatic. When symptoms and complications do develop, they are related to the site and the size of the hydatid cyst, with the liver and the lungs being the most prevalent sites for cyst implantation. The commonest symptoms of pulmonary hydatid cyst are cough, chest pain, dyspnea, and hemoptysis.1,2 Complications include cyst rupture into the bronchial tree or into the pleural cavity and secondary bacterial infection of the cyst.3 Cyst rupture can produce fever and acute hypersensitivity reactions including anaphylaxis, due to the release of antigenic material and secondary immunologic reactions.
Diagnosis of a pulmonary hydatid cyst is by CT and serology. Surgery is the preferred treatment. Preoperative treatment with albendazole reduces the risk of recurrence.4
The operative approach to pulmonary hydatid cyst needs to conform to the features of the cyst.5 Surgical options include capitonnage, intact endocystectomy, pericystectomy, wedge resection and lobectomy. During surgery, it is important to avoid fluid spillage which can lead to anaphylaxis and secondary seeding of the infection. If removal of the intact cyst is not feasible, 20% hypertonic saline should be injected into the cyst, and pads soaked with hypertonic saline should be placed over the surgical field prior to removing the contents of the cyst. Relapse may occur many years after treatment, and hence periodic follow-up is advisable.
Patient Description
A 19-year-old woman presented to the emergency room (ER) with abdominal pain. Two years previously she had onset of right upper quadrant abdominal pain and fatigue, and a few months later she also began complaining of chest discomfort and intermittent dyspnea. On the day of her admission, an abdominal ultrasound (US) examination was suspicious for a large epigastric cyst and she was therefore referred to the ER.
The patient had an unremarkable personal and familial medical history. She resided in a sheepherding Bedouin settlement where stray dogs commonly foraged.
On admission, her vital signs were temperature 38.6°C, heart rate 103 beats per minute, blood pressure 114/68 mm Hg, and oxygen saturation 98% in room air. On physical examination decreased breath sounds over the right lung and right upper quadrant abdominal tenderness were found.
Laboratory studies showed leukocytosis with neutrophilic predominance and an elevated CRP level.
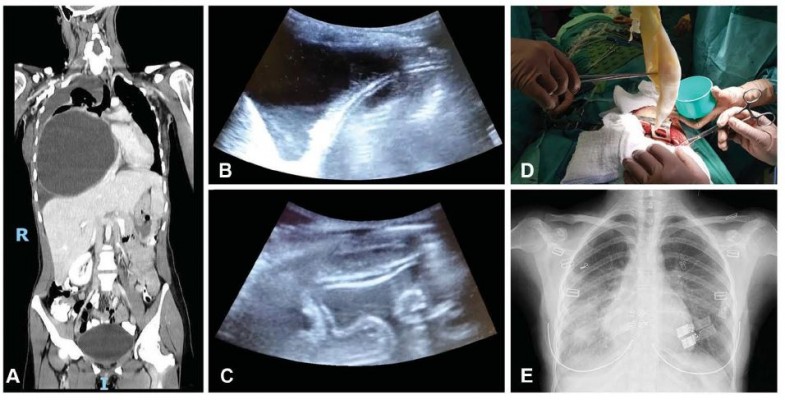
Double-contrast CT (computerized tomography) revealed a huge (15.0X14.5X16.0 cm) cyst in the right hemithorax encased in a multi-layered wall (Figure 1A). The cyst was causing almost total collapse of the right lung, significant leftward mediastinal shift, and compression of the Inferior vena cava, the right diaphragm, the right kidney and the liver. A medium-sized partially loculated right pleural effusion was also observed.
Serologic studies were positive for Echinococcus granulosus, confirming the diagnosis of a hydatid cyst.
The patient was treated for 6 days with albendazole and was then discharged in stable hemodynamic and respiratory condition, with the intention to perform surgery as soon as possible.
Following her discharge, a fulminant deterioration was noticed, and she was urgently re-admitted. On examination, she was tachycardic, tachypneic and severely dyspneic. Her oxygen saturation had decreased to 93% in room air and there was a total absence of breath sounds over her right lung.
The patient was taken urgently to the operating room. After intravenous administration of hydrocortisone, induction of anesthesia and intubation were performed. Intraoperative bronchoscopy showed findings of external compression and total occlusion of the right upper lobe bronchus, a bronchial blocker was inserted into the right main bronchus prior to withdrawal of the bronchoscope.
While induction of anesthesia and preparation for surgery was made, a US-guided drainage (Figure 1B and C) of 1.5 L of straw-colored pleural fluid and 0.5 L of straw-colored intra-cystic fluid was performed, following which 20% hypertonic saline was injected into the cyst cavity and re-drained after 20 mins. Exploratory thoracoscopy revealed a large encapsulated mass protruding from the lung parenchyma with extensive adhesions. These findings dictated transition to posterolateral thoracotomy which enabled extraction of the entire internal capsule (Figure 1D) and decapitation of the external capsule. The deep air leaks from the parenchyma were closed with sutures and biological glue. Repeat bronchoscopy performed after deflation of the bronchial blocker demonstrated normal airway patency. The right lung was almost fully expanded, and on ventilation of both lungs, no air leaks were demonstrated. However, a few moments later, the patient suddenly manifested signs of pulmonary edema including desaturation, hypotension and tachycardia. Foamy fluid was suctioned through the endotracheal tube. Arterial blood gas measurements showed respiratory acidosis with hypoxemia. Two drains were positioned in the pleural cavity, the incision was urgently closed, and the patient was immediately placed in the supine position. Respiratory stabilization was achieved by pressure-controlled mechanical ventilation and administration of IV furosemide and morphine and inhaled nitric oxide. Within 30 minutes, the patient’s condition improved and she was transferred to the Intensive care unit where she was successfully weaned from mechanical ventilation within a few hours. Her subsequent hospital course was uneventful, and she was discharged on the 5th postoperative day.
Comments
This case report describes the challenges encountered in managing an unusually large hydatid cyst of the lung with vital organ compression. It stresses some management issues that one should address, differing it from the current treatment algorithms.6
The first challenge was the timing of surgery. The patient initially presented in a clinically stable state despite the radiological characteristics of the cyst which was already causing mediastinal shift and compression of vital organs. The dilemma at this stage was whether to optimally prepare the patient for surgery by administration of Albendazole prior to intervention or to undertake urgent intervention. This case illustrates the need for urgent intervention even at the cost of incompletion of preoperatively Albendazole treatment course, due to the risk of immediate deterioration of the patient.
The second challenge was the anesthetic management. Due to airway compression caused by the mediastinal shift there was an obvious need for lung separation, and therefore a bronchial blocker was inserted. The risk of re-expansion pulmonary edema was anticipated while planning the operation and therefore its occurrence was dealt with immediately and effectively.
The third issue was the choice of a surgical technique. Since CT did not clarify whether the cyst could be entirely excised and whether normal lung parenchyma could be salvaged, the surgical approach was dictated by exploration of the pleural cavity. Complete resection of the cyst necessitated pneumonectomy, we therefore choose to do subtotal cystectomy with hydatidectomy (endocystectomy). When part of the outer capsule of a cyst is left in place, hypertonic saline should be applied to the cystic cavity, under closed observation. The use of 20% hypertonic saline in pleural cavity should be avoided due to the high rate of absorption and the accompanying complications. More however, in cases when the cyst is already erupted into the pleural cavity, which can be suggested by the presence of ipsilateral pleural effusion, it is assumed that the risks of anaphylactic shock and iatrogenic spillage of the cyst content are reduced and the precaution taken with the PAIR technique (puncture, aspiration, injection, re-aspiration) is less relevant.
Currently there are no designated guidelines for the management of giant lung hydatid cyst; therefore, extrapolation from the liver hydatid cyst guidelines needs to be made in accordance with the specific characteristics of each patient.
Ethical Statements
Written informed consent has been provided by the patient to have the case details and accompanying images published. No institutional approval was required to publish the case details.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Santivanez S, Garcia HH. Pulmonary cystic echinococcosis. Curr Opin Pulm Med. 2010;16(3):257–261. doi:10.1097/MCP.0b013e3283386282
2. Arinc S, Kosif A, Ertugrul M, et al. Evaluation of pulmonary hydatid cyst cases. Int J Surg. 2009;7(3):192–195. doi:10.1016/j.ijsu.2008.11.003
3. Turgut AT, Altinok T, Topçu S, Koşar U. Local complications of hydatid disease involving thoracic cavity: imaging findings. Eur J Radiol. 2009;70(1):49–56. doi:10.1016/j.ejrad.2008.01.002
4. Erzurumlu K, Hökelek M, Gönlüsen L, Tas K, Amanvermez R. The effect of albendazole on the prevention of secondary hydatidosis. Hepatogastroenterology. 2000;47(31):247–250.
5. Moro P, Schantz PM. Echinococcosis: a review. Int J Infect Dis. 2009;13(2):125–133. doi:10.1016/j.ijid.2008.03.037
6. Wen H, Vuitton L, Tuxun T, et al. Echinococcosis: advances in the 21st century. Clin Microbiol Rev. 2019;32(2):e00075–18.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

