Back to Journals » Clinical Ophthalmology » Volume 9
A Department-of-Anesthesiology-based management protocol for perioperative corneal abrasions
Authors Lichter J, Marr L, Schilling D, Hudson M, Boretsky R, Barad R, Chelly J
Received 11 March 2015
Accepted for publication 30 April 2015
Published 11 September 2015 Volume 2015:9 Pages 1689—1695
DOI https://doi.org/10.2147/OPTH.S84367
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Jessica R Lichter,1 Lawrence B Marr,2 Dennis E Schilling,3 Mark E Hudson,4 Robert H Boretsky,5 Roxana F Barad,6 Jacques E Chelly1–3
1Division of Clinical Research, Department of Anesthesiology, University of Pittsburgh, 2University of Pittsburgh Physicians, Department of Anesthesiology, UPMC Shadyside Hospital, 3UPMC Shadyside Hospital, 4University of Pittsburgh Physicians, Department of Anesthesiolgy, University of Pittsburgh Medical Center, 5Department of Anesthesiology, UPMC Shadyside, 6Department of Ophthalmology, UPMC Shadyside, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Introduction: Corneal abrasions (CAs) are the most prevalent ocular injuries in the perioperative period. Previously, patients at our community hospital would wait for an ophthalmologist to be available to manage these minor injuries. To decrease this waiting period – and thereby increase patient satisfaction – we developed an anesthesiology-based protocol to manage minor CAs arising in the recovery room. The current study sought to assess this protocol’s efficacy as well as further establish the incidence and some risk factors of CA.
Methods: This was a hospital-based, observational study. As per protocol, anesthesiologists saw and diagnosed any patient exhibiting symptoms of CA, after which they initiated a preestablished treatment regimen. To examine the efficacy of this protocol between March 2007 and December 2011, the number of CAs anesthesiologists managed and time to treatment were recorded. Additionally, the frequency of CAs was established along with some of their risk factors.
Results: Throughout the study period, there were 91,064 surgical cases, with 118 CAs (0.13% incidence). Anesthesiology alone managed 110 (93.22%) of these cases. The median time between the end of anesthesia to the time of prescribed ophthalmic medication was 156 minutes (first–third interquartile range: 108–219). All patients experienced resolution of symptoms by the morning following their complaint. Compared to the general surgical population, CA patients were older (P<0.01) and underwent longer surgeries (P<0.01).
Conclusion: Minor CAs can be safely and effectively managed using an anesthesiology-based approach. Advanced age and longer surgery are confirmed as risk factors for these injuries.
Keywords: corneal injuries, clinical protocols, patient care management, perioperative complications
Introduction
Corneal abrasions (CAs) are the most common ocular injuries in the perioperative period,1,2 occurring at an incidence typically between 0.013% and 0.17% of non-ocular surgeries.2–5 Although most are minor and involve only the surface epithelium, they still produce considerable discomfort. Generally, symptoms of CA are recognized between 1 hour and 3 hours following the conclusion of anesthesia,2,6 at which point an ophthalmologist is consulted to care for the injury. At community hospitals where ophthalmologists are not readily available, patients have to wait before receiving treatment. Undoubtedly, this prolonged waiting period may lead to unnecessary suffering and dissatisfaction.
For most patients, a combination of eye drops is the most effective method for healing CAs.7 Given this regimen’s simplicity, requiring that patients wait to see a specialist for the care of CAs seems especially unnecessary. Hence, to lessen the time between symptom onset and treatment – and in turn patient suffering and dissatisfaction – an anesthesiology-based protocol for the management of minor CAs identified in the post-anesthesia care unit (PACU) was developed with input from ophthalmology (Figure 1). This protocol became the standard approach at our institution. The current study sought to assess the effectiveness of this anesthesiology-based protocol, as well as clarify the incidence of CA and examine some of its associated risk factors.
  | Figure 1 Algorithm for the management of preoperative corneal abrasions. |
Methods
This was a medical record review approved by the University of Pittsburgh Institutional Review Board. The University of Pittsburgh Institutional Review Board has full Association for the Accreditation of Human Research Protection Program, Inc Accreditation and has approved this research examining perioperative CAs for the Department of Anesthesiology.
Each case of perioperative eye complaint was documented as it arose. Patients presenting with such complaints were treated in accordance with the guidelines of an anesthesiology-led protocol. The efficacy of this protocol is what we sought to evaluate in this study. After obtaining Institutional Review Board approval from the University of Pittsburgh, Pittsburgh, PA, for research protocol: Perioperative Corneal Abrasions: A Systematic Approach to Diagnosis and Management (University of Pittsburgh Institutional Review Board # PRO14030717), medical records were examined from March 1, 2007 to December 31, 2011 of all patients who complained of eye pain or discomfort following non-ocular surgery (barring pediatric and obstetric). Additionally, medical records of patients diagnosed with perioperative CA between 2002 and 2006 were reviewed to determine the amount of time these patients waited to receive treatment.
Description of anesthesiology-led protocol
Once in the PACU, the attending anesthesiologist saw any patient who reported eye discomfort or pain to the PACU nurse, as required by the anesthesiology-led protocol algorithm (Figure 1). The history of the complaint was taken, and a reporting form was completed. After gathering information pertaining to the nature of the complaint, anesthesiologists referred patients to ophthalmologists if they experienced a loss of vision, change in visual acuity, or severe or uncontrolled pain, as well as if they had a history of refractive surgery or eye disease. Additionally, consults were scheduled at the request of the patient or surgeon. For all other patients, anesthesiologists performed a bedside exam including the instillation of fluorescein dye and examination of the cornea with a Wizard Wand pocket light that provides cobalt blue light. All members of the Department of Anesthesiology were in-serviced in a bedside examination and the use of the Wand by Ophthalmology. Patients were scheduled for an ophthalmology consult if their exam revealed a large or complicated abrasion or the presence of a foreign body.
Regardless of whether a CA was noted in their bedside exam, all patients remaining under the care of Anesthesiology were treated with artificial tears (REFRESH TEARS PLUS® Eye Drops) instilled in the affected eye every 30 minutes for 2–3 hours until symptoms subsided. The eye was not patched. If the symptoms did not improve after 2–3 hours, then 0.5% erythromycin ophthalmic ointment was applied to the affected eye every 6 hours until symptoms subsided. If the patients were allergic to erythromycin, they received an alternative treatment (ciprofloxacin, tobramycin, bacitracin, or ketorolac 0.5% drops).
Patients were followed by the Department of Anesthesiology while they were in the hospital or until symptoms resolved and given instructions on how to manage their own care upon discharge. Inpatients were seen the morning following their complaint of eye pain, and if no improvement was noted, arrangements were made for them to be seen by an ophthalmologist. Outpatients were seen before discharge, at which point they were scheduled for a follow-up phone call and given instructions on how to apply artificial tears and/or ointment. If no improvement of symptoms was noted, arrangements were made for these patients to be seen by an ophthalmologist or primary care physician.
Data collection
Patients who complained of eye pain had their demographic, perioperative, and treatment information relevant to corneal injury recorded on a reporting form. The data used for the analysis were obtained either directly from this reporting form or by retrospectively reviewing patients’ medical records. Patient age and sex were recorded, along with associated medical conditions. Intraoperative factors that were reported include the type of surgery, surgical position, anesthesia type (general, spinal, or monitored anesthesia care [MAC]), anesthesia start and end time, and specific eye care used (eyes taped for general anesthesia, with or without the prior placement of a sterile petroleum ointment in the eyes; no eye protection for MAC or spinal). The perioperative factors reported on this form include the specifics of the patient complaint, results from an eye exam used to detect CAs, treatment prescribed, and follow-up observations.
When the data were available, time to treatment was measured in minutes from the end of anesthesia to the time the nurses charted the prescribed ophthalmic medication for patients diagnosed with CA in the perioperative period. Because symptoms of perioperative CA become apparent only after surgery, time to treatment represents the maximum amount of time patients had to wait between symptom onset and treatment under our anesthesiology-led protocol. The overall incidence of CA was also established along with two of the factors affecting its frequency, patient age, and duration of surgery. Duration of surgery was approximated based on the amount of time patients spent in the operating room.
Statistical analysis
Results were analyzed using R version 3.0.1.8 The Shapiro–Wilk test was used to assess the normality of the data. Two-sample Mann–Whitney U-tests were performed to compare the age and duration of surgery for patients diagnosed with CA to those not diagnosed with these ocular injuries. Data are presented as median (first–third interquartile range [IQR]) and mean (95% confidence interval [CI]). Alpha <0.05 was considered significant.
Results
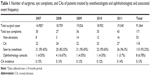
Over the study period, a total of 91,064 non-ocular surgical patients (except pediatric and obstetric) were followed. A total of 171 eye complaints were recorded and investigated. Table 1 represents the number of eye complaints, CAs, patients treated by an anesthesiologist, patients treated by an ophthalmologist, and associated event frequency. Out of the total number of surgical patients in this time period, 118 stained positive for a CA for an incidence of 0.13% (or 1.3 per 1,000 surgeries). Out of these 118 patients, 110 were seen only by an anesthesiologist, while eight received an ophthalmology consult, including six referred to an ophthalmologist at the request of either the patient (two) or the surgeon (four). Therefore, the anesthesia department successfully managed 93.22% of the perioperative CAs. The annual frequency of CA is also presented in Table 1. Incidence was consistent over the 5-year observational period, ranging between 0.12% and 0.15%.
Except for two patients who were referred to an ophthalmologist by the Department of Anesthesiology, all patients managed by Anesthesiology improved with conservative management, and were followed until symptoms abated. Out of the 110 patients seen exclusively by Anesthesiology, 85 experienced resolution of symptoms with artificial tears alone, nine with artificial tears followed by 0.5% erythromycin ophthalmic ointment, and eight with artificial tears followed by an alternative treatment (Table 2). Treatment information was not available for eight of the patients diagnosed with CA.
  | Table 2 Treatments given to patients diagnosed with corneal abrasions |
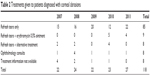
Using the anesthesiology-led protocol algorithm to identify symptoms of perioperative CA within the recovery room, anesthesiologists managed the care of 117 out of the 118 patients who presented with CAs within a few hours of their surgeries. Because the one patient who was identified outside of this window did not present with symptoms of CA until after she was extubated 2 days following her surgery, she was excluded from our calculation of time to treatment. Out of the remaining 117 cases of perioperative CA, data on time to treatment were available for 100 (84.55%). Mean time to treatment for these 100 patients was 177.84 (95% CI: 158.1–197.58), with a median time to treatment of 156 minutes (IQR: 108–219). The distribution of time to treatment for patients with CA is represented by the density histogram with the overlaying probability density function in Figure 2. Time to treatment was within 135 minutes for 39.0% of patients, within 180 minutes for 63.0% of patients, and within 225 minutes for 77.0% of patients. For only eight out of these 100 patients (8.0%) was the time to treatment greater than 315 minutes, and for only two (2.0%) was this interval greater than 495 minutes.
  | Figure 2 Density histogram of time to treatment for patients with corneal abrasion. |
During the study period, patients diagnosed with perioperative CAs were significantly older (P<0.01) than those in the general surgical population (Figure 3A). The average age of patients diagnosed with CAs was 64.49 years (95% CI: 62.28–66.7), compared to 58.1 years (95% CI: 57.99–58.21) for patients who did not develop these injuries. The median age was 66 years (IQR: 58.75–73) and 59 years (IQR: 48–70) for CA patients and non-CA patients, respectively.
Likewise, patients diagnosed with CA underwent surgeries of significantly longer duration (P<0.01) than those who were not diagnosed with these injuries (Figure 3B). Compared to patients who were not diagnosed with CA, who had a mean surgical duration of 132.73 minutes (95% CI: 132.04–133.42), the average surgical duration of patients diagnosed with CAs was 207.93 minutes (95% CI: 192.24–223.62). The median surgical duration was 202 minutes (IQR: 149.5–253) and 105 minutes (IQR: 61–166.5) for CA patients and non-CA patients, respectively.
Discussion
The current study demonstrates the effectiveness of an anesthesiology-led protocol for the identification and treatment of minor eye injuries identified in the recovery room. In hospitals where an ophthalmologist is not readily available, this eliminates the needs for the patient to wait before the diagnosis and treatment are initiated in the majority of patients exhibiting symptoms of perioperative CA.
Between March 2007 and December 2011, there were 91,064 patients undergoing surgeries in our hospital, with 171 presenting with eye complaints in the PACU. With the use of fluorescein staining and cobalt light, the Department of Anesthesiology diagnosed 118 of these patients with CAs. Subsequently, by following protocol guidelines, Anesthesiology alone successfully managed 110 (93.22%). Importantly, all patients diagnosed with CA experienced resolution of symptoms within 24 hours of treatment. Hence, our study demonstrates continued success with this anesthesiology-led protocol seeking to expedite the diagnosis and treatment of intraoperative CAs, evincing that anesthesiologists are capable of effectively managing these simple ocular injuries.
The main motivation for initiating an anesthesiologist-driven protocol was to reduce the amount of time between the patient experiencing eye pain or discomfort and the time of initiation of the appropriate treatment. In our study, the median time to treatment for patients exhibiting symptoms of CA perioperatively was 2.6 hours, with a range of 2 minutes to 8.82 hours. Further, the overwhelming majority of these patients (92.0%) received treatment in less than 5.25 hours. Importantly, it should be noted that the measure of time to treatment in our study is the most conservative estimate of the time patients had to consciously wait to receive treatment for their ocular injuries, as it includes both the time it takes for symptoms to surface and the time between symptom onset and treatment initiation. Given that 1) it typically takes between 1 hour and 3 hours just for the symptoms of CAs to become apparent,2–6 and 2) the mean time to treatment for CAs in our study (which includes this symptom onset period) is less than 3 hours, our study demonstrates that anesthesiologists trained under our protocol are attentive and quick to effectively manage CAs once symptoms arise. By reducing the time between symptom onset and treatment, our anesthesiology-led protocol may increase patient satisfaction.
CAs occurring perioperatively can arise from multiple factors, including trauma, chemical injury, and corneal edema.9 Although there is still debate on the frequency with which patients develop CAs, the American Society of Anesthesiologists closed-claims analysis found that CA was the most common ocular injury, accounting for 35% of all such injuries.10 At our hospital, the overall incidence of CA over the study period was 0.13%, which falls within the range of that observed in other studies.2–5 Year-to-year incidence over the study period was fairly constant, ranging from 0.12% to 0.15%.
In addition to evaluating the efficacy of an anesthesiology-led protocol for managing perioperative CAs and determining their incidence at our hospital, our study sought to further explore the risk factors associated with these injuries. Consistent with previous studies,3,4,6,11 we confirmed corneal injury to be associated with advanced age and longer surgeries.
Limitations and future studies
Despite collecting the data on CAs in a prospective fashion, this study is observational and faces all of the same limitations associated with a retrospective design. Consequently, findings from this study do not have the strength of those resulting from a randomized, double-blind, placebo-controlled trial, and certain data – such as the specific treatment prescribed and the time to treatment – were unavailable for a handful of patients. Furthermore, the study’s retrospective design did not allow for certain data to be readily examined, such as the exact time patients exhibited symptoms of CA. To more accurately determine the time between symptom onset and treatment initiation under an anesthesiology-led protocol for the management of CAs, future studies could document the time patients complain of eye pain prospectively. Having patient complaint serve as the primary mechanism by which perioperative CAs are identified can in itself be somewhat of a limitation, as those patients who do indeed develop CAs but do not experience acute pain in the recovery room will have their treatment delayed. Additionally, because this study was conducted only at one institution without an ophthalmologist readily available, some of its findings may not be generalizable to other sites. Finally, despite the fact that our database included over 90,000 patients, the number of CAs recorded was too small to perform more complex etiology-based analysis.
Conclusion
In summary, our data support the concept that anesthesiologists, with minimal training in examining the cornea, can safely and effectively manage simple CAs in the perioperative period, so long as they use proper selection criteria to refer difficult problems early and employ persistent follow-up. In an operative setting where ophthalmologists are generally not immediately available, the anesthesiology-led protocol we devised provides for early diagnosis and initiation of treatment. Having our protocol in place also obviates the need to have an ophthalmologist see the patients, reducing cost of care. Hence, this program, in conjunction with ophthalmology support, has allowed for timely and effective care to the small portion of individuals exhibiting symptoms of CA within our institution.
Acknowledgment
This study was funded by the Department of Anesthesiology, University of Pittsburgh Medical Center.
Disclosure
The authors report no conflicts of interest in this work.
References
Mecca RS. Postoperative recovery. In: Barash PG, Cullen BF, Stoelting RK, editors. Clinical Anesthesia. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:1396. | ||
Roth S, Thisted RA, Erickson JP, Black S, Schreider B. Eye injuries after nonocular surgery: a study of 60,965 anesthetics from 1988 to 1992. Anesthesiology. 1996;85:1020–1027. | ||
Yu HD, Chou AH, Yang MW, Chang CJ. An analysis of perioperative eye injuries. Acta Anaesthesiol Taiwan. 2010;48:122–129. | ||
Martin DP, Weingarten TN, Gunn PW, et al. Performance improvement system and postoperative corneal injuries: incidence and risk factors. Anesthesiology. 2009;111:320–326. | ||
Cucchiara RF, Black S. Corneal abrasion during anesthesia and surgery. Anesthesiology. 1998;69:978–979. | ||
Segal KL, Fleischut PM, Kim C, et al. Evaluation and treatment of perioperative corneal abrasions. J Ophthalmol. 2014;2014:901901. | ||
Fraser S. Corneal abrasion. Clin Ophthalmol. 2010;4:387–390. | ||
R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria; 2014. Available from: http://www.R-project.org/. | ||
White E, Crosse MM. The aetiology and prevention of peri-operative corneal abrasions. Anesthesia. 1998;53:157–161. | ||
Gild WM, Posner KL, Caplan RA, Cheney FW. Eye injuries associated with anesthesia: a closed claims analysis. Anesthesiology. 1992;76:204–208. | ||
Jabbur NS, O’Brien TP. Incidence of intraoperative corneal abrasions and correlation with age using Hansatome and Amadeus microkeratomes during laser in situ kertomileusis. J Cataract Refract Surg. 2003;29:1174–1178. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.