Back to Journals » Clinical Audit » Volume 13
A Cross-sectional Study to Analyze Blood and Blood Component Transfusion Practice at Tertiary Care Hospital of Ethiopia
Authors Muleta MB , Yisak EH, Gebreselassie HA, Tefera T , Berhanu E , Mekonnen AL, Alaye W, Akalu GT , Gelan EA, Bekele D
Received 1 July 2021
Accepted for publication 9 August 2021
Published 26 August 2021 Volume 2021:13 Pages 29—35
DOI https://doi.org/10.2147/CA.S326707
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Zoka Milan
Mahteme Bekele Muleta,1 Etsehiwot Haileselassie Yisak,1 Hana Abebe Gebreselassie,1 Tsega Tefera,1 Eden Berhanu,1 Adugna Lissanewerk Mekonnen,2 Woineshet Alaye,3 Gizachew Taddesse Akalu,4 Engida Abebe Gelan,1 Delayehu Bekele5
1Department of Surgery, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 2Department of Ophthalmology, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 3St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 4Department of Microbiology, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 5Department of Obstetrics and Gynecology, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Correspondence: Mahteme Bekele Muleta Email [email protected]
Purpose: This study aimed at looking into the demand and utilization of blood and blood components at a tertiary teaching hospital in Ethiopia.
Methods: A cross-sectional study was conducted from June 1, 2018 to August 31, 2018 at St Paul’s Hospital Millennium Medical College. Data on the types of blood products requested, indication for transfusion, availability of blood products and the utilization of different blood components, were collected by a structured questionnaire. Data were entered into SPSS version 20.1 and presented as frequency and percentage.
Results: Blood and blood components were requested for 819 patients during the study period. Blood group O RhD positive was the commonest blood group (BG) accounting for 292 (35.7%) of the study participants followed by blood group A RhD positive 259 (31.7%). Physicians requested 3290 units of blood and blood components for transfusion; however, only 1840 (55.9%) were available and transfused. Of the 1840 transfused blood and blood components, 771 (42%) were packed RBC, 460 (25%) platelet, 352 (19%) fresh frozen plasma, and 257 (14%) whole blood. Postpartum hemorrhage was the commonest indication of blood transfusion in obstetrics, while severe anemia was the leading emergency situation in pediatrics and internal medicine departments. Abdominal trauma was the leading indication of blood transfusion in the department of surgery.
Conclusion: This study finds a serious shortage of blood during emergency hours that may have a significant impact on patient survival. The hospital, in collaboration with the national blood bank, should devise a mechanism to alleviate the shortage.
Keywords: blood transfusion, transfusion demand, indication for transfusion, shortage of blood for transfusion, blood group
Background
Blood and blood component transfusions are an important part of medical care that saves millions of lives every year. Someone in the world requires blood every second for surgery, trauma, severe anemia, or pregnancy difficulties. Timely access to safe blood transfusion is a life-saving measure in many of these clinical conditions and can also prevent serious illness in these patients.1 There is a marked difference across the world regarding blood utilization. In well developed countries, blood components are being utilized for supporting advanced procedures, like cardiovascular surgeries, neurosurgeries, complicated trauma, and transplantation. But in low- and middle-income countries the lion's share is used to fix problems related with obstetric emergencies, severe anemia resulted from malaria, or malnutrition.1,2
A reliable supply of safe blood units is a well-recognized factor that assists effective health-care delivery around the world, and crucial for saving life in a variety of clinical circumstances. From the emergency room patient with an acute hemorrhage to the obstetric patient with antepartum/postpartum hemorrhage or the under-five youngster with anemic heart failure, prompt treatment is essential.3 It is also an apparent fact that as health systems expand and diagnostic and treatment options increase, the need for blood continues to rise internationally.
Paradoxically, despite a markedly inadequate blood supply in many countries, transfusions are sometimes given unnecessarily when the availability and use of simpler, less expensive treatments would provide equal or greater benefit. Not only does this put patient at risk of potentially catastrophic transfusion responses, but also widens the supply–demand gap and leads to blood and blood product shortages for patients who truly need them.1 Blood and its components are a very important scarce resource and hence should be used in a justifiable manner.4,5
Many blood transfusion rules and practices in Sub-Saharan Africa (SSA) are based on shaky or nonexistent evidence. Because its environment, consumers, and structures are completely different, SSA cannot extrapolate from research findings from advanced countries6 There are a scarcity of studies on blood and blood component utilization in Ethiopia in general, and in our college in particular. Hence, the aim of this study is to describe the common indications, type and number of requested and availability of blood and blood components in the four major departments of St Paul’s Hospital Millennium Medical College (SPHMMC).
Patients and Methods
A cross-sectional study was conducted from June 1, 2018 to August 31, 2018 at St Paul’s Hospital Millennium Medical College. The hospital is a tertiary teaching hospital and is located in Addis Ababa, the capital city of Ethiopia. The hospital has more than 20 clinical and basic science departments. The main hospital complex only accommodates the four departments; surgery, internal medicine, obstetrics and gynecology, pediatrics and child health, The other clinical departments are located in different building complexes, they include neurosurgery, orthopedics, otolaryngology, maxillofacial, ophthalmology, psychiatry and others. Therefore the study only included the four major departments which mainly utilize the central laboratory and blood bank. The blood bank in the hospital receives and stores blood, as a transitional hub, from the national blood bank and distributes the stored blood to the different departments on request.
Data on the requesting department, indication for transfusion, blood group, whether the request is for emergency or elective procedures and types of blood component requested, the number of requested bloods and available blood for transfusion were collected by a structured questionnaire every day, from the hospital blood bank blood transfusion registration book, department blood transfusion book, and medical records of the patient.
Ethical clearance was obtained from the Institutional Review Board of SPHMMC prior to data collection. All participants provided an informed consent to participate in the study in accordance with the Declaration of Helsinki.
Data was collected by trained surgery residents. Data was entered into statistical package for social science study software (SPSS) version 20.1. Categorical data are presented as frequency and percentage.
Result
Blood and blood components were requested for 819 patients during the study period. The blood group distribution of the 819 patients during the study period revealed that blood group O RhD positive 292 (35.7%) was the commonest followed by A RhD positive 259 (31.7%) as described in Table 1.
 |
Table 1 Blood Group Distribution Among Patients for Whom Blood Transfusion Requested, 2018 |
During the study period 3290 units of blood and blood components were requested and 1840 (55.9%) were transfused. Of the 1840 transfused blood and blood components 771 (42%) were packed RBC, 460 (25%) platelet, 352 (19%) fresh frozen plasma and 257 (14%) whole blood.
Blood component utilization by the different departments has shown that the obstetrics and gynecology department leads utilization of whole blood/packed RBC than any other department accounting for 338 units (37.7%), while internal medicine was the leading department in platelet and FFP utilization accounting for 231 (50.8%) and 128 (36.1%) of the components respectively as shown in Figure 1. Packed RBC and whole blood were interchangeably used during the study period.
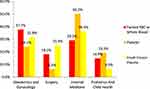 |
Figure 1 Blood and blood component utilization by each department, 2018. |
Emergency Conditions Requiring Blood Transfusion
A total of 823 units (80%) were used for emergency conditions whereas 205 units (20%) were used for perioperative stabilization of elective gynecological and surgical conditions. The emergency indications and availability of whole blood and/or packed RBC were discussed separately for each department herein.
Department of Obstetrics and Gynecology
The availability of requested blood for transfusion was 238/456 (52.2%) in obstetric emergency and 86/181 (47.5%) in emergency gynecological conditions. Of the 238 units transfused in the obstetrics unit postpartum hemorrhage (PPH) was the leading indication 70 (29.4%) followed by severe anemia 66 (27.7%). While in the gynecology unit gestational trophoblastic disease (GTD) was the leading indication of transfusion 24 (27.9%) followed by incomplete abortion 20 (23.3%) (Table 2).
 |
Table 2 Common Diagnosis Requiring Whole Blood or Packed Red Blood Cell Transfusion on Emergency Basis in the Different Units of Obstetrics and Gynecology Department, 2018 |
Department of Pediatrics and Child Health
In the department of pediatrics severe anemia was the leading indication of blood transfusion followed by congestive heart failure (CHF), while neonatal hyperbilirubinemia and severe anemia were the leading indication for blood transfusion in neonatal intensive care unit (NICU). The availability of blood for transfusion was 72/95 (75.8%) in the pediatric ward and OPD, while 91/93 (93.7%) in the NICU as shown in (Table 3).
 |
Table 3 Common Indications That Required Whole Blood or Packed RBC Transfusion in the Different Units of Department of Pediatrics and Child Health, 2018 |
Department of Internal Medicine
The amount of blood requested in the department of internal medicine was again far from the amount available for transfusion; 240/388 (61.9%) in the medical ward and 41/66 (62.1%) in the adult Intensive care unit (ICU). Anemia and upper gastrointestinal bleeding were the commonest indications for transfusion in the medical ward and emergency unit, while coagulopathy and disseminated intravascular coagulation were the leading indications for transfusion in the adult ICU (Table 4).
 |
Table 4 Common Indications for Whole Blood/Packed RBC During the Study Period in the Department of Internal Medicine, 2018 |
Department of Surgery
A total of 87 units of blood was requested on emergency time for 30 patients during the study period, however only 52 units of blood were available and transfused making the availability 59.8%. Abdominal trauma and small bowel obstruction were the leading indications for blood transfusion in the department of surgery on an emergency basis (Table 5).
 |
Table 5 Common Emergency Indications that Required Whole Blood and Packed RBC Transfusion During the Study Period in the Department of Surgery, 2018 |
Discussion
The current study revealed a severe scarcity of blood for transfusion for emergency and critical care. Blood and blood component shortages are a prevalent fact in third world countries where ignorance and misconception hinder adequate voluntary blood donation.7 Lack of blood for emergency transfusions was mentioned as a major, but poorly quantified and under-researched cause of maternal deaths in Sub-Saharan Africa.8 This was implied in our study too, where the shortage of whole blood or packed RBC during the emergency hours was very high in the obstetrics and gynecology department.
This serious shortage that was noticed in our study may also be because the country was in transition from replacement donors to voluntary donation to meet the WHO target of voluntary donation by 2020. This should be seriously evaluated as uncritical adoption of external advice and models, particularly those from more advanced countries, may lead to problems of sustainability.1 This shortage is also noted in the Indian study where 15% of the requested blood was found to be unsupplied when only voluntary donors were considered excluding the replacement donations.9
The WHO mentioned that in countries where diagnostic and treatment options are limited, a much greater proportion of blood is used to treat women with obstetric emergencies and children suffering from severe anemia, often resulting from malaria and malnutrition. Whereas In developed countries; transfusion is most commonly used to support advanced medical and surgical procedures, including trauma, cardiovascular surgery, neurosurgery, and transplantation.10
Our study proved the abovementioned assertion made by the WHO, as severe anemia was among the common indications of blood transfusion in pediatrics and the internal medicine department and postpartum hemorrhage as the leading cause in obstetric unit. This was also noticed in other studies from developing nations.11–13
Our findings demonstrated that O RhD positive was the most prevalent blood type among patients requiring blood transfusions; this is consistent with blood group distribution in the Ethiopian community as shown in other studies, with O RhD positive accounting for about 40% of the general population blood group.14,15 In studies conducted in Iran and India, the same blood group distribution was observed.9,16
In this study, packed RBC, platelet, and fresh frozen plasma were used for transfusion far more than whole blood. As the study demonstrated the pattern of utilization was by far superior to those of some Indian and African hospitals.4,6,16,17 However, it is significantly lower than countries such as Mauritius and the Kingdom of Saudi Arabia.11,12 In Mauritius in 2016, 98% of components were used, up from 40% in 2002.11 While encouraging the current work of the national blood bank, still it requires to strive hard to further increase the availability of components.
The study also revealed that the department of obstetrics and gynecology took the lead in utilization of whole blood/packed RBC. Internal medicine followed with the whole blood/packed RBC transfusion, but leading the platelet and FFP transfusion. Similar results were noted in a study done by Kaur et al where maximum demand was received from obstetrics and gynecology.14 However a study by Singh et al showed a different pattern of transfusion; where the largest number of units were supplied to general medicine 38%, followed by the pediatric ward.10 Our findings are explained in part by the enormous volume of deliveries at the hospital, which has the highest number of deliveries in the country, with over 10,000 each year.
The strength of our study is primary data collected from the respective departments on a daily basis and the limitation of the study is that it is a single center study.
Conclusion
Transfusions were commonly used for obstetrical emergencies, severe anemia, and injuries. This study revealed a severe scarcity of blood, which could have a substantial impact on patient survival. The hospital, in collaboration with the national blood bank, should devise a mechanism to alleviate the shortage by using a different mechanism. Strengthening the component utilization and reducing demand by complementary approaches to prevent severe anemia and treat hypovolemia are also important. Developing guidelines for blood and blood component utilization and auditing justification for blood requests and utilization by departments should also be given due emphasis.
Acknowledgment
We would like to thank the St Paul’s Hospital Millennium Medical college research directorate director for the administrative support to conduct this study. Our heartfelt appreciation goes to the blood bank staffs, interns, residents and nursing staffs of the college who have helped us a lot during data collection. The authors would like to acknowledge Mr Samuel Bekele for grammatical revision of the manuscript.
Disclosure
All authors read and approved the final manuscript. The authors report no conflicts of interest.
References
1. World Health Organization. Universal access to safe blood transfusion. World Health Organization; 2008. Available from: https://www.who.int/bloodsafety/publications/UniversalAccesstoSafeBT.pdf.
2. World Health Organization. Malaria control unit, United Nations Children’s Fund (UNICEF). The Africa Malaria Report 2003. World Health Organization; 2003.
3. Aneke JC, Okocha CE. Blood transfusion safety; current status and challenges in Nigeria. Asian J Transfus Sci. 2017;11(1):1–5. doi:10.4103/0973-6247.200781
4. Singhal M, Patel M, Kapoor D, Mittal D. A research analysis on blood component usage and wastage in blood bank and blood component center. J Physiol Pathopysiol. 2013;4(2):23–28.
5. Souza DAD, Silva FGE, Costa PJMDS. Critical evaluation of justifications for the transfusion of red blood cells: the reality of a government emergency hospital. Rev Bras Hematol Hemoter. 2013;35(4):263–267. doi:10.5581/1516-8484.20130080
6. Bates I, Hassall O, Mapako T. Transfusion research priorities for blood services in sub-Saharan Africa. Br J Haematol. 2017;177(6):855–863. doi:10.1111/bjh.14577
7. Allain J-P, Owusu-Ofori S, Bates I. Blood transfusion in sub-Saharan Africa. Transfus Altern Transfus Med. 2004;6(1):16–23. doi:10.1111/j.1778-428X.2004.tb00108.x
8. Bates I, Chapotera GK, McKew S, van den Broek N. Maternal mortality in sub-Saharan Africa: the contribution of ineffective blood transfusion services. BJOG. 2008;115(11):1331–1339. doi:10.1111/j.1471-0528.2008.01866.x
9. Singh SP, Nazreen H. A prospective study of blood usage pattern and demand supply assessment in a tertiary care hospital in India. J Blood Disord Transfus. 2015;6,6. doi:10.4172/2155-9864.1000317
10. Geißler RG, Franz D, Buddendick H. Retrospective analysis of the blood component utilization in a university hospital of maximum medical care. Transfus Med Hemother. 2012;39(2):129–138. doi:10.1159/000337956
11. Loua A, Sonoo J, Musango L, Nikiema JB, Lapnet-Moustapha T. Blood safety status in WHO African region countries: lessons learnt from Mauritius. J Blood Transfus. 2017;2017:1–8. doi:10.1155/2017/1970479
12. Alccantara TY, Alresheid AA, Al Shammary SA. A comparative study on blood componnnent utilization in selected hospital blood banks in Hail, KSA. IOSR J Nurs Health Sci. 2015;10:28–33.
13. Kaur P, Basu S, Kaur G, Kaur R. Analysis of the pattern of blood requisition and utilization. Natl J Integ. 2013;04(02):123–127.
14. Zerihun T, Bekele S. Pattern of ABO and rhesus blood groups distribution of five years survey in Jimma Town Blood Bank, South West Ethiopia. J Health Educ Res Dev. 2016;4(3). doi:10.4172/2380-5439.1000177
15. Girma N, Petros Y. Frequency of ABO, Rh Blood Group Alleles Among Oromo, Amhara and Wolayita Ethnic Group Students in Robe Secondary, Preparatory and Zeybela Primary School, Bale, Ethiopia. Int J Genet Genome. 2017;5:19. doi:10.11648/j.ijgg.20170502.11
16. Chegini A, Ebrahimi A, Maghari A. The evaluation of blood requests for transfusion and it’s utilization in four Iranian hospitals. Int Blood Res Rev. 2015;4(2):1–6. doi:10.9734/IBRR/2015/17177
17. Charan Paul MNP, Ommini S, Sreedhar VV, Narsinga Rao M, Bari Siddiqui MA. Pattern of blood component utilization in a tertiary care center. Der Pharm Lett. 2015;7(7):165–169.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
