Back to Journals » Infection and Drug Resistance » Volume 12
A comparison between dexlansoprazole modified release–based and lansoprazole-based nonbismuth quadruple (concomitant) therapy for first-line Helicobacter pylori eradication: a prospective randomized trial
Authors Tai WC , Liang CM , Bi KW , Kuo CM, Lu LS, Wu CK , Yang SC, Kuo YH, Lee CH, Huang CF , Hsu CN , Hsu PI, Wu DC , Hu TH, Wu KL , Chuah SK
Received 8 May 2019
Accepted for publication 3 September 2019
Published 16 September 2019 Volume 2019:12 Pages 2923—2931
DOI https://doi.org/10.2147/IDR.S213998
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sahil Khanna
Video abstract presented by Prof. Dr. Wei-Chen Tai
Views: 10855
Wei-Chen Tai,1 Chih-Ming Liang,1 Kuo-Wei Bi,2 Chung-Mou Kuo,1 Lung-Sheng Lu,1 Cheng-Kun Wu,1 Shih-Cheng Yang,1 Yuan-Hung Kuo,1 Chen-Hsiang Lee,3 Chih-Fang Huang,4 Chien-Ning Hsu,5 Pin-I Hsu,6 Deng-Chyang Wu,7 Tsung-Hui Hu,1,8 Keng-Liang Wu,1,8 Seng-Kee Chuah1,8
1Division of Hepatogastroenterology, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 2Division of Chinese Medicine, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 3Division of Infectious Diseases, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 4Division of Family Physician, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 5Department of Pharmacy, Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; 6Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Veterans General Hospital, National Yang-Ming University, Kaohsiung, Taiwan; 7Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Medical University Hospital and Kaohsiung Medical University, Kaohsiung, Taiwan; 8Chang Gung University College of Medicine, Taoyuan City, Taiwan
Correspondence: Seng-Kee Chuah; Chung-Mou Kuo
Division of Hepatogastroenterology, Kaohsiung Chang Gung Memorial Hospital, 123, Ta-Pei Road, Niao-Sung Hsiang, Kaohsiung 833, Taiwan
Tel +886 7 731 7123 ext. 8301
Fax +886 7 732 2402
Email [email protected]; [email protected]
Purpose: Steadily maintaining high intra-gastric PH is the major factor for successful Helicobacter pylori (H.pylori) eradication. It is important to search for a stronger PPI. Dexlansoprazole MR is a dual delayed release formulation PPI taken once daily which is capable of maintaining longer duration of high intra-gastric PH. It is very effective in treating gastroesophageal disease but reports on H, pylori eradication is very rare. This study sought to compare dexlansoprazole MR-based concomitant treatment and lansoprazole-based concomitant treatment in H. pylori infection and to investigate the factors that affect the eradication rates.
Methods: Two hundred two participants with H. pylori infection were included and randomly assigned to seven days of dexlansoprazole MR-based concomitant therapy (dexlansoprazole MR 60 mg once daily, clarithromycin 500 mg twice daily, amoxicillin 1 g twice daily and metronidazole 500 mg twice daily; DACM group) or a seven days of lansoprazole-based concomitant therapy (lansoprazole 30 mg twice daily, clarithromycin 500 mg twice daily, amoxicillin 1 g twice daily, and metronidazole 500 mg twice daily; LACM group). The participants were asked to perform urea breath tests eight weeks later.
Results: The eradication rates in the DACM group were 86.1% [95% confidence interval (CI): 77.8%–92.2%] in the ITT analysis and 90.6% (95% CI: 82.9%–95.6%) in the PP analysis, respectively, as compared with 90.1% (95% CI: 82.6%–95.2%) and 92.6% (95% CI: 85.5%–96.9%) (p=0.384 and p=0.572, respectively) in the LACM group for the same analyses. The adverse event rates were 11.5% in the DACM group and 10.2% in the LACM group (p=0.779).
Conclusion: As a first-line H. pylori treatment regimen, dexlansoprazole MR-based concomitant therapy attained a successful eradication rate of 90%, which was non inferior to that of lansoprazole-based concomitant treatment.
ClinicalTrials.gov identifier: NCT03829150.
Keywords: Helicobacter pylori eradication, strong proton-pump inhibitor, dexlansoprazole MR-based concomitant therapy, lansoprazole-based concomitant therapy, antibiotic resistance
Corrigendum for this paper has been published
Introduction
In patients infected with Helicobacter pylori (H. pylori), it is very important to choose a therapeutic medication able to attain a per-protocol eradication rate of 90% or more.1,2 However, the success H. pylori eradication using a standard triple-drug therapeutic approach has dropped to a rate of less than 80% because of the ongoing increase in clarithromycin-resistant strains of the organism worldwide.3–13 Prior research has indicated that seven to 10 days of concomitant treatment is an effective prescription in the presence of clarithromycin resistance in Taiwan.14,15
Importantly, the steady maintenance of a high intragastric pH is a major supporting factor for successful H. pylori eradication. A twice-daily PPI has been used in most studies to date;7,14,15 however, a twice-daily PPI approach may still not be strong enough to ensure a steady optimal intragastric pH, especially in those patients with genotypes predisposing them to rapid PPI metabolism. Therefore, a novel high-dose PPI dual therapy with amoxicillin, given either three or four times daily, has also been prescribed.16–19
It is important to search for a stronger PPI for the most optimal acid control that can be given ideally as a single dose daily. In view of the unmet need for an optimal acid-suppressing agent, it is worth mentioning another new drug with strong acid-suppressing effect: vonoprazan.20–24 This drug was reported to be able to maintain a much higher intragastric pH than the traditional PPIs. Unfortunately, this drug has not been made readily available worldwide. Most reports on vonoprazan in the literature were from a limited number of countries, especially Japan.
Dexlansoprazole MR is an R-enantiomer of lansoprazole. It has 3 to 5 times greater maximum concentration (Cmax), area under the plasma concentration–time curve (AUC), and a longer elimination half-life than S-lansoprazole because it contains two types of enteric-coated granules with different pH-dependent dissolution profiles that inhibit the proton pump. In this manner, gastric acid secretion can be effectively suppressed.25–27 The advantage of this dual delayed-release-formulation PPI is the once-daily dose to be taken after breakfast. In theory, dexlansoprazole MR should be able to maintain a steady optimal intragastric pH for H. pylori eradication. It is very effective in treating gastroesophageal disease but reports on H, pylori eradication is very rare. The present study was designed to compare dexlansoprazole MR-based concomitant therapy and lansoprazole-based concomitant therapy and to investigate the factors affecting the H. pylori eradication rates.
Materials and methods
Trial design and settings
Participants
From March 1, 2017 to February 28, 2019, we conducted an open-label trial by inviting 246 eligible naïve H. pylori–infected outpatient participants aged 18 years or older who were seen at Chang Gung Memorial Hospital in Kaohsiung, Taiwan. We excluded those patients who had taken the following medications within four weeks prior to invitation: antibiotics, nonsteroidal anti-inflammatory drugs, bismuth, and proton-pump inhibitors. We also excluded patients with a history of allergy to the study medications, those with severe comorbidities, those with a history of gastric surgery, pregnant women, and those who refused to participate or sign the consent form. Eventually, a total of 202 participants were included in this study.
When the participants underwent endoscopy examinations, two gastric specimens were taken from the antrum (one for rapid urease test and one for culture) and two were taken from the gastric body (one for rapid urease test and one for culture). Patients with any two positive results following rapid urease test, histology, and/or culture were eligible for recruitment into the present study. A standard questionnaire answered by all participants contained a complete medical history and basic data such as age; gender; and smoking, alcohol, and coffee and tea consumption habits.
The eligible H. pylori–infected participants were randomly assigned to two groups by using a computer-generated number sequence (ratio of 1:1). The two regimens were (1) dexlansoprazole MR-based concomitant treatment consisting of dexlansoprazole MR 60 mg q.d., clarithromycin 500 mg twice daily, amoxicillin 1 g twice daily, and metronidazole 500 mg twice daily for seven days (DACM group) and (2) lansoprazole-based concomitant treatment consisting of lansoprazole 30 mg twice daily, clarithromycin 500 mg twice daily, amoxicillin 1 g twice daily, and metronidazole 500 mg twice daily for seven days (LACM group).
Participants were requested to return on the eighth day to the outpatient clinic to evaluate them for treatment compliance by reviewing the remaining medications not taken by the participants (Figure 1). If the participant did not finish at least 80% of the medications, they were considered to be participants with poor compliance.7,9,10 Meanwhile, the adverse events were also recorded by a four-point scale system.19 The success of H. pylori eradication was confirmed by a negative urea breath test at eight weeks later with a cutoff value of 4.8% of δ13CO2. The outcome of H. pylori eradication and the factors affecting the eradication rates in both groups were analyzed by the statistician at the end of the study.
 |
Figure 1 Schematic flowchart of study design. |
Culture and antimicrobial resistance
In our laboratory, all stock cultures were preserved at −80 °C in Brucella broth (Becton, Dickinson and Company, Franklin Lakes, NI, USA) augmented with 20% glycerol (Sigma Chem. Co., St. Louis, MO, USA). The antibiotic susceptibility was tested by E test (AB Biodisck, Solna, Sweden) with MIC values of≥0.5, ≥5, ≥1, ≥4, and≥8 mg/L as the resistant breakpoints for amoxicillin, clarithromycin, levofloxacin, tetracycline, and metronidazole, respectively, as established by an international committee (Eucast. Breakpoint Tables for Interpretation of MICs and Zone Diameters).
Randomization
Our statistician generated randomization lists from a computer system to obtain the “random sequences” for the two groups at a ratio of 1:1 and a block for every six participants. After the doctors decided to enroll participants into the study and the participants signed a consent form, opaque envelopes containing information on respective treatment allocations were given to the participants. The participants received the prescriptions and then the medications.
Statistical analysis
The eradication rate of concomitant therapy by conventional PPI (twice daily) was found to be 92% in our previous studies.14,19 In this study, we assumed a true difference in favor of the DACM treatment of 8% and so decided to enroll 202 patients to make sure that the upper limit of a one-sided 95% confidence interval (CI) was 90%, excluding a difference toward the control group of 8% (<10% loss to follow-up). The primary outcome was successful eradication. The outcome comparisons were performed by using the chi-squared test with or without Yates correction for stability and Fisher’s exact test when appropriate. Statistical significance was reached when a p-value of less than 0.05 was attained. A univariate analysis by way of logistic regression modeling was performed to investigate the factors affecting the eradication rates.
Results
Figure 2 shows the deposition of patients. There were initially 246 eligible naïve H. pylori–infected patients, but 38 refused to participate and six met the exclusion criteria (ie, had comorbidities). Eventually, a total of 202 participants were enrolled (n=101 per group) in the ITT analysis. Five patients in the DACM group and three patients in the LACM group were lost during follow-up, leaving 95 participants in the DACM group and 98 in the LACM group, respectively, for inclusion in PP analysis. The demographic data of the two groups are summarized in Table 1. The treatment compliance rates were 100% in both groups.
 |
Figure 2 Patients’ deposition. |
 |
Table 1 Demographic data and endoscopic appearance of two groups of patients |
The eradication rates in the DACM group were 86.1% (95% CI: 77.8%–92.2%) in the ITT analysis and 90.6% (95% CI: 82.9%–95.6%) in the PP analysis, while the eradication rates in the LACM group were 90.1% (95% CI: 82.6%–95.2%) in the ITT analysis and 92.6% (95% CI: 85.5%–96.9%) in the PP analysis (p=0.384 and p=0.572, respectively) (Table 2). The adverse event rates were similar in the two groups (11.5% in the DACM group vs 10.2% in the LACM group; p=779). The most frequently encountered adverse event in both the DACM and LACM groups was diarrhea (7.3% and 7.1%, respectively), but all cases were mild (Table 3). Other adverse events included nausea sensation (3.1% and 2.0%), abdominal pain (2.1% and 3.1%), dizziness (1% in the LACM group only), and headache (1% in the LACM group only). Univariate analysis showed that antibiotics resistance to clarithromycin, metronidazole, and dually to both clarithromycin and metronidazole were factors that affected the eradication rates (p=0.043, p=0.003, and p<0.001, respectively (Table 4)).
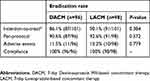 |
Table 2 The major outcomes of the two groups of patients |
 |
Table 3 Adverse events of the two groups of patients |
 |
Table 4 Univariate analysis of the clinical factors influencing the efficacy of H. pylori eradication therapy |
There were only 42 participants who agreed to undergo H. pylori culture, and the positive culture rate was 90.5% (38/42). Hence, the antibiotic resistance report in the current study included amoxicillin (0%), clarithromycin (21%), and metronidazole (26.32%). The successful H. pylori eradication rate among patients with the amoxicillin- and clarithromycin-susceptible strains was 100% (23/23) in this study, yet was only 33.3% for those with amoxicillin- and clarithromycin-resistant strains (1/3). Six out of eight participants (75%) with clarithromycin resistance and seven of 10 (70%) participants with metronidazole resistance assigned to both the concomitant therapy groups showed eradication.
Discussion
In this study, we used a dual delayed-release formulation of dexlansoprazole MR in a combination therapy prescribed once daily (DACM). We observed that seven days of said therapy achieves a high PP eradication rate as first-line anti–H. pylori therapy and was not inferior to seven-day lansoprazole-based concomitant therapy, although the dexlansoprazole MR-based concomitant regimen did not reach a 90% success rate in ITT analysis.
Concomitant therapy consists of a PPI in combination with clarithromycin, amoxicillin, and metronidazole for seven to 14 days. Many studies have reported the achievement of eradication rates of more than 90% for seven-day concomitant therapy regimens in both ITT and PP analyses between 2010 and 2012 in Taiwan and Japan.14,15,28 The current study in comparison attained a PP eradication rate of more than 90% but did not achieve a 90% success rate in ITT analysis, a finding that was also reported in other studies conducted in Taiwan.15 A possible explanation for the decline in ITT eradication may involve multiple factors. Unfortunately, there were only 42 participants who agreed to undergo H. pylori culture; although the positive culture rate was 90.5% (38/42); we are unable to comment much on the possible impact of potential antibiotics-resistant strains from this study due to the small culture population. There are suggestions that extending the treatment duration to 14 days could improve upon the presently reported eradication rates.29
One of the crucial factors to achieving successful H. pylori eradication was to maintain a steady intragastric pH of more than 6 so as to optimize the antibiotic sensitivity. Nevertheless, a high-dose PPI was needed with a dosage of two to four times daily among conventional PPIs such as esomeprazole, lansoprazole, rabeprazole, and pantoprazole. Another gastric acid suppressant, Dexlansoprazole MR, is an oral dual delayed-release-formulation PPI. It contains two types of enteric-coated granules with different pH-dependent dissolution profiles.26 Such a dual delayed release-formulation had the advantage of lengthening the acid suppression duration by way of extension of the plasma concentration of the drug. Another advantage of note is the once-daily dose taken after breakfast or any time of the day before or after the meal. This was proven in a comparative trial, where dexlansoprazole taken once daily showed better control of esophageal pH than 30 mg of lansoprazole taken once daily. Another, single-day pH study comparing the pharmacokinetic effects of different PPIs at 12–24 hrs postdose in healthy adult subjects reported that the mean percentage of time with a pH of more than 4 and the average of the mean pH were higher for dexlansoprazole than esomeprazole (60% vs 42%, p<0.001 and 4.5 vs 3.5, p<0.001, respectively).30,31 In theory, it should be able to maintain a steady optimal intragastric pH for H. pylori eradication. Indeed, our study results showed that DACM is not inferior as a first-line H. pylori eradication regimen in comparison with LACM (86.1% vs 90.1% in ITT analysis and 90.6% vs 92.6% in PP analysis with similar adverse events and compliance rates).
Nevertheless, the inevitable problematic issue is that strains with dual resistance to clarithromycin and metronidazole could negatively impact the efficacy of H. pylori eradication.3,11 In our study, antibiotic resistance rates were found for amoxicillin (0%), clarithromycin (21%), and metronidazole (26.32%). Univariate analyses of our data identified that clarithromycin resistance, metronidazole resistance, and dual resistance to both were the factors that reduced the efficacy of concomitant therapy. Six out of eight participants (75%) with clarithromycin resistance and seven of 10 participants (70%) with metronidazole resistance assigned to both of the concomitant therapy groups showed eradication. On the other hand, only one out of three participants with dual resistance demonstrated eradication. These findings could imply that dual resistance was a major factor affecting the outcome of concomitant therapy. Unfortunately, the number of patients infected dually with clarithromycin-resistant and metronidazole-resistant strains was small in this study, making the possibility of a type II error likely.
The limitation in this study was that the culture of H. pylori was completed only in a small subset of patients (n=42) but multiple drugs were used. Further, we were unable to discuss the influence of drug-resistant strains in the success rate of eradication because there was a possibility of type II error due to the small sample size of patients with culture reports, although the positive culture rate was 90.5% (38/42). However, both study groups used the same regimens for H. pylori eradication (concomitant therapy), and this might minimize the influence of antibiotics-resistant strains on treatment outcome.
Given that vonoprazan is still not available worldwide, by attempting to consider a stronger PPI, this study represents a very rare investigation and reported that dexlansoprazole MR-based concomitant therapy attained a PP success rate of more than 90%. This fulfilled the grade B report card32,33 and could be a promising perspective to explore for H. pylori treatment using current data. Notably, although the current results are promising, they should be replicated in different populations before assuming generalization of the findings.
Conclusion
In conclusion, seven-day dexlansoprazole MR-based concomitant therapy achieved a high PP eradication rate as first-line anti–H. pylori therapy and was not inferior to seven-day lansoprazole-based concomitant therapy.
Ethics approval and informed consent
This study’s protocol was approved by the institutional review board and the ethics committee of Chang Gung Memorial Hospital (IRB104-2643A3). All participants provided written informed consent before enrollment. None of the patients were minors. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee. The ClinicalTrials.gov registration identifier is NCT03829150.
Data sharing statement
No data will be shared except besides what is included in the manuscript
Acknowledgment
The authors would like to acknowledge Miss Ching-Yi Lin for her assistance in this study. This work was funded by grants from the Research Foundation of Chang Gung Memorial Hospital (CMRPG8F1421), Taiwan.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest exist in this work.
References
1. Chuah SK, Tsay FW, Hsu PI, Wu DC. A new look at anti-helicobacter pylori therapy. World J Gastroenterol. 2011;17:3971–3975. doi:10.3748/wjg.v17.i35.3971
2. Rimbara E, Fischbach LA, Graham DY. Optimal therapy for helicobacter pylori infections. Nat Rev Gastroenterol Hepatol. 2011;8:79–88. doi:10.1038/nrgastro.2010.210
3. Graham DY, Fischbach L. Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut. 2010;59:1143–1153. doi:10.1136/gut.2009.192757
4. Gisbert JP, Pajares R, Pajares JM. Evolution of Helicobacter pylori therapy from a metaanalytical perspective. Helicobacter. 2007;12:50–58. doi:10.1111/j.1523-5378.2007.00576.x
5. Gumurdulu Y, Serin E, Ozer B, et al. Low eradication rate of Helicobacter pylori with triple 7-14 days and quadruple therapy in Turkey. World J Gastroenterol. 2004;10:668–671. doi:10.3748/wjg.v10.i5.668
6. Bigard MA, Delchier JC, Riachi G, Thibault P, Barthelemy P. One-week triple therapy sing omeprazole, amoxycillin and clarithromycin for the eradication of Helicobacter pylori in patients with non-ulcer dyspepsia: influence of dosage of omeprazole and clarithromycin. Aliment Pharmacol Ther. 1998;12:383–388. doi:10.1046/j.1365-2036.1998.00315.x
7. Chuah SK, Liang CM, Lee CH, et al. A randomized control trial comparing two levofloxacin-containing second-line therapies for Helicobacter pylori eradication. Medicine (Baltimore). 2016;95:e3586. doi:10.1097/MD.0000000000004864
8. Chuah SK, Tai WC, Lee HC, Liang CM. Quinolone-containing therapies in the eradication of Helicobacter pylori. Biomed Res Int. 2014;2014:151543. doi:10.1155/2014/151543
9. Chuah SK, Hsu PI, Chang KC, et al. Randomized comparison of two non-bismuth-containing second-line rescue therapies for Helicobacter pylori. Helicobacter. 2012;17:216–223. doi:10.1111/j.1523-5378.2012.00937.x
10. Chuah SK, Tai WC, Hsu PI, et al. The efficacy of second-line anti-Helicobacter pylori therapy using an extended 14-days levofloxacin/amoxicillin/protonpump inhibitors -a pilot study. Helicobacter. 2012;17:374–381. doi:10.1111/j.1523-5378.2012.00960.x
11. Megraud F. H. pylori antibiotic resistance: prevalence, importance, and advances in testing. Gut. 2004;53:1374–1384. doi:10.1136/gut.2003.022111
12. De Francesco V, Giorgio F, Hassan C, et al. Worldwide H. pylori antibiotic resistance: a systematic review. J Gastrointestin Liver Dis. 2010;19:409–414.
13. Graham DY, Lu H, Yamaoka Y. Therapy for Helicobacter pylori infection can be improved: sequential therapy and beyond. Drugs. 2008;68:725–736. doi:10.2165/00003495-200868060-00001
14. Tai WC, Liang CM, Lee CH, et al. Seven-day non-bismuth containing quadruple therapy could achieve a grade “A” success rate for first-line. Helicobacter Pylori Eradication Biomed Res Int. 2015;2015:623732.
15. Wu DC, Hsu PI, Wu JY, et al. Sequential and concomitant therapy with 4 drugs are equally effective for eradication of H. pylori Infection. Clin Gastroenterol Hepatol. 2010;8:36–41. doi:10.1016/j.cgh.2009.09.030
16. Ren L, Lu H, Li HY, et al. New dual therapy for primary treatment of Helicobacter pylori infection: a prospective randomized study in Shanghai, China. J Dig Dis. 2014;15:622–627. doi:10.1111/1751-2980.12186
17. Yang JC, Lin CJ, Wang HL, et al. High-dose dual therapy is superior to standard first-line or rescue therapy for Helicobacter pylori infection. Clin Gastroenterol Hepatol. 2015;13:895–905. doi:10.1016/j.cgh.2014.10.036
18. Zullo A, Ridola L, Francesco VD, et al. High-dose esomeprazole and amoxicillin dual therapy for first-line Helicobacter pylori eradication: a proof of concept study. Ann Gastroenterol. 2015;28:448–451.
19. Tai WC, Liang CM, Kuo CM, et al. A 14 day esomeprazole- and amoxicillin-containing high-dose dual therapy regimen achieves a high eradication rate as first-line anti-Helicobacter pylori treatment in Taiwan: a prospective randomized trial. J Antimicrob Chemother. 2019;1(74):1718–1724. doi:10.1093/jac/dkz046
20. Mori H, Suzuki H. Role of acid suppression in acid-related diseases: proton pump inhibitor and potassium-competitive acid blocker. J Neurogastroenterol Motil. 2019;25:6–14. doi:10.5056/jnm18139
21. Masaoka T, Kameyama H, Yamane T, et al. Pathophysiology of potassium-competitive acid blocker-refractory gastroesophageal reflux and the potential of potassium-competitive acid blocker test. J Neurogastroenterol Motil. 2018;24:577–583. doi:10.5056/jnm18036
22. Oshima T, Arai E, Taki M, et al. Randomised clinical trial: vonoprazan versus lansoprazole for the initial relief of heartburn in patients with erosive oesophagitis. Aliment Pharmacol Ther. 2019;49:140–146. doi:10.1111/apt.15062
23. Sugimoto M, Yamaoka Y. Role of vonoprazan in helicobacter pylori eradication therapy in Japan. Front Pharmacol. 2018;9:1560. doi:10.3389/fphar.2018.01560
24. Abadi ATB, Ierardi E. Vonoprazan and helicobacter pylori treatment: a lesson from Japan or a limited geographic phenomenon? Front Pharmacol. 2019;10:316. doi:10.3389/fphar.2019.00848
25. Katsuki H, Yagi H, Arimori K, et al. Determination of R (+)- and S (-)-lansoprazole using chiral stationary-phase liquid chromatography and their enantioselective pharmacokinetics in humans. Pharm Res. 1996;13:611–615. doi:10.1023/A:1016062508580
26. Metz DC, Howden CW, Perez MC, Larsen L, O’Neil J, Atkinson SN. Clinical trial: dexlansoprazole MR, a proton pump inhibitor with dual delayed-release technology, effectively controls symptoms and prevents relapse in patients with healed erosive oesophagitis. Aliment Pharmacol Ther. 2009;29:742–754. doi:10.1111/j.1365-2036.2009.03954.x
27. Vakily M, Zhang W, Wu J, Atkinson SN, Mulford D. Pharmacokinetics and pharmacodynamics of a known active PPI with a novel dual delayed release technology, dexlansoprazole MR: a combined analysis of randomized controlled clinical trials. Curr Med Res Opin. 2009;25:627–638. doi:10.1185/03007990802693883
28. Yanai A, Sakamoto K, Akanuma M, Ogura K, Maeda S. Non-bismuth quadruple therapy for first-line Helicobacter pylori eradication: a randomized study in Japan. World J Gastrointest Pharmacol Ther. 2012;3:1–6. doi:10.4292/wjgpt.v3.i1.1
29. Fallone CA, Chiba N, van Zanten SV, et al. The toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology. 2016;151:51–69. doi:10.1053/j.gastro.2016.04.006
30. Chiang HH, Wu DC, Hsu PI, et al. Clinical efficacy of 60-mg dexlansoprazole and 40-mg esomeprazole after 24 weeks for the on-demand treatment of gastroesophageal reflux disease grades A and B: a prospective randomized trial. Drug Des Devel Ther. 2019;13:1347–1356. doi:10.2147/DDDT.S193559
31. Kukulka M, Eisenberg C, Nudurupati S. Comparator pH study to evaluate the single-dose pharmacodynamics of dual delayed-release dexlansoprazole 60 mg and delayed-release esomeprazole 40 mg. Clin Exp Gastroenterol. 2011;4:213–220. doi:10.2147/CEG.S24063
32. Graham DY, Lu H, Yamaoka Y. A report card to grade Helicobacter pylori therapy. Helicobacter. 2007;12:275–278. doi:10.1111/j.1523-5378.2007.00518.x
33. Graham DY, Lu H, Yamaoka Y. Therapy for Helicobacter pylori infection can be improved. Drugs. 2008;68:725–736. doi:10.2165/00003495-200868060-00001
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
