Back to Journals » Clinical Pharmacology: Advances and Applications » Volume 13
A Case of Thrombocytosis Associated with Enoxaparin Therapy in an Adolescent
Received 2 July 2021
Accepted for publication 23 September 2021
Published 18 October 2021 Volume 2021:13 Pages 203—207
DOI https://doi.org/10.2147/CPAA.S327541
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Arthur E. Frankel
Robert Murray,1 Joseph T Tobias1– 3
1Department of Pediatrics, Division of Pediatric Critical Care Medicine, Nationwide Children’s Hospital, Columbus, OH, USA; 2Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, OH, USA; 3Department of Anesthesiology & Pain Medicine, The Ohio State University College of Medicine, Columbus, OH, USA
Correspondence: Robert Murray
Department of Pediatrics, Division of Pediatric Critical Care Medicine, Nationwide Children’s Hospital, 700 Children’s Drive, Columbus, OH, 43205, USA
Tel +1 614 722-4200
Fax +1 614 722-4203
Email [email protected]
Abstract: Secondary thrombocytosis, often referred to as a reactive thrombocytosis, is more common than primary thrombocytosis and has many potential etiologies including anemia, infection, inflammation, medications, and post-splenectomy. When considering the critically ill patient in the ICU setting potential medication-related etiologies of thrombocytosis should be included in the differential diagnosis. We present a 15-year-old adolescent with a traumatic brain injury who developed thrombocytosis that was temporally related to the administration of enoxaparin. There was a prompt return of the platelet count to normal following the discontinuation of enoxaparin therapy which led to the probable diagnosis of enoxaparin-induced thrombocytosis.
Keywords: enoxaparin, thrombocytosis, platelet count, heparin, anticoagulation
Introduction
Thrombocytosis is generally defined as a platelet count greater than 450,000/mm3 (normal range 150–450/mm3). Thrombocytosis can be further classified as either primary or secondary.1–3 Primary thrombocytosis is caused by an intrinsic mechanism within the megakaryocyte or its precursor cells. Primary thrombocytosis, which is far less common than secondary thrombocytosis, can be caused by acquired or inherited defects in the genes which regulate thrombopoiesis. These can include malignancies such as chronic myeloid leukemia or acute myeloid leukemia, polycythemia vera, and myelodysplastic syndromes. Features suggestive of a primary rather than secondary cause include: unexplained vasomotor symptoms (flushing or pruritis), constitutional symptoms (night sweats, fever or weight loss), splenomegaly, thrombosis in unusual sites, an abnormal peripheral blood smear or a family history suggestive of thrombosis. In such scenarios, referral to a hematologist for further work-up is warranted.
Secondary thrombocytosis, often referred to as a reactive thrombocytosis, is more common than primary thrombocytosis and has many potential etiologies including anemia, infection, inflammation, medications, and post-splenectomy.2,3 The presence of thrombocytosis is often found incidentally on a complete blood count (CBC). The initial work-up should include a repeat CBC with differential, a review of the peripheral blood smear, and a thorough history and physical examination, including a review of the recent medical history and medications. We present a 15-year-old adolescent with a traumatic brain injury (TBI) who developed thrombocytosis that was noted to be temporally related to the administration of enoxaparin. An approach to identify the etiology of thrombocytosis is presented, previous reports regarding the association of thrombocytosis with enoxaparin are reviewed, and the potential pathophysiology is discussed.
Case Report
Review of this case and presentation in this format was approved by the Institutional Review Board of Nationwide Children’s Hospital. Informed consent for publication was obtained from the patient’s mother and the patient was unable to assent given the residual effects of his TBI. The patient was a 15-year-old male who was admitted to the Pediatric Intensive Care Unit (PICU) with a severe TBI following a motor vehicle collision. He was a previously healthy teenager with a medical history significant only for attention deficit hyperactive disorder. His other injuries at the time of admission included bilateral pelvic fractures and a left internal carotid artery dissection. Following admission, a right femoral central venous catheter was placed for access during the management of his increased intracranial pressure (ICP). Due to the internal carotid artery dissection, a heparin infusion was started at 20 units/kg/hour with a low anti-Xa goal of 0.3–0.5 IU/mL. Full anticoagulation with a higher anti-Xa was deemed contraindicated due to the cerebral contusions associated with his TBI and concerns for intracranial bleeding. His hospital course was unremarkable and there was gradual resolution of the increased ICP related to his TBI. Due to clinical concern for thrombus formation, an ultrasound of the right leg was performed, revealing a non-occlusive catheter associated thrombosis in the right femoral vein. In consultation with neurosurgery, it was determined that anticoagulation was appropriate and therapeutic enoxaparin (40 mg twice a day) was started and the heparin infusion was discontinued. An anti-Xa level was obtained following the initiation of enoxaparin with a peak level of 0.55 IU/mL, within the desired therapeutic goal for our patient (0.35–0.7 IU/mL). Platelet count trends before, during and after enoxaparin therapy are presented in Figure 1. Following the initiation of enoxaparin, on day 13 of hospitalization, there was an increase in platelet count and hematology consultation was obtained. The increasing platelet count continued from hospital day 13 to 20. As other possible causes for the thrombocytosis were ruled out including anemia, infection and inflammation, medication causes were considered. It was at this time, day 19, that enoxaparin was discontinued. After the discontinuation of enoxaparin his platelet count continued to rise for one subsequent day followed by a gradual return of the platelet count to normal values. Due to a continued need to provide some level of anticoagulation for this patient’s internal carotid artery dissection aspirin (81 mg daily) was started on hospital day 19 following the discontinuation of enoxaparin. As his acute medical concerns began to resolve the patient was transferred to an inpatient rehabilitation facility to continue working on mobility, self-care, cognition, and oral intake. He was able to be discharged home from inpatient rehabilitation approximately 2 months after his initial TBI.
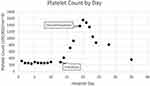 |
Figure 1 Platelet count over time. Enoxaparin therapy was started on hospital day 13 and discontinued on hospital day 19. |
Discussion
Enoxaparin is a low molecular weight heparin compound commonly used for both the prevention and treatment of thrombotic diseases. Clinical uses include the prophylaxis of deep vein thrombosis (DVT), as well as therapeutic anticoagulation for various thrombotic conditions including pulmonary embolism. Clinical advantages over unfractionated heparin include therapeutic anticoagulation with subcutaneous administration, a longer plasma half-life, a linear dose-response relationship, feasibility for administration in the outpatient setting and a limited need to monitor its anticoagulant effect.4 The most common adverse effects of enoxaparin include anemia, hemorrhage, and thrombocytopenia.4 Peripheral edema, ecchymoses, nausea, hematuria, alterations in liver function tests, confusion, and fever have also been reported.
In our patient, there was a temporal association between the initiation of enoxaparin therapy and the development of thrombocytosis. During the work-up for thrombocytosis in conjunction with pediatric hematology specialists, other potential etiologies were ruled out. At the time that our patient developed thrombocytosis, they were approximately 2 weeks removed from the initial traumatic injury, their clinical condition was improving, they were not anemic, and there was no evidence of an ongoing infectious or inflammatory process. Other possible pharmacologic causes were reviewed and ruled out. Therefore, the conclusion was that the reactive thrombocytosis was most likely secondary to enoxaparin. Most importantly, there was a prompt decline in the platelet count following discontinuation of the enoxaparin. This conclusion is support by our calculated Naranjo score of 7, presented in Figure 2, suggesting a probable adverse drug reaction linking enoxaparin to thrombocytosis in our patient.
Thrombocytosis associated with enoxaparin has been anecdotally reported in various clinical scenarios previously in both adult and pediatric patients.5–8 A multicenter study evaluating the safety of enoxaparin for the prevention of postoperative thromboembolism unexpectedly noted thrombocytosis in the study cohort of 290 adult patients.9 The patients received either 20 or 40 mg of subcutaneous enoxaparin once daily with platelet counts evaluated prior to surgery and on the 5th, 7th, 11th, and 15th postoperative day. Although no thrombocytopenia or thrombosis were noted, there was an increase in postoperative platelet counts in most patients. Postoperative thrombocytosis was greater in patients with neoplasms as well as those with excessive perioperative blood loss and transfusion requirements. No thrombotic complications related to the thrombocytosis were noted. The authors concluded that as changes in the platelet counts were not the main topic of their study, the data should be regarded only as preliminary and further investigations are needed to resolve the cause of the observed phenomenon of thrombocytosis with enoxaparin.
The mechanism by which enoxaparin leads to thrombocytosis has not been fully elucidated. In a murine experiment, an increase in platelet count, immature megakaryocytes, and colony-forming unit megakaryocytes in the bone marrow occurred after the intraperitoneal administration of a low molecular weight heparin compound, fraxiparin, for 4 days.10 The authors hypothesized that fraxiparin interacts with heparin cofactor II and antithrombin III to promote megakaryocyte colony formation. It has also been demonstrated that heparin can potentiate the megakaryocyte-poietic activity of the C-Mpl ligand and interleukin-6 as well as neutralize the inhibitory actions of platelet factor 4 and transforming growth factor β1 on megakaryocyte colony growth.11 These factors would result in the stimulation of hematopoiesis in the bone marrow leading to an increase in platelet formation.
Conclusion
Although physicians are generally aware of the association of heparin with thrombocytopenia (heparin-induced thrombocytopenia), thrombocytosis has been only anecdotally reported. We suggest that enoxaparin should be considered in the differential diagnosis of thrombocytosis, supported by a Naranjo Score of 7 in our case, suggesting a probable adverse drug reaction. Cessation of heparin therapy is suggested if feasible based on the risk-benefit ratio of the individual patient. It is generally postulated that reactive thrombocytosis does not represent a significant thrombotic risk however, no conclusion has been reached regarding this potential association. Currently, there is limited evidence-based medicine on which to guide decisions regarding the need for anti-platelet therapy such as aspirin in patients with thrombocytosis.12,13 Although we chose not to initiate additional therapy in our patient other than transition to once daily aspirin (81 mg) for their internal carotid artery dissection, clinicians should evaluate the thrombotic and bleeding risks on a case-by-case basis to develop the most appropriate management plan for each patient.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Skoda RC. Thrombocytosis. Hematology. 2009;2009:159–167. doi:10.1182/asheducation-2009.1.159
2. Harrison CN, Bareford D, Butt N, et al. Guideline for investigation and management of adults and children presenting with a thrombocytosis. Br J Haemat. 2010;149:352–375. doi:10.1111/j.1365-2141.2010.08122.x
3. Yohannan MD, Higgy KE, Al-Mashhadani SA, Santhosh-Kumar CR. Thrombocytosis. Clin Pediatr. 1994;33:340–343. doi:10.1177/000992289403300605
4. Hofmann T. Clinical application of enoxaparin. Expert Rev Cardiovasc Ther. 2004;2:321–337. doi:10.1586/14779072.2.3.321
5. Ranze O, Ranze P, Magnani HN, et al. Heparin-induced thrombocytopenia in paediatric patients: a review of the literature and a new case treated with danaparoid sodium. Eur J Pediatr. 1999;158(suppl 3):S130–3. doi:10.1007/PL00014338
6. Tonbul A, Uras N, Tayman C, Halici T, Polat A, Mansur Tatli M. Thrombocytosis associated with enoxaparin: a very rare cause in newborns. Platelets. 2010;21:300–302. doi:10.3109/09537101003649807
7. Xiang T, Cheng M. Enoxaparin-induced reactive thrombocytosis: a case report. Thromb J. 2021;19:34. doi:10.1186/s12959-021-00290-x
8. Hummel MC, Morse BC, Hayes LE. Reactive thrombocytosis associated with enoxaparin. Pharmacotherapy. 2006;26:1667–1670. doi:10.1592/phco.26.11.1667
9. Ziaja K, Simka M, Krupowies A, Dugaj M, Ludyga T. Thrombocytosis after prophylactic administration of enoxaparin: unexpected findings in a Polish prospective multicenter trial on the efficacy and safety of enoxaparin in the prevention of postoperative thromboembolism. Int Angiol. 1999;18:65–69.
10. Shen ZX, Basara N, Xi XD, et al. Fraxiparin, a low-molecular-weight heparin, stimulates megakaryocytopoiesis in vitro and in vivo in mice. Br J Haematol. 1994;88:608–612. doi:10.1111/j.1365-2141.1994.tb05080.x
11. Han ZC, Bellucci S, Shen ZX, et al. Glycosaminoglycans enhance megakaryocytopoiesis by modifying the activities of hematopoietic growth regulators. J Cell Physiol. 1996;168:97–104. doi:10.1002/(SICI)1097-4652(199607)168:1<97::AID-JCP12>3.0.CO;2-M
12. Buss DH, Stuart JJ, Lipscomb GE. The incidence of thrombotic and hemorrhagic disorders in association with extreme thrombocytosis: an analysis of 129 cases. Am J Hematol. 1985;20:365–372. doi:10.1002/ajh.2830200408
13. Randi ML, Stocco F, Rossi C, Tison T, Girolami A. Thrombosis and hemorrhage in thrombocytosis: evaluation of a large cohort of patients (357 cases). J Med. 1991;22:213–223.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

