Back to Journals » International Medical Case Reports Journal » Volume 7
A case of anxiety associated with miliary tuberculosis
Authors Alosaimi F , Alkharboush F, Altuwariqi M
Received 26 March 2014
Accepted for publication 22 April 2014
Published 20 June 2014 Volume 2014:7 Pages 111—115
DOI https://doi.org/10.2147/IMCRJ.S64855
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Fahad D Alosaimi,1 Feras A Alkharboush,2 Maram H Altuwariqi1
1Department of Psychiatry, King Saud University, Riyadh, Kingdom of Saudi Arabia; 2College of Medicine, King Saud University, Riyadh, Kingdom of Saudi Arabia
Abstract: Miliary tuberculosis (TB) is a serious infection with various presentations that can perplex even the most experienced clinicians. To our knowledge, there is a lack of published reports that link psychiatric symptoms directly with miliary TB (either alone or co-occurring with other medical symptoms). Mental health workers may, therefore, not consider, and consequently miss, this important diagnosis. Here we are reporting a case of cyclical anxiety occurring in a 67-year-old patient. For 3 years prior to admission, the patient failed to respond to multiple courses of different antianxiety medications. The patient required hospital admission as he deteriorated and had a reduced level of consciousness. A chest X-ray revealed bilateral nodules and a magnetic resonance imaging scan showed multiple enhancing tuberculous lesions in the cerebral white matter, brain stem, and cerebellum. A diagnosis of miliary TB was finally made. Several characteristics of this case suggest that the diagnosed anxiety disorder was due to miliary TB. However, we cannot exclude the possibility that generalized anxiety disorder preceded the onset of miliary TB or that both diseases were coincidental. The report serves as a reminder that organic causes for psychiatric symptoms always need to be considered, particularly if they follow an atypical pattern or fail to improve with usual psychiatric medications.
Keywords: anxiety disorder, elderly, psychosomatic, case report, Saudi Arabia
Introduction
Tuberculosis (TB) is a serious infectious disease caused by the bacillus Mycobacterium tuberculosis. The incidence of TB has been falling globally for several years, and mortality due to TB has decreased by about 40% since 1990. In spite of this, the global burden of TB remains enormous. In 2012, there were an estimated 8.6 million new cases of TB and 1.3 million people died from TB.1 In Saudi Arabia, there was an annual increase in the number of TB cases registered from 3,284 in 2000 to 3,964 in 2009, and the highest rates were seen in the ≥65-years age group.2 However, the mortality among TB patients show a declining trend among Saudis starting from the year 2003, and it was positively correlated with advanced age and male sex (7.3% compared to 5.3% mortality among females).3
TB typically affects the lungs (pulmonary TB), but can also affect other sites (extrapulmonary TB) in about 10% of cases.4 Extrapulmonary TB is diagnosed when a patient has tuberculous lesions in organs other than the lungs (eg, pleura, lymph nodes, abdomen, genitourinary tract, skin, joints and bones, meninges).5 Miliary TB, which represents approximately 20% of extrapulmonary TB, results from lymphohematogenous dissemination of TB bacilli.6 The disease is usually seen in children after the age of 6 months and in elderly adults (65 years and above) due to the relative waning of immunity.7,8 TB symptoms usually last for several weeks – median 4–9 weeks in different studies.9,10
Anxiety disorders are a category of disorders characterized by excessive worrying, uneasiness, apprehension, and fear of future events. They comprise one of the most common psychiatric disorders worldwide;11,12 as of 2010, approximately 273 million people (4.5% of the global population) had an anxiety disorder.13 Generalized anxiety disorder (GAD) is a particularly common subtype, with a lifetime incidence of 4.1% and a 12-month incidence of 2.1% in the US population.14 GAD is commonly seen in the primary care setting where the prevalence is estimated to be 7.6%, with most of the affected individuals being females.12,14
The diagnosis of GAD is based on the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria, which includes a history of at least 6 months of “excessive anxiety and worry” about a variety of events or activities, and associated significant difficulty in controlling the worry.11 Three or more (or only one in children) of the following symptoms on most days over the 6 months prior to presentation are required to make the diagnosis: irritability; muscle tension; insomnia; concentration problems; fatigue; and feeling restless. These symptoms should cause significant distress or impairment in the patient’s function. Finally, the DSM-5 criteria of GAD stipulate that these anxiety features are not better explained by another mental disorder and are not attributable to another medical condition or substance that is known to pathophysiologically cause anxiety. In the event of anxiety symptoms being confirmed to be secondary to another medical condition, the diagnosis of “anxiety disorder due to another medical condition” can be made.11
Medical disorders that can be associated with anxiety include chronic pain conditions and endocrine, cardiovascular, respiratory, gastrointestinal, and neurological disorders.15 Therefore, thorough history taking, physical examination, and laboratory testing should be performed to rule out medical causes of anxiety such as migraine, thyroid and parathyroid dysfunction, diabetes, arrhythmias, coronary heart disease, asthma, chronic obstructive pulmonary disease, irritable bowel syndrome, stroke, and seizure disorder.15–17 Additionally, practitioners evaluating anxious patients should consider a substance- or medication-induced etiology, such as legal and illegal drug use (eg, cocaine or other stimulants, such as caffeine), drug withdrawal (eg, cessation of the use of alcohol, opiates, or benzodiazepines), or prescribed medications (eg, corticosteroids and sympathomimetics).18 The pathophysiology of GAD is thought to involve dysfunctional neural processing of emotional stimuli, probably mediated by the adrenal system.15,16 GAD symptoms can be relieved with cognitive behavioral therapy as well as antianxiety medications such as selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, and the calcium channel modulator pregabalin.19
Case report
A 67-year-old male Saudi patient was referred to our psychosomatic service. The patient was a retired elementary school teacher from Al-Qassim province, Saudi Arabia, and due to difficulty in communicating with the patient, the medical history was obtained from his sons. The patient had a history of hypertension and symptoms of benign prostatic hypertrophy for many years. Three years prior to presentation, he began to have repetitive behaviors; in particular, checking and rechecking his underwear for possible urine remnants, which intruded on his prayer duties in the mosque and was noticed by his sons. His thoughts became more intrusive as he planned to do Umrah (minor pilgrimage) to the holy city of Makkah, when he started to repeatedly ask questions about religious rulings. He went on to express excessive worry about his responsibilities towards his family’s ownership and inheritance. His condition progressed into continuous fear and worry throughout the day that began to disturb his sleep, first with sleep interruption and later with more persistent insomnia. The sons described a special pattern to their father’s anxiety; extreme worry associated with description of palpitations, or occasionally numbness, at the beginning of the day (at dawn prayer) followed by failure to resume sleep in an effort to reduce his anxiety. The symptoms progressed throughout the day, culminating in a more severe and persistent form associated with continuous fatigue by sunset. After sunset, the patient experienced considerable relief and could resume enjoying the company of his family and friends.
No specific triggers to the patient’s anxiety were described; there was no history of specific fears, flashbacks, or avoidant behaviors, and his sons did not observe irritability. The patient was witnessed crying only three times over this period, but did not experience persistent low mood, and had normal appetite except over the last few weeks of his illness. He did not report any suicidal ideation.
There was no family or personal history of other psychiatric disorders. Premorbid, he was described as an introverted religious person who, while active at family gatherings, only reluctantly socialized with strangers.
In the 3 years prior to presentation, the patient also frequently described “chest heat”, but, given the context of symptoms, his sons ascribed this to a psychological rather than organic cause. The patient therefore presented to several local psychiatrists during this period who diagnosed GAD. He was initially prescribed paroxetine 10 mg once daily (od) for 2 months, to which he showed no response. He was then switched to escitalopram, initially at a dose of 5 mg od, and then 10 mg od for about a year, which was accompanied by a small improvement, but he complained of a feeling of lethargy. Escitalopram was later replaced with mirtazapine 15 mg and fluvoxamine 50 mg (later increased to 100 mg) for another 6 months, but with no response. The last course was replaced finally with sertraline 50 mg od (later increased to 75 mg), again with no response. No significant side effects were reported during the use of these medications.
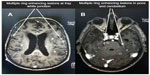
The cyclical nature of the patient’s anxiety symptoms and, finally, deterioration of his condition encouraged his sons to seek medical advice at a tertiary center. The patient was referred to our hospital and electively admitted. He presented with a 6-week history of continuous fever, a reduced level of consciousness, mild dry cough, moderate loss of appetite and weight, and left-sided weakness. There was no history of chest pain, hemoptysis, nausea, vomiting, headache, dizziness, or syncope. A chest X-ray showed bilateral nodular lesions in the lungs (Figure 1). A computed tomography (CT) scan was performed to rule out stroke and showed mild brain atrophy with ischemic changes in the small vessels. A magnetic resonance imaging scan revealed small left corpus callosum lacunar infarcts as well as extensive small vessel disease, in addition to widespread multiple enhancing lesions in the cerebral white matter, brain stem, and cerebellum (Figure 2A and B). Sputum and blood cultures were positive for M. tuberculosis. The patient was therefore diagnosed with miliary TB involving the brain. An abdominal and pelvic CT scan showed normal adrenal glands, and a cortisone challenge test and adrenocorticotropic hormone challenge test were normal. Electroencephalography showed diffuse background slow-waves.
  | Figure 1 Chest X-ray showing nodular lesions on both lungs consistent with miliary TB lesions. |
During the admission, the patient was disorientated in time and place, and experienced episodes of visual hallucination. The patient’s final diagnoses were delirium of hypoactive type (current) and anxiety disorder secondary to miliary TB (past). Different doses of risperidone were prescribed with the patient showing mild improvement at a dose of 1.5 mg. Eventually, the patient responded to antituberculosis treatment without any anxiety or depressive manifestations, but with residual paraplegia and dementia.
Discussion
To our knowledge, there are almost no published reports describing psychiatric symptoms caused by miliary TB (either alone or co-occurring with other medical symptoms); mental health workers may, therefore, not consider, and may consequently miss, this important diagnosis. Cognitive and behavioral changes have been described in a patient with brain tuberculomas resulting from miliary TB.20 Additionally, altered mental state has been reported in approximately one quarter of adult patients with miliary TB, most probably due to affection of brain or meninges.9,21 Several characteristics of this case suggest that the diagnosed anxiety disorder was due to miliary TB. However, we cannot exclude the possibility that generalized anxiety disorder preceded the onset of miliary TB or that both diseases were coincidental. The onset of anxiety symptoms in an older patient (64 years) is unusual, since anxiety disorders without medical causes usually present in a younger age group (35–40 years),16,18,19 and the lack of personal or family history of anxiety and lack of specific triggers favor an organic cause.16,18 The worsening of anxiety symptoms in the early morning and remission in the early evening is atypical of regular GAD.18,19,22 Furthermore, the relatively rapid progression of symptoms and lack of efficacy of several courses of different antianxiety medications further suggests that the organic cause was likely to be responsible. The disappearance of anxiety manifestations after clearance of miliary TB support the organic cause of the anxiety symptoms. The appearance of anxiety symptoms 3 years before the acute symptoms of miliary TB may represent a manifestation of a chronic course of miliary TB; given that, our patient complained of chronic fatigue during that period. Overt presentation of miliary TB with absent clinical and radiographic features has been described in 40% of patients with miliary TB.23 The cyclical nature of anxiety symptoms raised the possibility of adrenal involvement, which was investigated and ruled out by both CT scanning and cortisone and adrenocorticotropic hormone challenge tests. Other differential diagnoses in this case include anxiety secondary to symptoms related to benign prostatic hypertrophy, such as dribbling,24,25 which was ruled out as the onset of the urinary symptoms preceded anxiety onset by several years.
In conclusion, this case report serves as a reminder that organic causes for psychiatric symptoms always need to be considered, particularly if they follow an atypical pattern or fail to improve with usual psychiatric medications.
Acknowledgments
The authors would like to acknowledge the support from College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization. Global Tuberculosis Report 2012. Geneva: World Health Organization; 2012. Available from: http://apps.who.int/iris/bitstream/10665/75938/1/9789241564502_eng.pdf. Accessed April 15, 2013. | |
Abouzeid MS, Zumla AI, Felemban S, Alotaibi B, O’Grady J, Memish ZA. Tuberculosis trends in Saudis and non-Saudis in the Kingdom of Saudi Arabia – a 10 year retrospective study (2000–2009). PLoS One. 2012;7:e39478. | |
Abouzeid MS, Al RF, Memish ZA. Mortality among tuberculosis patients in Saudi Arabia (2001–2010). Ann Saudi Med. 2013;33:247–252. | |
Lawn SD, Zumla AI. Tuberculosis. Lancet. 2011;378:57–72. | |
Golden MP, Vikram HR. Extrapulmonary tuberculosis: an overview. Am Fam Physician. 2005;72:1761–1768. | |
Ray S, Talukdar A, Kundu S, Khanra D, Sonthalia N. Diagnosis and management of miliary tuberculosis: current state and future perspectives. Ther Clin Risk Manag. 2013;9:9–26. | |
Gurkan F, Bosnak M, Dikici B, et al. Miliary tuberculosis in children: a clinical review. Scand J Infect Dis. 1998;30:359–362. | |
Hamamoto Y, Koyama H, Hashihira M, Taniguchi T, Hashimoto K, Osako T. [Clinical studies on nine cases with miliary tuberculosis: serum level of tumor markers and bronchoscopy in differential diagnosis]. Kekkaku. 1994;69:681–687. Japanese. | |
Hussain SF, Irfan M, Abbasi M, et al. Clinical characteristics of 110 miliary tuberculosis patients from a low HIV prevalence country. Int J Tuberc Lung Dis. 2004;8:493–499. | |
Maartens G, Willcox PA, Benatar SR. Miliary tuberculosis: rapid diagnosis, hematologic abnormalities, and outcome in 109 treated adults. Am J Med. 1990;89:291–296. | |
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Press; 2013. | |
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325. | |
Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–2196. | |
Grant BF, Hasin DS, Stinson FS, et al. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2005;35:1747–1759. | |
Culpepper L. Generalized anxiety disorder and medical illness. J Clin Psychiatry. 2009;70 Suppl 2:20–24. | |
Hoge EA, Ivkovic A, Fricchione GL. Generalized anxiety disorder: diagnosis and treatment. BMJ. 2012;345:e7500. | |
Castillo CS, Schultz SK, Robinson RG. Clinical correlates of early-onset and late-onset poststroke generalized anxiety. Am J Psychiatry. 1995;152:1174–1179. | |
Fricchione G. Clinical practice. Generalized anxiety disorder. N Engl J Med. 2004;351:675–682. | |
Bandelow B, Boerner JR, Kasper S, Linden M, Wittchen HU, Möller HJ. The diagnosis and treatment of generalized anxiety disorder. Dtsch Arztebl Int. 2013;110:300–309; quiz 310. | |
Akritidis N, Galiatsou E, Kakadellis J, Dimas K, Paparounas K. Brain tuberculomas due to miliary tuberculosis. South Med J. 2005;98:111–113. | |
Ayatollahi J. Clinical manifestations and outcome of miliary tuberculosis. Acta Med Iran. 2004;42:432–436. | |
Wittchen HU, Hoyer J. Generalized anxiety disorder: nature and course. J Clin Psychiatry. 2001;62 Suppl 11:15–19; discussion 20–21. | |
Proudfoot AT, Akhtar AJ, Douglas AC, Horne NW. Miliary tuberculosis in adults. Br Med J. 1969;2:273–276. | |
Coyne KS, Kvasz M, Ireland AM, Milsom I, Kopp ZS, Chapple CR. Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the United Kingdom, and the United States. Eur Urol. 2012;61:88–95. | |
Bogner HR, Gallo JJ, Swartz KL, Ford DE. Anxiety disorders and disability secondary to urinary incontinence among adults over age 50. Int J Psychiatry Med. 2002;32:141–154. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.