Back to Journals » Nature and Science of Sleep » Volume 15
S-Ketamine Improves Slow Wave Sleep and the Associated Changes in Serum Protein Among Gynecological Abdominal Surgery Patients: A Randomized Controlled Trial
Authors Zhang T, Song N, Li S , Yu L , Xie Y, Yue Z, Zhang R, Wang L, Tan H
Received 24 August 2023
Accepted for publication 31 October 2023
Published 6 November 2023 Volume 2023:15 Pages 903—913
DOI https://doi.org/10.2147/NSS.S430453
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Valentina Alfonsi
Tianzhuo Zhang,1,2,* Nan Song,3,* Shuo Li,2,* Ling Yu,2 Yining Xie,2 Zhijie Yue,2 Rui Zhang,4 Lijie Wang,4 Hongyu Tan2
1Department of Gastroenterology, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, 100045, People’s Republic of China; 2Department of Anesthesiology, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Peking University Cancer Hospital & Institute, Beijing, 100142, People’s Republic of China; 3Department of Gynecology, Key laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Peking University Cancer Hospital & Institute, Beijing, 100142, People’s Republic of China; 4Philips (China) Investment Co., Ltd., Beijing, 100600, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hongyu Tan, Department of Anesthesiology, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Peking University Cancer Hospital & Institute, Beijing, 100142, People’s Republic of China, Tel +86-10-88196409, Email [email protected]
Purpose: This study aims to evaluate the effect of S-ketamine on slow wave sleep (SWS) and the related changes in serum protein in gynecological patients after open abdomen surgery.
Methods: This was a randomized controlled trial. One hundred gynecological patients undergoing open abdomen surgery were randomized into an S-ketamine group (group S) or placebo group (0.9% saline; group C). During operation, patients in group S received adjuvant S-ketamine infusion (0.2 mg·kg− 1·h− 1) while those in group C received 0.9% saline. All patients were connected to patient-controlled intravenous analgesia (PCIA) pump in the end of the surgery and the patients in group S with an additional S-ketamine in PCIA pump. Polysomnogram (PSG) was monitored during the next night after surgery with PCIA pump. Blood samples were collected for proteomic analysis at 6:00 AM after PSG monitoring. The primary outcome was the percentage of SWS (also known as stage 3 non-rapid eye movement sleep, stage N3) on the next night after surgery, and the secondary outcome was subjective sleep quality, pain scores, and the changes in serum proteomics.
Results: Complete polysomnogram recordings were obtained from 64 study participants (31 in group C and 33 in group S). The administration of S-ketamine infusion resulted in a significant increase in the percentage of SWS/N3 compared to the control group (group C, median (IQR [range]), 8.9 (6.3, 12.5); group S, median (IQR [range]), 15.6 (12.4, 18.8), P< 0.001). However, subjective evaluations of sleep quality revealed no significant variances between the two groups. The protein affected by S-ketamine was primarily associated with posttranslational modification, protein turnover, carbohydrate transport, and metabolism.
Conclusion: In patients undergoing open gynecological surgery, S-ketamine enhanced the percentage of objective sleep of SWS during the next night after surgery. Additionally, there were differences observed in serum protein levels between the two groups.
Trial Registration: ChiCTR2200055180. Registered on 02/01/2022.
Keywords: S-ketamine, slow wave sleep, serum proteomics, gynecologic surgery
Introduction
It is widely recognized that major abdominal surgeries can result in significant sleep disturbance. Various elements contribute to the quality of sleep following surgery, including the body’s response to surgical stress, the degree of pain experienced, the administration of sedatives and analgesics, the patient’s age and environmental factors such as noise levels.1 Postoperative sleep disorders (PSD) are characterized by alterations in the quality of sleep that occur post-surgery.2 Studies have used PSG to objectively measure sleep patterns in surgical patients and have revealed that patients who have undergone major surgeries experience lower sleep efficiency, disrupted sleep, decreased rapid eye movement (REM) sleep, and, in some cases, the absence of N3 sleep stage.3,4
Numerous studies have disclosed that a common pathway exists between physiological sleep and general anesthesia.5 Although opioids have been successful in managing postoperative pain, they can also disrupt sleep regulation and create sleep disturbances.6,7 Given this, ketamine has emerged as an effective multimodal analgesic treatment option that produces fewer side effects.8 As a non-competitive antagonist of the N-methyl-D-aspartate glutamate receptor (NMDAR), ketamine has not only demonstrated fast acting antidepressant properties but also shown to influence circadian rhythms.9 S-ketamine, also known as S(+)-enantiomers of ketamine, is twice as potent as ketamine for inducing a similar level of sedation10 and has received approval as an adjunctive treatment for major depression disorder.11
Ketamine has demonstrated the ability to enhance slow wave activity in both rats and individuals with major depressive disorder. The observed effect aligns with the levels of plasma brain-derived neurotrophic factor (BDNF).12 Ketamine, along with other general anesthetics like propofol, can activate a specific neuronal population in the hypothalamus, consisting of neuroendocrine cells, and subsequently increase slow-wave sleep (SWS).13 The antidepressant effects of ketamine are notable due to its capacity to block NMDARs on gamma-aminobutyric acid (GABA)-ergic interneurons.14 Furthermore, the metabolite of ketamine, hydroxynorketamine (HNK), is capable of activating postsynaptic α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptors (AMPARs), thereby influencing the molecular pathway involved in antidepressant actions.15,16
Given the known effect of ketamine on slow-wave sleep (SWS) and its potential anti-depressant properties via molecular mechanisms, the specific subanesthetic level of S-ketamine required to impact SWS in normal patients undergoing major open gynecological abdominal surgery remains unknown. To address this knowledge gap, our hypothesis was that a subanesthetic dose of S-ketamine could potentially improve SWS in these patients. The intervention involved the administration of additional S-ketamine during both the intraoperative and postoperative periods in group S. Accordingly, the primary outcome was the percentage of SWS on the next night after surgery and the secondary outcome was subjective sleep quality, pain scores, and the changes in serum proteomics.
Methods
Participants
The double-blind, prospective randomized controlled trial was conducted in our hospital in Beijing, China. The Institutional Review Board at Peking University Cancer Hospital’s Ethics Committee granted approval for this study, with reference to the assigned number 2021YJZ109, and all participants provided written informed consent before participating in the trial. Furthermore, the trial was registered ahead of patient enrollment with the Chinese Clinical Trial Registry, under the assigned number ChiCTR2200055180, with Hongyu Tan serving as the Principal Investigator and the registration date set for January 02, 2022. This article strictly adheres to relevant Consolidated Standards of Reporting Trials (CONSORT) guidelines.
From January 2022 to July 2022, eligible patients were identified and recruited at the Peking University Cancer Hospital if they (1) were aged 18–65 years, with body mass index (BMI, in kg·m−2) between 18 and 30, were diagnosed with gynecological cancers, and underwent elective open abdominal gynecological surgery, (2) were stratified by the American Society of Anesthesiologists (ASA) grade into I–II, (3) were expected to be hospitalized for over 4 days, and (4) had the operation finished before 20:00 of the day.
The eligible patients were subject to random assignment, in a 1:1 ratio, to either the S-ketamine group (group S) or placebo (0.9% saline) group (group C). A data manager who had no involvement in determining eligibility or assessment of outcomes performed the randomization using random number tables. An independent research nurse opened each patient’s envelope containing the random numbers only after completing the baseline assessment. Patients were excluded from the study with the following conditions: (1) refusal to participate in the study; (2) tumor recurrence; (3) multiple primary malignant tumors; (4) current and chronic use of analgesics, psychotropic medications, hormones, or non-steroidal anti-inflammatories; (5) a history of chronic pain, schizophrenia, epilepsy, dementia, obstructive sleep apnea syndrome and sleep disorders (requirement of hypnotics/sedatives during the last month); (6) a history of diabetes with uncontrolled hypertension or blood glucose; (7) hepatorenal dysfunction; (8) any contraindications to the anesthetic agents used during surgery; (9) diagnosis of depression. The enrolled patients’ age, BMI, ASA physical status, preoperative comorbidity, type of gynecological cancer, Pittsburgh Sleep Quality Index (PSQI)17 of the recent one-month sleep quality, and Richards-Campbell Sleep Questionnaire (RCSQ)18 of the night before surgery were recorded. The RCSQ evaluated the patient’s perceived sleep quality over six domains based on scores from 0 to 100, with 0 representing a negative perception of sleep and 100 indicating positive perception. The assessment of patients’ PSQI and RCSQ was carried out by a blinded study investigator, and none of the enrolled patients were being treated with drugs known to affect sleep.
Anesthetic and Analgesic Techniques
During the surgical procedure, patient monitoring was carried out using a range of techniques including electrocardiography, pulse oximetry, end-tidal carbon dioxide, invasive arterial pressure, urine output, and the bispectral index. To induce general anesthesia, patients were given intravenous administration of 2 mg·kg−1 of propofol, 0.4 μg·kg−1 of sufentanil, and a single dose of 0.2 mg·kg−1 cisatracurium to aid endotracheal intubation. Group C patients received general anesthesia administered through the inhalation of 1% sevoflurane and received intravenous doses of 2–4 ng·mL−1 (plasma concentration) remifentanil and 1–3 μg·mL−1 (plasma concentration) propofol to maintain anesthesia. In comparison, group S patients received the same general anesthesia doses as group C, with an additional target-controlled infusion (CP-600TCI; SLGO, Beijing, China) of 0.2 mg·kg−1·h−1 S-ketamine (Hengrui Medicine Co., Ltd., Jiangsu, China). The oxygen inhalation flow rate during the procedure was set to 50%, and the ventilator was adjusted to maintain end-tidal carbon dioxide between 35 and 45 mmHg. Sevoflurane and propofol levels were adjusted to maintain the bispectral index at a spectral entropy value of 40–60. The concentration of remifentanil was modified as required by hemodynamic changes. Towards the end of the surgery, patients were given 10 μg of intravenous sufentanil and 15 mg of ketorolac tromethamine, followed by 5 mg of tropisetron administered 15 minutes before concluding the surgical procedure.
S-ketamine was discontinued 30 minutes before the end of the surgery. Following the procedure, patients were linked to a PCIA pump that contained 120 mL of a 2 μg·kg−1 sufentanil solution, 90 mg of ketorolac tromethamine, and 20 mg of tropisetron in a 0.9% sodium chloride solution for group C. In group S, an additional 50 mg of S-ketamine was added. The PCIA pump was set to administer a 2 mL loading dose, a 1 mL·h−1 basal infusion, a 2 mL bolus dose with a lockout interval of 10 minutes, and a maximum dose of 13 mL·h−1. Post surgery, patients were initially transported to the post-anesthesia care unit, and after extubation, subsequently transferred to the ward. The amount of S-ketamine infusion during the operation, the overall intraoperative infusion, blood loss, total urine output, red blood cell transfusion necessity, and the duration of general anesthesia were all noted.
Polysomnographic Monitoring
Polysomnography was performed with a Philips Alice PDx EEG/PSG Recording device (Philips Respironics) from 19:30 PM to 5:30 AM during the next night following surgery. The polysomnogram comprised a two-channel electroencephalogram (C3, C4), a two-channel electrooculogram (E1, E2), a two-channel chin electromyogram (Chin1-Chin2) and a single channel for the grounding wire. Trained investigators (R.Z. and L.W.) were responsible for placing the electrodes on the patients. Sleep architecture was scored manually on an epoch-by-epoch basis and processed with SleepG3 software version 4.0.1.0 (Philips Respironics) by a qualified sleep physician (R.Z.) who was independent of the research process. In addition to these measures, we recorded the percentages of non-rapid eye movement (including N1, N2, and N3 stages), REM, total sleep time, and sleep efficiency for each patient.
Other Postoperative Data Collection
The subjective sleep quality of surgery tonight and next night was measured by the RCSQ and assessed by an independent investigator. The daytime sleep after surgery was recorded with HUAWEI band 6 (equipped with HUAWEI TruSleep™ 2.0 sleep monitoring algorithm, Huawei Technologies Co., Ltd., Shenzhen, China).
Postoperative pain at rest was assessed using the Visual Analogue Scale (VAS, ranging from 0 to 10, 0 = no pain, 10 = the worst imaginable pain). To achieve a VAS score ≤3 before discharge from the post-anesthesia care unit, patients were administered 0.1 μg·kg−1 of sufentanil by an anesthesiologist. If the VAS score was >3, repeated doses of 0.1 μg·kg−1 sufentanil were administered at intervals no less than 15 minutes until the VAS score was ≤3. Postoperative visits were made by a nurse anesthetist who was not involved in the research process. If the VAS score was >3, the surgeon provided additional analgesic drugs, primarily intravenous morphine. We recorded the S-ketamine consumption, VAS scores at 24 h and 48 h after surgery, the additional analgesic drug requirements, and sufentanil consumption of the PCIA in the initial 24 h postoperatively, starting from the patient’s discharge from the post-anesthesia care unit. Any untoward events such as dizziness, nausea, and vomiting were documented.
Quantitative Proteomics by Multiplexed Tandem Mass Tag (TMT) MS
As the cost for serum proteomics was considered, 20 samples were submitted to the laboratory for analysis, a top 10 and bottom 10 score of N3 percentage in the group S and group C were selected. The baseline of clinical characteristics of 20 patients was in Supplementary Tables 1–4. Serum samples were collected at 6:00 AM following sleep monitoring. Proteins were extracted from 100 μL of serum and high-abundance protein was digested with trypsin and labelled with TMT reagents. The pooled peptides were separated into 15 fractions using a C18 column (Waters BEH C18 4.6 × 250 mm, 5 µm) on a Rigol L3000 HPLC.
Sample Size
In our initial trial, we observed that the percentage of N3 on the next night after surgery in patients who did not receive S-ketamine was 2.3%, whereas those who accepted supplementary use of S-ketamine had a percentage of N3 at 23% on the next night after surgery. We utilized the PASS 15 power analysis and sample size software (NCSS, LCC, Kaysville, Utah, USA, ncss.com/software/pass.) to derive our sample size. We specifically employed the “proportions-two independent proportions-test (inequality)-test for two proportions” to compute the number of patients required per group for 80% power to detect the difference, with a two-tailed significance level of 0.05. Accordingly, we calculated a sample size of 40 patients per group, considering a dropout rate of about 20%, we intended to enroll 50 patients in each group.
Statistical Analysis
All statistical analyses were conducted using SPSS version 20.0 software (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.). Continuous variables with normal distribution were presented as mean ± standard deviation (SD). Non-normal variables were presented as median (interquartile range). Categorical data were expressed as percentages (%). Continuous variables were analyzed using the independent-sample t-test or the Mann–Whitney U-test, with the differences expressed as 95% confidence interval (CI). Categorical variables were analyzed using the χ2 test. The level of statistical significance was set at a two-sided P value of <0.05.
Results
From January to July 2022, a total of 100 patients were initially enrolled. By the end of the study period, 36 patients dropped out of the study. Among these patients, 3 were excluded due to a change of the operative mode during operation, 2 patients had blood pressure higher than 180/100 mm Hg upon entering the operating room, polysomnographic monitoring failed in 22 patients because of electrode detachment or refused to wear the electroencephalogram (EEG) monitor (11 patients in each group), and 5 patients in group C and 4 patients in group S with PCIA pump failure due to serious side effects within the first 24 h following the operation. A final of 64 patients were included in the present study analysis. The CONSORT diagram is shown in Figure 1.
 |
Figure 1 CONSORT flow diagram. CONSORT indicates Consolidated Standards of Reporting Trials. Abbreviation: PCIA, patient-controlled intravenous analgesia. |
Sixty-four patients aged 53.9 ± 5.1 years (range, 43–65) with BMI of 25.2 ± 3.2 (range, 19.1–30.0) had gynecologic cancer and preferred open abdominal surgery were included in this study. The RCSQ of the night before surgery and self-reported sleep quality over the past month using the PSQI of group S had no significant difference from group C, the demographic data between the two groups were no statistically significant differences (Table 1).
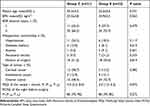 |
Table 1 Patient Demographics and Perioperative Characteristics |
Intraoperative and anesthetic data are shown in Table 2. The dose of S-ketamine in group S during the operation was 35.0 ± 15.0 mg (range, 13.8–73.2 mg). No statistically significant differences were observed between groups for intraoperative infusion (crystalloids and colloids), red blood transfusion, intraoperative blood loss, intraoperative urine output, or general anesthesia time.
 |
Table 2 Intraoperative Characteristics |
The consumption of S-ketamine in group S on the next night following surgery was 21.7 ± 7.4 mg (range, 8.7–37.1 mg). A significant difference was observed between the two groups that S-ketamine improved patients’ objective sleep quality of SWS (N3 stage, P<0.001, Table 3, Figure 2A), the percentage of stage N3 sleep increased from media 8.9% (IQR [range], [6.3–12.5]) in group C to 15.6% (IQR [range], [12.4–18.8]) in group S (95% CI, 4.0 to 8.5) on the next night following surgery. Total sleep time and sleep efficiency in group S were slightly higher than in group C, while there was no significant difference between the two groups. Other fragments of sleep structure such as N1, N2, and REM sleep were not significantly different between the two groups. The RCSQ subjective sleep quality score of the surgery tonight did not differ between the two groups, and the RCSQ of the next night of surgery in both groups were better than the surgery tonight.
 |
Table 3 Postoperative Variables |
Median (IQR [range]) pain scores were significant difference between the two groups, 4 (3–4.5 [0–10]) for the group C and 3 (2–4 [0–10]) for the group S after postoperative 24 h (P = 0.015). The pain score decreased after surgery 48 h for both groups with no difference (Table 3). The additional requirement of analgesic drugs after surgery (P>0.999) was not different between the two groups.
The incidences of adverse events and other complications after surgery 24 h were not statistically different between the two groups (Table 4). A total of 28 (43.7%) patients had dizziness, nausea, vomiting, or flatulence/bloating adverse events in this study, 13 (41.9%) of which were in group C, and 15 (45.4%) were in group S. No patient experienced respiratory depression, postoperative delirium, oliguria, or emergence agitation in this study.
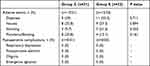 |
Table 4 Adverse Events and Postoperative Complications |
We then arranged the percentage of SWS stage in 64 patients in descending order. Our findings were intriguing as the top 10 patients exhibiting the highest levels of SWS belonged to group S, while the bottom 10 patients with the least levels of SWS were from group C (Supplementary Table 3). This outcome accentuates the potentiation of the adjuvant S-ketamine effect on SWS.
We sought to investigate the molecular mechanisms present in serum that may be responsible for the enhanced slow wave effects. Through the label-free proteomics platform, a total of 991 proteins were obtained from all serum samples based on filter criteria (Additional File 1). The majority of these proteins were found to be involved in posttranslational modification, protein turn over, carbohydrate transport, and metabolism (Figure 2B). Gene Ontology analysis revealed that these proteins were mainly located in the extracellular region and were involved in calcium ion binding and proteolysis (Figure 2C). A total of 55 proteins exhibited significant difference between the groups (|fold change|>1.5 and P<0.05, Additional File 2). Compared to the group C, 36 proteins were up-regulated (partly shown in Table 5), and 19 proteins were down-regulated in the group S (Figure 2D, Additional Files 3 and 4). Based on the findings of our hierarchical clustering analysis, we can observe a notable distinction between the control and S-ketamine groups as a result of the differential expression of proteins (Figure 2E).
 |
Table 5 Different Proteins Upregulated in Top 10 Level of SWS Group and the Bottom 10 Level of SWS Group Patients |
Discussion
According to the results of the randomized controlled trial conducted during open gynecological surgery, implementation of a PCIA pump after surgery coupled with administration of S-ketamine demonstrated a significant improvement in postoperative sleep quality. The research uncovered patients in the S-ketamine group displayed augmentations in SWS (N3 stage) as compared to the control group on the ensuing night following surgery.
Thus far, numerous studies utilized PSG to evaluate the objective sleep quality of patients in the intensive care unit.19–21 PSG monitoring in hospitalized regular-care ward has less reported. The preliminary research indicated that various factors such as pain, nursing interventions, and the noise produced by medical devices may have contributed to compromised sleep quality among patients on the night following surgery.22 Previous reports have revealed that postoperative pain has a greater impact on females,23 and gynecological surgeries are associated with an elevated risk of postoperative nausea and vomiting.24 Although the percentage of such adverse events did not significantly differ between the two groups in our trial, the total percentage of such events on the night of surgery was 43.7% (Table 4). Notably, the median score of RCSQ of the surgery tonight in both groups was only 60 (100 for the total). These factors contributed to lower patient compliance with PSG monitoring in general wards on the surgery night, so we set the primary outcome as the percentage of SWS (N3 stage) on the next night post-surgery.
Previous studies showed that patients undergoing gynecological surgery occur PSD frequently.25 In our trial, we used PSQI and RCSQ to assess the sleep quality of patients in recent month and the night before surgery, to make sure our participants have no sleep disorders and “first night effect”. During the next night after surgery, the objective sleep measures of SWS are significantly enhanced in group S, and the other sleep measures of total sleep time and sleep efficiency in group S were slightly higher than in group C but no significant difference between the two groups. However, the subjective sleep measure of RCSQ in both groups was no significant difference. Some studies have discussed the relationship between subjective and objective sleep quality, because “sleep quality” may characterize some aspects of sleep experience not currently understood,26,27 the inconsistency of our results is reasonable.
Ketamine functions as an NMDA receptor antagonist, low-dose perioperative ketamine may reduce chronic postsurgical pain after surgical procedures.28 S-ketamine has approximately two times more effective than the racemic mixture of ketamine and gets increasing use in worldwide.10 The surgical scopes of the patients enrolled in our study exhibit minimal variance, and our study’s findings indicated that the use of S-ketamine resulted in a significant reduction of the VAS score 24 h after the surgical procedure, but the VAS score 48 h following surgery was slightly lower in group S with no difference. The addition of S-ketamine contributed meaningfully to the efficacy of pain mitigation of acute pain postoperatively in our study. Furthermore, it should be noted that the enhanced proportion of SWS observed in patients treated with S-ketamine was not influenced by analgesia. This conclusion is supported by the fact that the PSG monitoring was conducted 48 hours postoperatively, and there was no discernible difference in pain scores between the two groups.
Early studies have shown that the administration of ketamine could enhance the SWS in major depressive disorder patients, correlated with changes in the level of BDNF in plasma.12 It is thought that ketamine’s antidepressant properties may from the activation of AMPA-mediated mTOR stimulation.15,16,29 In general anesthetics, ketamine has been demonstrated to activate a hypothalamic neuronal population consisting of neuroendocrine cells, resulting in an increase in slow-wave sleep.13 In our study, group S contained the top 10 patients who evidenced the highest levels of SWS, while group C accounted for the bottom 10 patients who exhibited the lowest levels of SWS. Based on the above theoretical foundation, we propose that the peripheral markers related to the improved SWS would also change after S-ketamine infusion in gynecological abdominal surgery patients, and these 20 samples were sent to the laboratory for testing.
No significant variations were observed in serum biochemical measures, such as C-reactive protein levels among samples. Our serum proteomics analysis revealed that alterations in proteins in the top 10 SWS level patients treated with S-ketamine were primarily related to posttranslational modification, protein turnover, carbohydrate transport and metabolism (Figure 2B and C). The upregulated proteins in the top 10 SWS level patients compared with the bottom 10 were identified as Ceruloplasmin, which activity is related to neurodegenerative diseases;30 CSF1R, the colony-stimulating factor 1 receptor, which plays important roles in the neuropathic pain and tumor immunology,31,32 had drawn our attention to further investigate the relationship among the S-ketamine, SWS, and these proteins in the molecular level.
BDNF was not detected in the top 10 SWS level patients in our data, one possible reason is that, compared with the ketamine used in major depressive disorder patient, the ketamine i.v. infusion was 0.5 mg·kg−1 over the course of 40 minutes and the serum was detected within 230 minutes,12 while our serum samples were obtained from the next morning following PSG monitoring in our trial. The different dosage and time of sample collection may lead to the different outcomes.
This study has some limitations. First, this trial was conducted in a single center, and further research of multiple centers for different surgery patients is needed. Second, we only used subjective sleep measures of PSQI and RCSQ to limit sleep disorder before surgery, objective sleep measure of PSG is recommended during the night before surgery in further study. Third, the sample size calculation suggested that 40 samples per group were needed; however, due to the complexity of PSG, final data to be completely analyzed were less than we expected, the statistical power of the main comparison (N3 proportion) with one-sided hypothesis was 82.9%, and higher numbers of enrolled patients are required to adequately verify this conclusion. Considering the cost of serum proteomic analysis, only 20 samples were tested for proteomics, the sample size of serum analysis was lower. This may cause some bias in the analysis of the alteration in serum protein, and more samples should be included in future studies.
In conclusion, our study showed that in the gynecological abdominal surgery patients, SWS was improved during the next night after surgery under S-ketamine treatment, and the adjuvant use of S-ketamine caused an alteration in serum protein.
Data Sharing Statement
The datasets generated during the current study are available in the ProteomeXchange Consortium (http://proteomecentral.proteomexchange.org) via the iProX partner repository with the dataset identifier PXD040679 (https://www.iprox.cn/page/project.html?id=IPX0006049000).
Acknowledgments
We thank the anesthetists and gynecologists for collaboration in the surgery. We acknowledge Novogene (Beijing, China) for proteomics technical support.
Funding
This work was supported by Beijing Municipal Science & Technology Commission No. Z221110007422031.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Rosenberg-Adamsen S, Kehlet H, Dodds C, Rosenberg J. Postoperative sleep disturbances: mechanisms and clinical implications. Br J Anaesth. 1996;76(4):552–559. doi:10.1093/bja/76.4.552
2. Rosenberg J. Sleep disturbances after non-cardiac surgery. Sleep Med Rev. 2001;5(2):129–137. doi:10.1053/smrv.2000.0121
3. Gögenur I, Wildschiøtz G, Rosenberg J. Circadian distribution of sleep phases after major abdominal surgery. Br J Anaesth. 2008;100(1):45–49. doi:10.1093/bja/aem340
4. Edéll-Gustafsson UM, Hetta JE, Arén CB. Sleep and quality of life assessment in patients undergoing coronary artery bypass grafting. J Adv Nurs. 1999;29(5):1213–1220. doi:10.1046/j.1365-2648.1999.01006.x
5. Franks NP. General anaesthesia: from molecular targets to neuronal pathways of sleep and arousal. Nat Rev Neurosci. 2008;9(5):370–386. doi:10.1038/nrn2372
6. Cronin A, Keifer JC, Baghdoyan HA, Lydic R. Opioid inhibition of rapid eye movement sleep by a specific mu receptor agonist. Br J Anaesth. 1995;74(2):188–192. doi:10.1093/bja/74.2.188
7. Keifer JC, Baghdoyan HA, Lydic R. Sleep disruption and increased apneas after pontine microinjection of morphine. Anesthesiology. 1992;77(5):973–982. doi:10.1097/00000542-199211000-00021
8. Himmelseher S, Durieux ME, Weiskopf R. Ketamine for perioperative pain management. Anesthesiology. 2005;102(1):211–220. doi:10.1097/00000542-200501000-00030
9. Kohtala S, Alitalo O, Rosenholm M, Rozov S, Rantamäki T. Time is of the essence: coupling sleep-wake and circadian neurobiology to the antidepressant effects of ketamine. Pharmacol Ther. 2021;221:107741. doi:10.1016/j.pharmthera.2020.107741
10. Peltoniemi MA, Hagelberg NM, Olkkola KT, Saari TI. Ketamine: a review of clinical pharmacokinetics and pharmacodynamics in anesthesia and pain therapy. Clin Pharmacokinet. 2016;55(9):1059–1077. doi:10.1007/s40262-016-0383-6
11. Kim J, Farchione T, Potter A, Chen Q, Temple R. Esketamine for treatment-resistant depression - first FDA-approved antidepressant in a new class. N Engl J Med. 2019;381(1):1–4. doi:10.1056/NEJMp1903305
12. Duncan WC, Sarasso S, Ferrarelli F, et al. Concomitant BDNF and sleep slow wave changes indicate ketamine-induced plasticity in major depressive disorder. Int J Neuropsychopharmacol. 2013;16(2):301–311. doi:10.1017/S1461145712000545
13. Jiang-Xie LF, Yin L, Zhao S, et al. A common neuroendocrine substrate for diverse general anesthetics and sleep. Neuron. 2019;102(5):1053–65.e4. doi:10.1016/j.neuron.2019.03.033
14. Abdallah CG, Sanacora G, Duman RS, Krystal JH. The neurobiology of depression, ketamine and rapid-acting antidepressants: is it glutamate inhibition or activation? Pharmacol Ther. 2018;190:148–158. doi:10.1016/j.pharmthera.2018.05.010
15. Koike H, Iijima M, Chaki S. Involvement of AMPA receptor in both the rapid and sustained antidepressant-like effects of ketamine in animal models of depression. Behav Brain Res. 2011;224(1):107–111. doi:10.1016/j.bbr.2011.05.035
16. Li N, Lee B, Liu RJ, et al. mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science. 2010;329(5994):959–964. doi:10.1126/science.1190287
17. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
18. Kamdar BB, Shah PA, King LM, et al. Patient-nurse interrater reliability and agreement of the Richards-Campbell sleep questionnaire. Am J Crit Care. 2012;21(4):261–269. doi:10.4037/ajcc2012111
19. Elliott R, McKinley S, Cistulli P, Fien M. Characterisation of sleep in intensive care using 24-hour polysomnography: an observational study. Crit Care. 2013;17(2):R46. doi:10.1186/cc12565
20. Wu XH, Cui F, Zhang C, et al. Low-dose dexmedetomidine improves sleep quality pattern in elderly patients after noncardiac surgery in the intensive care unit: a pilot randomized controlled trial. Anesthesiology. 2016;125(5):979–991. doi:10.1097/ALN.0000000000001325
21. Aurell J, Elmqvist D. Sleep in the surgical intensive care unit: continuous polygraphic recording of sleep in nine patients receiving postoperative care. Br Med J. 1985;290(6474):1029–1032. doi:10.1136/bmj.290.6474.1029
22. Wesselius HM, van den Ende ES, Alsma J, et al. Quality and quantity of sleep and factors associated with sleep disturbance in hospitalized patients. JAMA Intern Med. 2018;178(9):1201–1208. doi:10.1001/jamainternmed.2018.2669
23. Yang MMH, Hartley RL, Leung AA, et al. Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis. BMJ Open. 2019;9(4):e025091. doi:10.1136/bmjopen-2018-025091
24. Apfel CC, Heidrich FM, Jukar-Rao S, et al. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth. 2012;109(5):742–753. doi:10.1093/bja/aes276
25. Duan G, Wang K, Peng T, Wu Z, Li H. The effects of intraoperative dexmedetomidine use and its different dose on postoperative sleep disturbance in patients who have undergone non-cardiac major surgery: a real-world cohort study. Nat Sci Sleep. 2020;12:209–219. doi:10.2147/NSS.S239706
26. Krystal AD, Edinger JD. Measuring sleep quality. Sleep Med. 2008;9(Suppl 1):S10–S17. doi:10.1016/S1389-9457(08)70011-X
27. Van Den Berg JF, Van Rooij FJ, Vos H, et al. Disagreement between subjective and actigraphic measures of sleep duration in a population-based study of elderly persons. J Sleep Res. 2008;17(3):295–302. doi:10.1111/j.1365-2869.2008.00638.x
28. Zhang T, Yue Z, Yu L, et al. S-ketamine promotes postoperative recovery of gastrointestinal function and reduces postoperative pain in gynecological abdominal surgery patients: a randomized controlled trial. BMC Surg. 2023;23(1):74. doi:10.1186/s12893-023-01973-0
29. Ignácio ZM, Réus GZ, Arent CO, Abelaira HM, Pitcher MR, Quevedo J. New perspectives on the involvement of mTOR in depression as well as in the action of antidepressant drugs. Br J Clin Pharmacol. 2016;82(5):1280–1290. doi:10.1111/bcp.12845
30. Zanardi A, Conti A, Cremonesi M, et al. Ceruloplasmin replacement therapy ameliorates neurological symptoms in a preclinical model of aceruloplasminemia. EMBO Mol Med. 2018;10(1):91–106. doi:10.15252/emmm.201708361
31. Xu C, Zheng H, Liu T, Zhang Y, Feng Y. Bioinformatics analysis identifies CSF1R as an essential gene mediating neuropathic pain - experimental research. Int J Surg. 2021;95:106140. doi:10.1016/j.ijsu.2021.106140
32. Yeung J, Yaghoobi V, Miyagishima D, et al. Targeting the CSF1/CSF1R axis is a potential treatment strategy for malignant meningiomas. Neuro Oncol. 2021;23(11):1922–1935. doi:10.1093/neuonc/noab075
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

