Back to Journals » Clinical Ophthalmology » Volume 13
Wide-angled endoillumination vs traditional scleral buckling surgery for retinal detachment – a comparative study
Authors Cohen E , Rosenblatt A, Bornstein S, Loewenstein A , Barak A, Schwartz S
Received 5 August 2018
Accepted for publication 9 October 2018
Published 8 February 2019 Volume 2019:13 Pages 287—293
DOI https://doi.org/10.2147/OPTH.S182751
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Eyal Cohen,1,2 Amir Rosenblatt,1,2 Sandy Bornstein,2 Anat Loewenstein,1,2 Adiel Barak,1,2 Shulamit Schwartz1,2
1Department of Ophthalmology, Tel Aviv Sourasky Medical Center, Tel Aviv, Israel; 2Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
Purpose: To evaluate the surgical outcomes of traditional scleral buckling (TSB) compared to chandelier-assisted scleral buckling (CSB) for rhegmatogenous retinal detachment repair.
Patients and methods: A retrospective interventional comparative case series of 49 eyes that underwent SB procedure. Medical records of 27 and 22 eyes that underwent TSB and CSB surgery, respectively, were evaluated. Outcome measures included primary anatomical success, visual acuity (VA), and perioperative complications.
Results: Primary reattachment rate was similar with 85.2% in the TCB group and 81.8% in the CSB group (P=1.00); eight patients needed one additional operation or gas injection with a final reattachment rate of 100% at 6 months. Mean VA in the CSB group improved from 20/60 at presentation to 20/35, 6 months postoperatively. In the TSB group, VA improved from 20/80 to 20/45 (P=0.90). Among the eyes that were successfully reattached with either SB approach, two eyes in each group had cataract progression and none of them required surgery during follow-up. No cases of endophthalmitis were observed.
Conclusion: CSB is a modified technique with an advantage of superior visualization compared with the traditional surgery, which simplifies the operation, enhance competency, and could be used as a valuable educational tool. It can provide similar anatomical and functional outcomes with no additional perioperative complications.
Keywords: chandelier, endoillumination, retinal detachment, scleral buckle, wide-angled viewing system
Introduction
Scleral buckling (SB) surgery was first described by Custodis,1 Schepens,3 and Arruga2 in1950 and since then became a well-known technique for the treatment of rhegmatogenous retinal detachment (RRD). Numerous studies have already addressed the comparison between SB and pars plana vitrectomy (PPV) for the treatment of RRD with comparable results. Yet, over the recent years, there has been growing abandonment of SB procedures among retina specialists, with preference toward PPV. One of the leading causes for this trend is the wide-angled viewing systems combined with new illumination tools that enable surgeons to get excellent retinal viewing (around 100°–115°, depending on system used) and easy and quick localization of all peripheral retinal tears.4
Traditional SB (TSB) procedure, however, has remained unchanged over the years, using indirect ophthalmoscopy as the main source of retinal viewing. When using indirect ophthalmoscopy together with condensing lens, the +20 D condensing lens offers 3× magnification and a field of view of approximately 45°. A +30 D lens will offer 2× magnification along with a field of approximately 65°. The small field of view and expertise in usage require a high level of technical skills, a substantial learning curve, and experience. Retinal surgeons worldwide are becoming less skilled in performing indirect ophthalmoscopy, and today, most use slit lamp with noncontact wide-angle lenses. The decline in standard use of indirect ophthalmoscopy makes using it during surgery especially difficult, and most surgeons will prefer performing a procedure with wide-angle viewing system, which they are comfortable with.
In TSB surgery, an intraoperative indirect ophthalmoscope is being used to accomplish two main principals of the surgery: to identify all retinal tears and to create a chorioretinal scar around them with transscleral cryopexy. Since the success of the SB procedure relies, among others, on the identification of all breaks, there has been a recent tendency toward improving visualization in this procedure too. Several studies have already presented a modification of the traditional technique, using an intraoperative wide-angled viewing system together with chandelier illumination. Concerns were raised regarding the safety of the procedure in terms of cataract formation and endophthalmitis as well as reattachment rates. These issues were not fully addressed in the literature yet.
The aim of our study was to compare the outcomes of chandelier-assisted SB (CSB) surgery to the TSB surgery.
Methods
Study design
This is a retrospective interventional comparative case series of patients who underwent an SB procedure for RRD by three senior retina specialists between January 2011 and November 2015 in Tel Aviv Medical Center, Tel Aviv, Israel. Thirty-one consecutive patients underwent a TSB procedure between January 2011 and October 2013, and 22 consecutive patients underwent a CSB procedure between November 2013 and November 2015. The medical charts of the two groups were retrospectively compared. Data collection included patients’ demographics, comprehensive eye examination, and intra- and postoperative complications and risk factors.
The study was conducted in accordance with the tenets set forth in the Declaration of Helsinki, and all necessary authorizations were obtained from the Tel Aviv medical center Institutional Review Board. Patients’ informed consent was not required by the institutional review board as this is a retrospective study and patient data were kept confidential by using only deidentified data.
Preoperative and postoperative evaluations
All patients underwent a preoperative evaluation including a detailed ocular history, best corrected visual acuity (BCVA) measurements, a slit-lamp examination, and an intraocular pressure measurement with a Goldmann applanation tonometry. A comprehensive fundus examination was performed using a three-mirror lens and an indirect ophthalmoscope. A fundus drawing was made describing RD extension, number of break(s) and their location, macula status (on/off), and proliferative vitreoretinopathy grading.
None of the patients had risk factors such as trauma, giant retinal tear, or proliferative vitreoretinopathy grade C.
Postoperative evaluation was conducted by a retina specialist at 1, 7, and 30 days and 3 and 6 months post operation. Visits included BCVA, slit-lamp examination, and ophthalmoscopic findings. All patients completed at least 6 months of follow-up.
Surgical technique: traditional SB
With the patient under general or retrobulbar anesthesia, a conjunctival peritomy was performed and four rectus muscles were hooked and isolated on a 2–0 silk suture, after which the break(s) was localized using an indirect ophthalmoscope. Transscleral cryopexy was performed at the site of the break(s) under indirect visualization. The anterior and posterior edges of the break were marked, and the distance from the muscle insertion to the posterior extent of the break was measured using a caliper. According to physician discretion, a segmental or circumferential encircling buckle consisting of a silicone tire or sponge was sutured to the sclera with 5–0 Mersilene mattress sutures. External subretinal fluid drainage was performed upon physician discretion using a diamond blade sclerotomy and a 30-gage needle. The buckle sutures were closed after a final assessment of the buckle height and apposition of the retinal breaks. The conjunctiva was then closed with 7–0 Vicryl sutures.
Surgical technique: wide-angled endoillumination SB
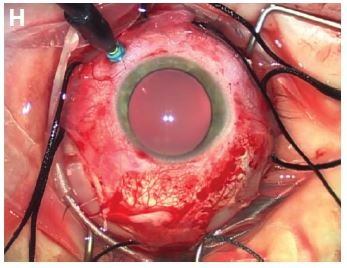
This procedure was done similar to the traditional approach except that the retina was visualized with a wide-angle viewing system (BIOM, Port St. Lucie, FL, USA) along with a chandelier 25-gage light source (Alcon, Fort Worth, TX, USA) as a replacement for the standard indirect ophthalmoscope. As shown in Figure 1, the chandelier light was placed 3.5 mm posterior to the limbus at the superotemporal quadrant after rectus muscle localization. BIOM viewing system using Wide Field High Definition Lens was mounted on a 844 Zeiss microscope (Carl Zeiss Meditec AG, Jena, Germany). After a comprehensive examination of the retina, location of the break(s), and a cryopexy procedure, the chandelier light source was removed and the cannula was closed with a scleral plug during the placement of scleral sutures, buckle insertion, and subretinal fluid drainage, if needed. The light source was reintroduced for a final assessment of the buckle height and apposition of the retinal breaks. The sclerotomy was sutured with a 7–0 Vicryl suture if there was any leak.
We did not use an intravitreal gas injection in any of the cases.
Outcome measures
Main outcome was the primary reattachment rate in the two groups after one procedure. Secondary outcomes were final BCVA and intra- and postoperative complications including cataract formation and endophthalmitis.
Statistical analyses
The data were recorded in Microsoft Excel and analyzed using SPSS version 21 (IBM Corporation, Armonk, NY, USA). VA was measured in decimal and converted to logarithm of the minimum angle of resolution (Log MAR) for statistical purposes. Continuous variables, such as VA, are presented as mean and SD, and nominal variables, such as gender and laterality, are presented as number and respective percentage. Continuous variables, such as VA, were compared within subjects by means of the Wilcoxon nonparametric test for paired comparisons. Between-subjects comparison of continuous variables was performed by the Mann–Whitney nonparametric test. Binary and nominal variables were compared between subjects using the Pearson’s chi-square or Fisher’s exact test. All tests were two-tailed, and the threshold for statistical significance was set at a P-value ≤0.05.
Results
Patients’ baseline characteristics
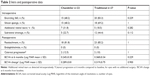
A total of 53 SB procedures were performed in the ophthalmology department at Tel Aviv Medical Center between 2011 and 2015. Of them, 49 eyes of 47 patients were included in the study: 27 eyes in the TSB group and 22 eyes in the CSB group. Four patients who were lost from follow-up were excluded. There were 27 eyes of female patients (55.1%) with a mean age of 42.24±16.9 years (range, 5–77) and a mean follow-up duration of 22.29±19.7 months (range, 6–70 months). The right eye was involved in 55.1% of the cases. Thirty-six eyes had a preoperatively documented myopia with a mean sphere of 5.5±2.9 D (range 1.00–13.0 D). The macula was involved in 32 (65.3%) eyes. The median VA at presentation was 20/40 (range from 20/20 to hand motion). Only two (4.1%) eyes were pseudophakic, and the rest were phakic. Table 1 summarizes patients’ baseline characteristics for the two groups. Multiple retinal tears (more than one) were found preoperatively in 12 eyes (54.5%) in the CSB group and in 8 eyes (29.6%) in the TSB group. The SB procedure was the first treatment of choice in 19 eyes (86.4%) in the CSB group and in 21 eyes (77.8%) in the TCB group (P=0.488). Pneumatic retinopexy with cryopexy prior to SB was done in three eyes (16.3%) in the CSB group and in five eyes (18.5%) in the TCB group (P=0.715).
Intraoperative data
An encircling 360° buckle was used in 15 eyes (68.2%) in the CSB group and in 20 eyes (83.8%) in the TCB group (P=0.229). A silicon sponge (Geuder AG, Heidelberg, Germany) was the most prevalent type of implant used in both groups: specifically, it was used in 15 CSB eyes (68.2%) and in 18 TCB eyes (69.2%; P=1.00). External subretinal drainage was performed in 5 CSB eyes (22.7%) and in 12 TCB eyes (44.4%; P=0.112).
Additional retinal tears not detected during presurgical evaluations were found during the operation in 5 of 27 eyes (18.5%) in the TSB group compared to 7 of 22 eyes (31.8%) in the CSB group. This represents a difference of 71.9% in the rate of intraoperative additional tears recognition. There was one case of an intraoperative complication in the CSB group. The patient had a subretinal hemorrhage during fluid drainage that was absorbed completely without intervention during the first month of follow-up.
Postoperative outcomes
The overall reattachment rate was similar between the two groups: 81.8% (18 of 22 eyes) in the CSB group and 85.2% (23 of 27 eyes) in the TCB group (P=1.00). Four eyes in each group failed to attach. Three eyes in each group underwent PPV with successful reattachment after one surgery and one eye in each group underwent a supplemental intravitreal gas injection that was sufficient for retinal reattachment. Overall, we had a 100% reattachment rate during the follow-up period. Table 2 summarizes intra- and postoperative outcomes.
The differences in VA between the two study groups were not statistically significant in all measured time points throughout follow-up (1, 3, and 6 months postoperatively) as shown in Table 3.
At 6 months, the mean BCVA measured in Log MAR was 0.245 in the CSB group and 0.368 in the TSB group (P=0.229), which represented a mean improvement in VA in Log MAR of 0.289 in the CSB group and 0.319 in the TSB group (P=0.900).
Among the eyes that were successfully reattached with either SB approach, cataract progression was observed in four eyes only. Two patients from the CSB group were with a nuclear cataract progression without any component that might suggest contact with the lens during surgery, one of them with a visually significant cataract progression and a decline in VA from 20/30 to 20/50 during follow-up. Two patients from the TSB group had cataract progression that did not become visually significant. None of those patients required cataract extraction surgery during the first 6 months of follow-up. The six patients who underwent PPV had their cataract removed either at the operation itself or later on in a separate surgery for further visual improvement.
There were no cases of endophthalmitis in either group.
Discussion
Scleral buckle technique possesses some clear advantage over vitrectomy by being an extraocular surgery and a preferred technique for young phakic patients.5 A comparison of the SB vs primary vitrectomy in RRD study (SPR) showed in the subgroup analysis that phakic patients had better visual outcomes, less cataract progression, and needed fewer retina-affecting procedures in the SB group compared with the vitrectomy group.6 The study confirms that SB still has its place in the vitreo-retinal (VR) surgeon’s repertoire for the correction of RRD, and that the knowledge and skills needed for doing it have to be preserved. Despite its clear advantages, a significant and progressive decline in the utilization of this procedure for RD repair is seen in the last years. In the ASRS Pat survey, answering the question: What is your usual recommendation for a pseudophakic superior RD, macula-on, −3.00 myope, single tear? Around 30% of physicians preferred SB in 2012, yet only around 3%–4% preferred SB in 2017 (https://www.asrs.org/content/documents/_2017-pat-survey-trending-data-for-website.pdf). The shift away from SB can be explained by a number of factors that contribute to the inevitable preference of VR surgeons toward vitrectomy including, the complications associated with SB surgery such as strabismus and increased axial length, longer operation time, and a longer learning curve for the SB surgery, as well as the tremendous progress in PPV instrumentation and visualization. Still, visualization with the indirect ophthalmoscope appears to be a key factor in the abandonment of SB compared with wide-angle systems used in PPV nowadays.
In recent years, an increasing numbers of case reports and studies have been published describing a modified SB technique using chandelier endoillumination with a wide-angle viewing system. This modification replaces the need for indirect ophthalmoscopy and provides comfortable and more accurate visualization of the retina and tear assessment, the ability to share information with another surgeon during surgery, and a better means of documentation, recording, and teaching. Moreover, it is a technique well known to VR surgeons from PPV surgeries. It was first reported in 2012 by Aras et al7 who used a torpedo-style chandelier light source through an uncannulated sclerotomy and a noncontact wide-angle viewing system and achieved a reattachment rate of 81%. Kita et al8 published a case report of a young patient who presented with a retinal detachment. No retinal tear had been identified prior to surgery. The patient underwent an SB procedure using a 25-gage fiber-optic chandelier light source through a transscleral cannula, and a retinal tear was found during the operation and treated successfully. This case report raised the yet unanswered question of whether the use of endoillumination and a wide-angle viewing system can better visualize the retina with a higher rate of tears identification. In our study, we found additional intraoperative retinal tears in 31.8% of the eyes in the CSB group compared to18.5% in the TSB group, when compared with the preoperative tears assessment. Although the difference did not reach a level of significance, the trend can be explained by the better visualization through a wide-angle viewing system with endoillumination compared with an indirect ophthalmoscope.
Several other studies described the use of a similar SB modification with a 25-gage fiber-optic chandelier light source that yielded a reattachment rate of 83.3%–95.5% without any significant intraoperative and postoperative complications.9–15 Narayanan et al16 recently published the first and only study thus far that compared patients who underwent CSB with noncontact wide-angle viewing to a group that underwent SB with the indirect ophthalmoscope (14 patients in each group). Those authors observed that the reattachment rates were similarly high, with 92% in the CSB group and 85% in the TSB group. Interestingly, the duration of surgery was significantly shorter in the CSB group, a finding that may be explained by faster recognition of the retinal tears and by avoiding the steps of placing and removing the indirect ophthalmoscope.
Cataract progression is a major concern in an intraocular surgery, and in our case, especially because of the illuminating instrument maintained at the pars plana which can damage the lens during insertion and manipulation of the globe, no difference was found between the groups in the effect of cataract progression. In each group, there were two cases of cataract progression but none of them required surgery during follow-up. It should be noted that in the surgical method, as described in the introduction after the identification of the retinal tears and the performance of the cryopexy, the chandelier light source was removed and the cannula was closed with a scleral plug during the placement of scleral sutures, buckle insertion, and subretinal fluid drainage, if needed. The light source was reintroduced for a final assessment of the buckle height and apposition of the retinal breaks at the end of the surgery.
Our study is the largest series so far (49 eyes overall) which compares the outcome of CSB to TSB surgery. We found no significant differences between the two study groups regarding the reattachment rate and intra- and postoperative complications with comparable result to the literature.
Moreover, the wide-angled viewing system allowed for detection of more retinal tears, illustrating additional benefits.
Limitations of the study are its retrospective nature and that it was not sufficiently powered to statistically define the noninferiority of the modified technique compared with the traditional one, related to the reattachment rate. Without said that the differences in reattachment rates were negligible.
Conclusion
Scleral buckle is an important surgery that should be kept as part of the retinal specialists’ surgical repertoire. Our study represents a supplementary step in the evolution of the well-known scleral buckle procedure. The promising results we showed regarding primary anatomical success, VA outcomes, and complications compared to the traditional surgery, further support its implementation. This modified technique simplifies the operation with no apparent side effects, thereby enhances the VR surgeons competency to be well versed with all techniques of RD repair.
Disclosure
The authors report no conflicts of interest in this work.
References
Custodis E. Treatment of retinal detachment by circumscribed diathermal coagulation and by scleral depression in the area of tear caused by imbedding of a plastic implant. Klin Monbl Augenheilkd Augenarztl Fortbild. 1956;129(4):476–495. German. | ||
Arruga H. Le cerclage equatorial pour traiter le décollement rétinien [An equatorial cerclage to treat retinal detachment]. Bull Mem Soc Fr Ophthalmol. 1958;71:571. | ||
Schepens CL, Okamura ID, Brockhurst RJ. The scleral buckling procedures. 1. Surgical techniques and management. Arch Ophthalmol. 1957;58(6):797–811. | ||
Park SW, Kwon HJ, Kim HY, Byon IS, Lee JE, Oum BS. Comparison of scleral buckling and vitrectomy using wide angle viewing system for rhegmatogenous retinal detachment in patients older than 35 years. BMC Ophthalmol. 2015;15:121. | ||
Park SW, Lee JJ, Lee JE. Scleral buckling in the management of rhegmatogenous retinal detachment: patient selection and perspectives. Clin Ophthalmol. 2018;12:1605–1615. | ||
Heimann H, Bartz-Schmidt KU, Bornfeld N, et al; Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment Study Group. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology. 2007;114(12):2142–2154. | ||
Aras C, Ucar D, Koytak A, Yetik H. Scleral buckling with a non-contact wide-angle viewing system. Ophthalmologica. 2012;227(2):107–110. | ||
Kita M, Fujii Y, Kawagoe N, Hama S. Scleral buckling with a noncontact wide-angle viewing system in the management of retinal detachment with undetected retinal break: a case report. Clin Ophthalmol. 2013;7:587–589. | ||
Nam KY, Kim WJ, Jo YJ, Kim JY. Scleral buckling technique using a 25-gauge chandelier endoilluminator. Retina. 2013;33(4):880–882. | ||
Zhong LX, du Y, Liu W, Huang SY, Zhang SC. Using surgical microscope for sclera buckling and transscleral cryopexy: an alternative procedure of treatment for rhegmatogenous retinal detachment. Biomed Res Int. 2014;2014:364961–364967. | ||
Nagpal M, Bhardwaj S, Mehrotra N. Scleral buckling for rhegmatogenous retinal detachment using vitrectomy-based visualization systems and chandelier illumination. Asia Pac J Ophthalmol (Phila). 2013;2(3):165–168. | ||
Gogia V, Venkatesh P, Gupta S, Kakkar A, Garg S. Endoilluminator-assisted scleral buckling: our results. Indian J Ophthalmol. 2014;62(8):893–894. | ||
Imai H, Tagami M, Azumi A. Scleral buckling for primary rhegmatogenous retinal detachment using noncontact wide-angle viewing system with a cannula-based 25G chandelier endoilluminator. Clin Ophthalmol. 2015;9:2103–2107. | ||
Seider M, Nomides R, Hahn P. Chandelier-assisted scleral buckling for repair of primary rhegmatogenous retinal detachment: initial US experience. In: American Society of Retinal Specialists Annual Meeting; July 2015; Vienna, Austria. | ||
Assi A, Abdelmassih Y, El-Khoury S. Endoillumination-assisted modified scleral buckling. Retina. 2018;38(2):320–324. | ||
Narayanan R, Tyagi M, Hussein A, Chhablani J, Apte RS. Scleral buckling with wide-angled endoillumination as a surgical educational tool. Retina. 2016;36(4):830–833. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.