Back to Journals » Patient Preference and Adherence » Volume 10
Validation of the Chinese version 10-item Perceived Efficacy in Patient-Physician Interactions scale in patients with osteoarthritis
Authors Zhao HW, Luo W , Maly RC, Liu J, Lee JY, Cui YN
Received 19 April 2016
Accepted for publication 13 July 2016
Published 28 October 2016 Volume 2016:10 Pages 2189—2195
DOI https://doi.org/10.2147/PPA.S110883
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Video abstract presented by Wen Luo.
Views: 70
Huiwen Zhao,1 Wen Luo,1 Rose C Maly,2 Jun Liu,1 Junyi Lee,1 Yaning Cui1
1Joint Department, The 2nd Ward of Joint Surgery, Tianjin Hospital, Tianjin, the People’s Republic of China; 2Department of Family Medicine David Geffen School of Medicine, University of California Los Angeles, Los Angeles, CA, USA
Objectives: This study aimed to assess the reliability and validity of the Chinese version of the 10-item Perceived Efficacy in Patient–Physician Interaction (PEPPI-10) scale in hospitalized patients with severe knee osteoarthritis in the People’s Republic of China.
Methods: Between January and March 2015, the Chinese versions of PEPPI, self-efficacy for exercise scale, osteoporosis self-efficacy scale, and modified fall efficacy scale were applied to assess 110 severe knee osteoarthritis patients who were hospitalized in the second ward of the department of arthroplasty surgery of Tianjin Hospital.
Results: The Chinese version of the PEPPI-10 scale had a high coefficient of internal consistency (Cronbach’s α coefficient, 0.907). The score of the Chinese version of PEPPI was weakly correlated with the scores of the Chinese versions of self-efficacy for exercise scale, osteoporosis self-efficacy scale, and modified fall efficacy scale.
Conclusion: The Chinese version of the PEPPI-10 scale exhibits sufficient internal consistency and convergent validity in hospitalized patients with severe knee osteoarthritis in the People’s Republic of China.
Keywords: assessment of osteoarthritis, patient–physician communication, self-efficacy, instrument validation
Background
Osteoarthritis is the most prevalent arthritic disease and affects older adult populations worldwide, and knees are the most commonly affected joints.1 In its advanced stages, it may cause knee dysfunction, pain, and rigidity. In the US, it is estimated that ~27 million patients suffer from osteoarthritis every year, of whom about 10 million suffer from knee osteoarthritis.2 One out of every ten people over the age of 60, on average, suffers from knee osteoarthritis. With the aging of the population in the People’s Republic of China, the incidence of knee osteoarthritis is also increasing annually.3,4 For 2002, the burden of osteoarthritis in disability-adjusted life years was 34,150 person years.5
Since the 1970s, the patient–physician interaction has attracted extensive attention. Due to the unequal status of patients and physicians, patients are often passive, and the patient–physician relationship is very complicated.6 Studies have verified that patient–physician communication can improve the satisfaction of patients, treatment persistency, understanding of medical information, quality of life, and even health.7 Effective patient–physician communication has been shown to be associated with a broad range of improved outcomes of care.8,9 The confidence of patients in communicating with physicians can significantly affect the quality of the patient–physician relationship to a certain extent.10 Another study found that the Perceived Efficacy in Patient–Physician Interaction (PEPPI)-5 (the five item version of PEPPI) was strongly correlated with perceived health management skills, and moderately with social support and psychosocial aspects of health.11 Good patient–physician interaction has been shown to be associated with improved satisfaction with care and health outcomes.12
Self-efficacy is the belief that one can successfully take appropriate and meaningful action.13 The English version of the PEPPI scale is used to test the confidence of patients when they communicate with physicians. The English PEPPI scale has two versions: a full ten-item scale and a simplified five-item scale, both of which have good reliability and validity (Cronbach’s α coefficient for PEPPI-10 is 0.91, respectively, Cronbach’s α coefficient for PEPPI-5 is 0.83.10 The English version of PEPPI-5 has been translated into Dutch, and its clinical feasibility has been verified.11 However, further studies are required to study the differences of this scale in assessing populations of different backgrounds, races, and beliefs. Until now, no studies have investigated the application of this scale in hospitalized patients with severe knee osteoarthritis in the People’s Republic of China. This study aimed to assess the reliability and validity of the Chinese version of PEPPI-10 scale in hospitalized patients with severe knee osteoarthritis in Tianjin, People’s Republic of China.
Patients
A total of 115 patients with severe knee osteoarthritis hospitalized between January and March 2015 were included in the study. Only patients who were hospitalized for knee osteoarthritis of Kellgren–Lawrence grade III and above by X-ray were included. Patients with known cognitive impairments or literacy problems were excluded. The survey was accompanied by a cover letter and consent form explaining the purpose and voluntary nature of the study. In addition to the PEPPI-10, the survey contained questions on other self-efficacy scales. This study was approved by the Tianjin Hospital Ethics Committee and the patients and the Chinese investigators signed the informed consent before the survey.
Methods
Survey methods
The survey was performed using a method where respondents filled out the questionnaire at admission to the hospital. In the data collection process, investigators explained the survey purpose, rights, obligations, and other precautions to the eligible respondents and gained consent from the respondents. The investigators explained the requirements of the questionnaire to the respondents using uniform guidance language. The privacy of the respondents was protected during the investigation process, and all the questionnaires were collected at the time of their completion.
Survey tools
PEPPI
In this study, the ten-item PEPPI was adapted (Supplementary materials), and the English version of the PEPPI was translated into the Chinese version after obtaining consent from the author. It was then back-translated into English and the English and Chinese versions were reconciled by both Chinese- and English-speaking investigators. Compared to the English version, the Chinese version consisted of ten items to assess the confidence of patients when they interacted with physicians (such as get a doctor to take your chief health concern seriously, or knowing what questions to ask the physicians). Each item of the scale was translated into an initial Chinese version by two clinical experts in Tianjin. The respondents were mostly hospitalized patients with severe knee osteoarthritis, and they mainly interacted with physicians and nurses. The modified Chinese version of the PEPPI was formally determined after discussion in a team meeting. Two items of the translated PEPPI scale were raised as being of concern with regard to the Chinese words employed to describe “answer” (item 5 “Get a doctor to answer all of your questions”) and “do something with” (item 9 “Get a doctor to do something about your chief health concern”). A modified Chinese version was developed after a series of meetings with members of the study team. This procedure was intended to ensure that the Chinese version of the PEPPI scale was linguistically appropriate.10 Then, preliminary tests were conducted to confirm the readability and feasibility of the scale in the actual survey by recruiting ten hospitalized patients with severe osteoarthritis.
In recent years, researchers have tested the internal consistency of the PEPPI, and have also analyzed the correlation between the scale and main psychological scales. For example, PEPPI-5 was positively but weakly correlated with perceived health management skills (Effective Musculoskeletal Consumer Scale, EC-17), mental health (the MOS 36-Item Short Form, SF-36 MCS), and support from family and friends (Arthritis Impact Measurement Scales 2, AIMS2).11
Other assessment tools
The self-efficacy for exercise scale (SEE-C) was mainly used to study self-efficacy for exercise in aged people.14 The Cronbach’s α coefficient of its English version was 0.92, displaying a high internal consistency. This scale consisted of nine items, and the Likert ten-grade scoring was applied, where a high score referred to a stronger exercise self-efficacy. The Cronbach’s α coefficient of the Chinese version SEE-C was 0.75, which is adequate and is applicable in clinical studies (PEPPI).15 The modified fall efficacy scale (MFES) was used to assess the confidence in overcoming the fear of falling. Most of the MFES terms16 were based on the fall efficacy scale,17 and they consisted of 14 items to quantitatively analyze the fear of falling in daily activities for the elderly. A Likert 11-point scoring system was adopted, where 0 points referred to no confidence and 10 points referred to absolute confidence. Studies have confirmed that the MFES had good reliability and validity in the elderly population in the People’s Republic of China, with a Cronbach’s α coefficient of 0.9774.18 The osteoporosis self-efficacy scale (OSES) consisted of 21 items, and was divided into two subscales: osteoporosis motion efficacy subscale (1–10) and osteoporosis calcium intake efficacy scale (11–21)19 where the Cronbach’s α coefficient of each scale was 0.90, showing good internal consistency. A visual analog scoring was applied in the English version of the OSES,19 where a high score referred to stronger self-efficacy in preventing osteoporosis. A Likert 11-point scoring was adopted in the revised Chinese version of the OSES, and the Cronbach’s α coefficient of this version was 0.93, suggesting a high level of internal consistency.20
Statistical analysis
Statistical analyses were performed using Statistical Product and Service Solutions 19.0 (SPSS 19.0) (IBM Corporation, Armonk, NY, USA; 2010). Structural validity was examined using confirmatory factor analysis with LISREL 8.7 (Scientific Software International, Lincolnwood, IL, USA). Due to small loss of data, no missing data patterns were identified. Factor analyses were performed to assess the validity of the Chinese version of the PEPPI, in order to determine the hidden representative factors among many variables. Testing results showed that factor analyses were applicable in scales with Kaiser–Meyer–Olkin index >0.7 and P<0.05.21 In this study, factors that met the requirements (eigenvalue >1) were extracted using principal component analysis and varimax rotation. The obtained component matrices were rotated using varimax rotation, and the variables that scored >0.6 were included in the factors.
Based on previous instruments assessing similar constructs of PEPPI,22,23 we tested the correlation coefficients of the Chinese version of PEPPI and SEE-C, MFES, OSES, age, gender, education level, marital status, and disease duration.
The reliability of the Chinese version of the PEPPI was assessed using Cronbach’s α coefficient, which refers to the mean value of the split-half reliability coefficients obtained using all possible methods to divide items and is the most common reliability measure.24 A Cronbach’s α coefficient >0.7 represents a good consistency of the scale or good reliability, and the scale is applicable in clinical studies.25
Results
Patients
Descriptive analyses of the data were performed with all study variables to describe the study participants. Of the 115 participants recruited, five were excluded because of missing responses to questions in the scale, resulting in a total sample size of 110. Of the study participants, 65 were female, the mean age was 63 years, and most of them were married (Table 1). The overall characteristics of the respondents were comparable to other cross-sectional surveys of patients with knee osteoarthritis.
Distribution
The overall score of PEPPI for the patients was relatively high. Statistical analyses were performed using SPSS 19.0 software. The results revealed that the majority of patients tended to have a high score; the skewness was −1.873 and the kurtosis was 3.773. The results of the survey showed that the Chinese version of the PEPPI was negatively skewed and mostly concentrated above the mean value (68.2%). None of the patients scored 0 points, and 31 patients (28.2%) obtained a score of 100 points (Figure 1). Meanwhile, our survey results were not normally distributed due to the floor and ceiling effects.
  | Figure 1 Distribution of total PEPPI scores. |
Factor analysis
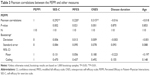
The Cronbach’s α coefficient was 0.907, indicating sufficient internal consistency of this scale, or close correlation between the internal items in the scale. The data of the PEPPI in the 110 patients with knee osteoarthritis were analyzed, and the Kaiser–Meyer–Olkin index was found to be 0.889 and the results of the Bartlett’s test of sphericity revealed a χ2 value of 812.813 (P<0.01), where factor analysis was applicable. Two common factors with eigenvalue ≥1 were extracted using principal component analysis and varimax rotation, and the cumulative contribution rate was 71.178%. The eigenvalue of the first common factor was 6.111, and was 3.955 after rotation, including the 2–7 items, with a contribution rate of 61.105%. The eigenvalue of the second common factor was 1.007 and 3.163 after rotation, including the 1, 8–10 items, with a contribution rate of 10.073% (Table 2, Figure 2).
  | Table 2 Factor analysis of the Chinese version of PEPPI |
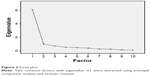  | Figure 2 Scree plot. |
Structural validity and internal consistency
With the exception of the root mean square error of approximation, which was above the cutoff value for good fit, confirmatory factor analysis showed good fit indices for a two-factor model of the PEPPI-10 (df=33, P-value =0.000, root mean square error of approximation =0.164). Standardized factor loadings ranged between 0.75 for item 1 and 1.02 for item 2 (Figure 3). The median residual correlation between the items was 0.25 and the largest residual correlation (between items 2 and 9) was 0.46. The correlation coefficient between the two factors was 0.89 (Figures 3 and 4).
  | Figure 3 Standardized factor loadings and residuals for the items of the PEPPI. |
  | Figure 4 The correlation of main factors. |
Correlation study
The Chinese version of the PEPPI was statistically, significantly, and positively correlated with other self-efficacies, including SEE-C, OSES, and MFES. The score of the Chinese version of the PEPPI was negatively correlated with age (r=−0.018, P>0.05) and disease duration (r=−0.016, P>0.05), but these relationships were not statistically significant (Table 3).
Discussion
The main purpose of this study was to introduce the PEPPI into the People’s Republic of China after translating it into the Chinese version, and to test its reliability and validity in a small sample of hospitalized patients with severe knee osteoarthritis. Our preliminary results confirmed that the Chinese version of the PEPPI has good reliability in hospitalized patients with severe knee osteoarthritis. A high internal consistency of the Chinese version of the PEPPI indicated the same measurement purpose of internal items, and confirmed the reasonability of the contents and items of the questionnaire. Factor analysis is the common and effective method of evaluating construct validity. Our study confirmed that the content of the Chinese version of PEPPI is reasonable. Our results showed that the Cronbach’s α coefficient of the Chinese version was consistent with that of the English version.10 But the factor analysis result shows that the Chinese version of PEPPI-10 has two common factors, which is different from the English version of PEPPI-10.10 The reason for this result may be that cultural background, social, and family roles can influence the PEPPI. The population of the People’s Republic of China is large and all patients undergoing total knee replacement need to pay a certain percentage of the cost of surgery in Tianjin. Although our study showed that the two common factors of the Chinese version of PEPPI-10 have a close relationship, analysis of the survey results showed a negative correlation between the PEPPI in hospitalized patients with severe knee osteoarthritis with age, disease duration, education level, but the correlations were not high. Due to the limited conditions, test–retest reliability was not conducted, which might have provided further evidence of the reliability of PEPPI. However, we preliminarily confirmed that the Chinese version of the PEPPI has sufficient reliability and convergent validity, and is applicable in hospitalized patients with severe knee osteoarthritis in the People’s Republic of China, with clinical value.
Due to the limited sample size, the results of this survey showed that the scores of the Chinese version of the PEPPI in our study population were negatively skewed instead of normally distributed. Therefore, we suggest the need for conducting long-term studies of the Chinese version of the PEPPI with a large sample size to promote the Chinese version in the People’s Republic of China and to identify its applicability in Chinese patients.
Correlation analysis of the Chinese version with the relevant self-efficacy scales for the orthopedic inpatients returned findings consistent with our prior assumptions, where the Chinese version of the PEPPI was positively but weakly correlated with the Chinese versions of the SEE-C, OSES, and MFES. It has been reported that self-efficacy in a specific domain does not emanate from a general sense of efficacy.26 The Chinese version of the PEPPI is used to measure the PEPPI in specific environments. Due to the long-term burden of the disease, inpatients with severe knee osteoarthritis care about their own quality of life, and hope to improve their physical and mental health and quality of life in various aspects. In terms of clinical and demographic characteristics, the PEPPI score showed statistically nonsignificant correlations with age and disease course. This may be because most of the inpatients with severe knee osteoarthritis undergo long-term treatment, leading to skilled patient–physician interaction.
For half a century, a large number of studies on self-efficacy theory have been conducted by clinical physicians, psychologists, nursing scholars, and educators, including the establishment of self-efficacy management programs and design of the specific self-efficacy scale. Similar to other self-efficacy scales, the PEPPI was designed to assess self-efficacy for specific aspects in patients. Efficacy in the patient–physician interaction can be considered a tool to assess the effects of intervention on health treatment and adherence.10
Conclusion
To our knowledge, this is the first time PEPPI was applied to assess hospitalized patients with severe knee osteoarthritis in the People’s Republic of China. Our results indicated that the Chinese version of the PEPPI can be used to measure the PEPPI in hospitalized patients with severe knee osteoarthritis. Although we found good reliability and convergent validity of the Chinese version of the PEPPI in this study, further clinical applications are required to assess its long-term merits and demerits.
Disclosure
The authors report no conflicts of interest in this work.
References
Dawson J, Linsell L, Zondervan K, et al. Epidemiology of hip and knee pain and its impact on overall health status in older adults. Rheumatology. 2004;43(4):497–504. | ||
Burks K. Osteoarthritis in older adults: current treatments. J Gerontol Nurs. 2005;31(5):11–19. | ||
NIH Consensus Statement on total knee replacement. NIH Consens State Sci Statements. 2003;20(1):1–34. | ||
Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87(7):1487–1497. | ||
Office of Statistics, ROC Department of Health. Using national health insurance data in Taiwan to enhance the function of national health expenditure statistics via health resource allocation approach; 2004. Available from: http://www.doh.gov.tw/statistic/table.xls. Accessed December 20, 2006. | ||
Arrow KJ. Uncertainty and the welfare economics of medical care. J Health Polit Policy Law. 2001;6:851–883. | ||
Fortin F, Kirouac S. A randomized controlled trial of preoperative patient education. Int J Nurs Stud. 1976;13:11–24. | ||
Egbert LD, Battit GE, Welch CE, Bartlen MK. Reduction of postoperative pain by encouragement and instruction of patients. N Engl J Med. 1964;270:825–827. | ||
Greenfield S, Kaplan S, Ware J. Expanding patient involvement in care: effects patient outcomes. Am Intern Med. 1985;102(4):520–528. | ||
Maly RC, Frank JC, Marsball GN, DiMatteo MR, Reuben DB. Perceived Efficacy in Patient-Physician Interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc. 1998;46(7):889–894. | ||
Klooster PMT, Oostveen JCM, Zandbelt LC, et al. Further validation of the 5-item Perceived Efficacy in Patient–Physician Interactions (PEPPI-5) scale in patients with osteoarthritis. Patient Educ Couns. 2012;87(1):125–130. | ||
Schenker Y, Stewart A, Na B, Whooley MA. Depressive symptoms and perceived doctor–patient communication in the heart and soul study. J Gen Intern Med. 2009;24(5):550–556. | ||
Bandura A. Self-efficacy: toward a unifying theory of behavior change. Psychol Rev. 1977;84(2):191–215. | ||
Resnick B, Palmer MH, Jenkins LS, Spellbring AM. Path analysis of efficacy expectations and exercise behavior in older adults. J Adv Nurs. 2000;31(6):1309–1315. | ||
Lee LL, Perng SJ, Ho CC, Hsu HM, Lau SC, Arthur A. A preliminary reliability and validity study of the Chinese version of the self-efficacy for exercise scale for older adults. Int J Nurs Stud. 2009;46(2):230–238. | ||
Hill K. Studies of Balance in Older People. Australia: The University of Melbourne; 1998. | ||
Tinetti M, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45(6):239–243. | ||
Hao YP, Liu XQ. Testing of the modified fall efficacy scale in elderly population in China. Chinese J Nurs. 2007;42:19–21. | ||
Horan ML, Kim KK, Gendler P. Development and evaluation of the osteoporosis self-efficacy scale. Res Nurs Health. 1998;21(5):395–403. | ||
Chen YP, Liu XQ. A reliability and validity study of osteoporosis self-efficacy scale. Nurs J PLA. 2005;22:38–39. | ||
Monticone M, Giorgi I, Baiardi P, et al. Development of the Italian version of the tampa scale of kinesiophobia (TSK-I): cross-cultural adaptation, factor analysis, reliability, and validity. Spine (Phila Pa 1976). 2010;35(12):1241–1246. | ||
Clayman ML, Pandit AU, Bergeron AR, Cameron KA, Ross E, Wolf MS. Ask, understand, remember: a brief measure of patient communication self-efficacy within clinical encounters. J Health Commun. 2010;15(Suppl 2):72–79. | ||
Han WT, Collie K, Koopman C, Azarow J, et al. Breast cancer and problems with medical interactions: relationships with traumatic stress, emotional self-efficacy, and social support. Psychooncology. 2005;14(4):318–330. | ||
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. | ||
Crotina JM. What is coefficient alpha? An examination of theory and applications. J Appl Psychol. 1993;78(1):98–104. | ||
Maddux JE, Gosselin JT. Self-efficacy In: Leary MR, Tangney JP, editors. Handbook of Self and Identity. New York: The Guilford Press; 2003:218–238. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.