Back to Journals » Research and Reports in Urology » Volume 9
Using central venous catheter for suprapubic catheterization in cardiac surgery
Authors Bilehjani E, Fakhari S
Received 28 October 2016
Accepted for publication 4 December 2016
Published 4 January 2017 Volume 2017:9 Pages 1—4
DOI https://doi.org/10.2147/RRU.S125996
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Eissa Bilehjani,1 Solmaz Fakhari2
1Department of Cardiovascular Anesthesia, Tabriz University of Medical Sciences, Madani Heart Hospital, 2Department of Anesthesiology, Tabriz University of Medical Sciences, Madani Heart Hospital, Tabriz, Iran
Abstract: Suprapubic catheterization is an alternative method for urinary drainage that is used when transurethral catheterization fails. Traditionally, inserted large-bore suprapubic catheters may cause fatal complications. During the past decade, we used a small central venous catheter (CVC) suprapubicly in 16 male patients for the purpose of urinary drainage, when transurethral catheterization failed. The procedure is performed in no more than 10 minutes. Success rate was 100% and this approach did not lead to any complications. In conclusion, placing a CVC for suprapubic drainage is a safe method with a high success rate and we recommend it in patients with failed transurethral catheterization after a few attempts (2–3 attempts).
Keywords: suprapubic catheterization complication, urethral catheterization, central venous catheter, Seldinger’s technique, cardiac surgery
Introduction
It is mandatory to drain and monitor urinary output intra- and early postoperatively during cardiac surgery.1 Transurethral catheterization is the common method for urinary drainage. Sometimes in male patients with benign prostate hypertrophy or previous prostatectomy, catheter placement may be challenging and unsuccessful; traditionally, professional urologic consultants are called for help in these situations. If transurethral catheterization fails, urologists usually insert a large-bore suprapubic catheter into the bladder.2–4 The procedure involves insertion of a sharp trocar into the bladder percutaneously, usually by palpation, percussion, or under ultrasonographic guidance.5 Although it is generally considered a safe procedure, suprapubic catheter placement is, however, associated with many complications such as bowel injury, bladder injury, or bleeding.6 Nevertheless, suprapubic catheterization is commonly a safe practice, but in cases of full patient heparinization, its complications may be fatal in cardiac surgery.
Cases
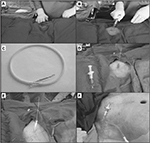
In 16 male patients who were anesthetized for cardiac surgery at Madani Heart Hospital, Tabriz, Iran, during the decade 2006–2015, the surgical team failed to catheterize the bladder transurethrally. Table 1 shows the patients demographic data and the planned surgery. Five patients had a history of benign prostate hypertrophy (BPH); three had previous transurethral resection of the prostate (TURP) surgery (3–12 years ago); and one had previous transabdominal prostatectomy (6 years ago). All of the patients reported no daily urinary problems, except the patient who had transabdominal prostatectomy history. When routine transurethral catheterization (after a few attempts using enough lubricant) became unsuccessful, the patients were administered 500–1,000 mL Ringer’s solution (within 15–30 minutes after the unsuccessful attempt) as well as 5 mg furosemide; both were administered intravenously. Then with appropriate aseptic preparation, a central venous catheter (CVC) (five French single lumens or seven French double lumens) was inserted into the bladder suprapubicly using Seldinger’s technique. At a mildly Trendelenburg position, an empty 10 mL syringe was attached to the CVC needle (18G), we then entered the bladder in the midline direction (mildly directed caudally), 1–2 cm above the symphysis pubis, with continuous aspiration. As the urine flowed freely to the syringe, the guidewire advanced to the bladder (20–30 cm); through the needle and after a small incision with a surgical scalpel blade (No 11), the path was dilated, and finally, the CVC was inserted into the bladder over a guide wire. When free-flowing urine was confirmed by applying light pressure on the bladder, the catheter was fixed at 18–20 cm (Figure 1). In the first two patients, this method was done only when professional urologists attempts failed to catheterize transurethrally; however, in the following cases, no professional help was requested. Bloody urethra was seen in the first three patients. In all of the patients the procedure was performed successfully in no more than 10 minutes. One patient who had previous transabdominal prostatectomy and had had eight transurethral attempts, the other patients did not have any intra- or postoperative hematuria. The patient did not have any problem in mobility. Postoperatively, the CVC was extracted when the patients were able to micturate normally while suprapubic catheter was clamped. Catheters were extracted within 72 hours. After removal, there were not any urinary problems, except one patient who had had the problem preoperatively.
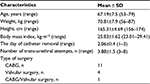  | Table 1 Patients’ characteristics Abbreviations: CABG, coronary artery bypass graft; SD, standard deviation. |
Discussion
Sometimes conventional transurethral catheterization may be unsuccessful intraoperatively. In these situations, the interventions by urologists usually leave the patient with a bloody and traumatized urethra. Considering the common need for full heparinization of patients during cardiac surgery, gross hematuria may occur intra- or postoperatively. Although suprapubic catheter is a good option in such situations, the kits used by urologist are very thick (trocar systems) and may not be suitable for short perioperative period urine drainage.7 Recently, a new method (inside–out approach) for suprapubic catheterization has been introduced for clinical use. The device has mainly been used in female patients with acceptable safety. However, in comparison with our method the method is more invasive, needs more urological skills, and may be more risky when done by anesthesiologists.8 There are different insertion kits for different clinical situations. Suprapubic catheter use can be divided into Foley balloon catheter or catheter without a balloon, which requires a suture to secure. For preventing bowel damage, the patient should have at least 300 mL urine to cause the bladder to be palpable;7 ultrasonography use may reduce complications.9–10 Recently, modified trocar systems have been introduced in clinics which utilize the Seldinger principle. The insertion of a suprapubic catheter should be undertaken by a skillful clinician. There are many indications for suprapubic catheter insertion, but in the operating room, it is placed only in cases of failure of transurethral catheterization.11 Contraindications for suprapubic catheters may be a non-palpable bladder, previous lower abdominal surgery, or ascites.12 Suprapubic catheters may have some potential advantages compared with transurethral catheters, such as greater patient satisfaction,13 normal micturition once the suprapubic catheter is in situ, and decrease in urinary tract infection (UTI).14 Although suprapubic catheters have many advantages, there are also several important risks and limitations to note. The most common are risk of visceral injury (bowel perforation),6,15 bleeding, hematuria, and UTI.12,16 Sheriff et al reviewed 185 cases and identified 2.7% incidence of bowel perforation, with one fatal outcome,17 but the National Patient Safety Agency placed the figure at 0.15%.18 Recently, Dalela et al introduced a new method of suprapubic catheter placement.19 They used an over guidewire method with the help of a transurethral Bougie guide in females with vesicovaginal fistula. Tompkins et al presented an algorithm to contribute to the selection of open, percutaneous, or image-guided methods for suprapubic catheter placement.20 Using a pediatric size (8–10 F), suprapubic catheter may be another option but there is not enough evidence. Anesthesiologists are expert enough in vascular catheterization and may use their skills for a safe suprapubic catheterization to monitor urinary flow intraoperatively. CVCs are small and flexible with appropriate length placed using the over guidewire technique; their size is large enough for perioperative urine drainage, which can be fixed with simple suturing. After only a few unsuccessful attempts (2–3 attempts) for transurethral catheterization, we recommend placing a CVC for suprapubic drainage; this strategy may prevent crucial complications. Thus, suprapubic catheterization using a small CVC is the best solution. It is safe with a high success rate. Our patients had relatively normal body mass indices, however it may be difficult to use this method in obese patients without other supplementary instruments.
Conclusion
In conclusion, placing a small sized CVC for suprapubic drainage (over a guide wire) is a safe method with a high success rate, and we recommend this method in patients with failed transurethral catheterization after a few attempts (2–3 attempts).
Acknowledgments
The authors thank Dr Samad Gaffari, the head manager of the Tabriz Cardiovascular Research Center, for his support in this study. This study is supported by Cardiovascular Research Center of Tabriz University of Medical Sciences.
Ethical considerations
The study was approved by the Ethical Committee of Tabriz University of Medical Sciences and was accepted as an innovative activity. All patients provided written informed consent to participate in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
O’Neal JB, Shaw AD, Billings FT. Acute kidney injury following cardiac surgery: current understanding and future directions. Crit Care. 2016;20:187. | ||
Liu JJ, Guo DP, Gill H. Patterns of urinary catheter consults in a tertiary care hospital. Can J Urol. 2013;20(6):7046–7049. | ||
Bacsu C, Van Zyl S, Rourke KF. A prospective analysis of consultation for difficult urinary catheter insertion at tertiary care centres in Northern Alberta. Can Urol Assoc J. 2013;7(9–10):343–347. | ||
Beaghler M, Grasso M 3rd, Loisides P. Inability to pass a urethral catheter: the bedside role of the flexible cystoscope. Urology. 1994;44(2):268–270. | ||
Lawrentschuk N, Lee D, Marriott P, Russell JM. Suprapubic stab cystostomy: a safer technique. Urology. 2003;62(5):932–934. | ||
Bonasso PC, Lucke-Wold B, Khan U. Small bowel obstruction due to suprapubic catheter placement. Urol Case Rep. 2016;27(7):72–73. | ||
Kashefi C1, Messer K, Barden R, Sexton C, Parsons JK. Incidence and prevention of iatrogenic urethral injuries. J Urol. 2008;179(6):2254–2257. | ||
Flynn BJ, Larke RJ, Knoll PB, Anderson KM, Siomos VJ, Windsperger AP. Prospective study of the Transurethral Suprapubic endo-Cystostomy (T-SPEC®): an “inside-out” approach to suprapubic catheter insertion. Int Urol Nephrol. 2015;47:257–262. | ||
Jacob P, Rai BP, Todd AW. Suprapubic catheter insertion using an ultrasound-guided technique and literature review. BJU Int. 2012;110(6):779–784. | ||
Johnson S, Fiscus G, Sudakoff GS, O’Connor RC, Guralnick ML. The utility of abdominal ultrasound during percutaneous suprapubic catheter placement. Can J Urol. 2013;20(4):6840–6843. | ||
Addison R, Foxley S, Mould C, et al. Catheter care: RCN guidance for nurses. Royal College of Nursing; 2012. Available from: https://www2.rcn.org.uk/__data/assets/pdf_file/0018/157410/003237.pdf. Accessed December 22, 2016. | ||
Harrison SC, Lawrence WT, Morley R, Pearce I, Taylor J. British Association of Urological Surgeons’ suprapubic catheter practice guidelines. BJU Int. 2011;107(1):77–85. | ||
Hunter KF, Bharmal A, Moore KN. Long-term bladder drainage: suprapubic catheter versus other methods. A scoping review. Neurourol Urodyn. 2013;32(7):944–951. | ||
Yates A. The risks and benefits of suprapubic catheters. Nurs Times. 2016;112(6–7):19–22. | ||
Gallagher KM, Good DW, Brush JP, Alhasso A, Stewart GD. Small bowel injury after suprapubic catheter insertion presenting 3 years after initial insertion. BMJ Case Rep. 2013;2013:bcr2013201436. | ||
Adeyemo B, Makovitch S, Foo D. A peculiar complication of suprapubic catheterization: recurrent ureteral obstruction and hydronephrosis. J Spinal Cord Med. 2013;36(2):166–169. | ||
Sheriff MK, Foley S, McFarlane J, Nauth-Misir R, Craggs M, Shah PJ. Long-term suprapubic catheterization: clinical outcome and satisfaction survey. Spinal Cord. 1998;36(3):171–176. | ||
Lamont T, Harrison S, Panesar S, Surkitt-Parr M. Safer insertion of suprapubic catheters: summary of a safety report from the National Patient Safety Agency. BMJ. 2011;342:d924. | ||
Dalela D, Gupta P, Dalela D, et al. Transurethral Bougie-guided placement of suprapubic catheter over guide wire monorail in females: a novel technique. Urology. 2016;94:270–273. | ||
Tompkins AJ, Travis M, Watne RE, Lasser M, Ellsworth P. Decreasing suprapubic tube-related injuries: results of case series and comprehensive literature review. Urol Nurs. 2014;34(1):9–17. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.