Back to Journals » Patient Preference and Adherence » Volume 12
Understanding ethno-cultural differences in cardiac medication adherence behavior: a Canadian study
Authors King-Shier K , Quan H , Mather C, Chong E, LeBlanc P , Khan N
Received 24 March 2018
Accepted for publication 28 June 2018
Published 7 September 2018 Volume 2018:12 Pages 1737—1747
DOI https://doi.org/10.2147/PPA.S169167
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Kathryn King-Shier,1,2 Hude Quan,2 Charles Mather,3 Elaine Chong,4 Pamela LeBlanc,1 Nadia Khan5
1Faculty of Nursing, University of Calgary, Calgary, Canada; 2Department of Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, Canada; 3Department of Anthropology, Faculty of Arts, University of Calgary, Calgary, Canada; 4Faculty of Pharmaceutical Sciences, University of British Columbia, Vancouver, Canada; 5Division of General Internal Medicine, Faculty of Medicine, University of British Columbia, Vancouver, Canada
Background: There are ethno-cultural differences in cardiac patients’ adherence to medications. It is unclear why this occurs. We thus aimed to generate an in-depth understanding about the decision-making process and potential ethno-cultural differences, of white, Chinese, and south Asian cardiac patients when making the decision to adhere to a medication regimen.
Methods: A hierarchical descriptive decision-model was generated based on previous qualitative work, pilot tested, and revised to be more parsimonious. The final model was examined using a novel group of 286 cardiac patients, using their self-reported adherence as the reference. Thereafter, each node was examined to identify decision-making constructs that might be more applicable to white, Chinese or south Asian groups.
Results: Non-adherent south Asians were most likely to identify a lack of receipt of detailed medication information, and less confidence and trust in the health care system and health care professionals. Both Chinese and south Asian participants were less likely to be adherent when they had doubts about western medicine (eg, the effects and safety of the medication). Being able to afford the cost of medications was associated with increased adherence. Being away from home reduced the likelihood of adherence in each group. The overall model had 67.1% concordance with the participants’ initial self-reported adherence, largely due to participants’ overreporting adherence.
Conclusion: These identified elements of the decision-making process are generally not considered in traditionally used medication adherence questionnaires. Importantly these elements are modifiable and ought to be the focus of both interventions and measurement of medication adherence.
Keywords: cardiac, descriptive decision-modeling, ethno-culture, medication adherence
Introduction
The two largest visible minority groups in Canada are Chinese (from China, Hong Kong, Macau, or Taiwan) and south Asians (from India, Pakistan, Sri Lanka, Bangladesh or Nepal) and are among the fastest growing.1 Canada’s health care providers will need to develop a strategy to meet the potential care delivery challenges for these groups.
Chinese are among the least likely whereas south Asians are among the most likely ethnic groups to develop heart disease.2–4 Chinese patients have a higher early mortality following a cardiac event than south Asian or white patients, while south Asian and white patients have a greater likelihood of having future cardiac events.5 A number of studies have revealed that south Asians have higher rates of ischemic heart disease deaths relative to Chines or whites.4–8 There is a lack of clarity or consensus regarding why this occurs. It is possible that ethnocultural differences in access to, and delivery of health care may influence management of heart disease and thereby morbidity and mortality outcomes.
Medication adherence has most recently been defined as “the process by which patients take their medications as prescribed”.9 (p696) Adherence to prescribed medications is already a challenge among the general population, and nonadherence is typically influenced by the interaction of several factors. Krousel-Wood et al10 and others11,12 have identified that patient- (eg, ethnicity, age, socioeconomic status, health beliefs), provider- (eg, sense of reciprocal respect) and health care system-related (eg, access to understandable information, costs) factors affect medication adherence. The disease itself, and the types and numbers of medications may also influence adherence. Coronary artery disease, for example, requires lifestyle modification and often the use of several medications; many of which have their own side effects, thereby increasing the risk of nonadherence.10,11
The majority of patients who suffer a cardiac event will survive the initial event and require chronic (outpatient) management.13,14 The evidence-based management of coronary artery disease includes adhering to cardiac medications as a core therapy to reduce cardiovascular morbidity and mortality. Adherence to antiplatelet agents, beta blocker, statins and ACE inhibitor or angiotensin receptor blocking agents (medications recommended in international cardiovascular guidelines)15,16 is associated with 20%–30% reduction in morbidity and mortality following a cardiac event.15–18 Outside the clinical trial setting, adherence to pharmacotherapy is often poor, thus limiting the extent of therapeutic benefit that can be achieved.9,19,20 The risks of poor adherence are extensive and may result in disease progression, repeated hospitalizations, and death. The collective economic repercussions for medication nonadherence are estimated to exceed $100 billion per year.21
Previous work has shown that Chinese and south Asian cardiac patients are significantly less likely to adhere to their medications,5 and Chinese and south Asian diabetics who are prescribed cardiac medications are also significantly less likely to adhere to their medications relative to their white counterparts.22 These study findings clearly highlight important discrepancies in cardiovascular medication adherence between these three ethno-cultural groups.
Adherence to medications is largely controlled by patients (self-managed). It is unknown how recognized (and yet to be discovered) factors work together or how they are prioritized in the context of patients’ everyday decision-making to take or not to take their medications as prescribed. We aimed to generate a more in-depth understanding about the decision-making process that people with ACS undergo when faced with making therapeutic choices. The results could lay the groundwork to develop and evaluate ethno-culturally sensitive practices that will help to optimize morbidity and mortality reduction in ethnic patients with heart disease.
Methods
Design
We used a three-phased approach to develop and examine a descriptive decision-model that depicts how whites, Chinese and south Asians who have heart disease make the decision to adhere (or not) to their prescribed medications. We used Gladwin’s23 ethnographic decision-tree modeling approach, to describe how people arrive at their decision, and the role that ethno-culture plays in that decision-making. This is a method used primarily by anthropologists and which has been successfully used by health disciplines24–29 to model group behavior based on individuals’ decision-making. This study protocol received approval from the Conjoint Health Research Ethics Board of the University of Calgary and was undertaken in accordance with the Helsinki Declaration of 1964.
Gladwin’s23 decision-tree modeling approach relies on methodological triangulation. Initially, qualitative interviewing strategies are used to generate data that support the inductive work of building the original model (stage A). The interviews focus on learning about the contexts in which, and criteria that, people use to identify and select among available alternatives. The preliminary decision-tree model is developed and refined through quantitatively (survey methods) “pilot testing” (stage B). Thereafter, a quantitative (survey) method is used for determining if the decision-tree model “works” (stage C). Though our aim was not directed at evaluating the model for accuracy, as we were more concerned about examining ethno-cultural differences in how participants respond to the model questions, we examined concordance of the model outcomes with self-reported adherence. The findings from the qualitative interviews have already been published,30 thus the description below focuses on stages B and C.
Sample
There were 286 participants in this study. Gladwin23 suggests a sample of approximately 150 when there are multiple groups and outcomes. This sample size is in keeping with our previous work,26,27 as well as that of others,24,25,28,29 who have used this method.
The majority of participants were selected from a cohort of acute coronary syndrome patients who were included in an international study focused on ethnicity and symptoms presentation. Participants of that cohort study were asked if they would agree to be contacted for potential participation in future studies. These potential participants were contacted by telephone to explain the study and the consent process. Written informed consent for this study was obtained by mailing a consent form to the potential participant. Once the consent form was returned to the investigators, the surveys were undertaken by telephone by trained research assistants. After finding difficulty garnering a sample of Chinese participants, we sought additional participants through a Chinese senior’s cultural center. There, we asked attendees if a physician told them that they had heart disease (coronary artery disease), and if they were prescribed more than two medications for their heart disease. If these potential participants answered affirmatively to each question, we invited them to participate, obtained their written informed consent, and conducted the interview in person.
Participants were selected based on their self-identified ethnicity of European-white, Chinese or south Asian and their ability to speak English; Cantonese or Mandarin; or Punjabi or Hindi. There was a greater proportion of male south Asian and Chinese participants, and a greater proportion of non-English speaking south Asian participants who agreed to participate in this study relative to the cohort from which participants were recruited. The Chinese participants in this study were older relative to the cohort from which they were initially recruited because many were recruited from a senior’s center.
Translation
All study materials were rigorously translated and the details are outlined in a previous publication.31 Briefly, study materials were professionally translated, as well as validated by “lay” people who speak and read the languages of interest. This process ensures that study materials are indeed accurate and understandable (eg, not too high or low a reading level). All non-English interviews were undertaken by highly trained research assistants who fluently spoke and read both English as well as the non-English language.
Decision-tree model preliminary testing and refinement, stage B
A decision-tree model was developed based on qualitative interviews in stage A.30 This model was hierarchical and comprised a series of yes/no questions. The questions were translated into traditional and simplified Chinese characters as well as Punjabi and Hindi languages, as described above. The preliminary (pilot) testing of this model was undertaken by administering a survey based on the series of questions in the model to a small sample of 59 novel white (n=25), Chinese (n=9) and south Asian (n=25) participants (eg, they had not participated in stage A). We aimed to identify areas where the model was unclear (eg, question needed to be reworded); “failing” to work in interview format; the translation needed revision; or interviewer error was occurring.23 Field notes were taken to document any other issues (eg, difficulty with asking questions in the correct order) that arose during this data collection phase. Following these interviews, a more parsimonious model was developed (see Figure 1).
  | Figure 1 The decision-tree model which was based on the qualitative interviews in stage A. |
Decision-tree model examination, stage C
Another novel group of participants was recruited to test the final model. First, a short demographic questionnaire was administered to enable characterization of the study sample. These data were analyzed using ANOVA or Chi-square, as appropriate. Then, in keeping with Gladwin’s23 process, the participants were asked to self-report their adherence behavior as: “consistently,” “sometimes” or “not at all” adherent to their cardiac mediations. These three potential outcomes were identified through the qualitative work undertaken in stage A.30 The number of participants whose self-reported adherence matched the outcome of the decision-tree were identified, then divided by the number of participants. This proportion represented the concordance of the self-report with the model outcome. To address our main study aim, we then compared items significantly related to the model outcomes, and item responses based on ethnicity. Chi-squared tests or Fisher’s exact tests were used for these analyses. All data were analyzed using IBM SPSS Statistics 23.
Results
As seen in Table 1, 286 participants (117 white, 79 Chinese, 90 south Asian) were surveyed to test the decision-tree model. There were differences in the demographic characteristics examined by ethnic group. There were significantly more men in the south Asian group than there were in the white and Chinese groups. The Chinese were significantly older than the other participants (possibly due to where a portion of them were recruited) and south Asians are known to develop heart disease at a younger age.32 More than 87% of Chinese surveys and 50% of south Asian surveys were undertaken in languages other than English. The greatest proportion of Chinese and south Asians immigrated to Canada >20 years ago. Significantly more south Asians were married and resided in extended family situations relative to other participants. Significantly more whites were educated beyond high school (or equivalent) than others. Given the age difference, significantly more Chinese were retired relative to their counterparts.
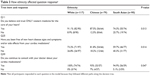
  | Table 1 Demographic characteristics of 286 stage C participants |
To examine decision-making process differences between whites, Chinese and south Asian participants, the dichotomous response to each question in the model (Figure 1) was compared to the model outcome response for each ethnic group (see Table 2 for significant factors). These significant factors are presented here in the order in which they appear in the model. South Asian participants who were not at all adherent to their cardiac medications were most likely to identify that they had not received detailed information from the family doctor about taking their cardiac medications (Figure 1, Q9). They were also most likely to identify that they did not have confidence and trust in the health care system or health care professionals regarding their treatment (Figure 1, Q10). Whites who were consistently or sometimes adherent to their cardiac medications tended to believe and trust only western medicine for the care of their heart (Figure 1, Q11). All study participants who indicated that they could afford the financial costs of their medications tended to be those who consistently or sometimes took their medications (Figure 1, Q18). Those south Asians who indicated they could not always afford the financial costs, and who indicated that they received assistance to pay for their medications were then more likely to be consistently or sometimes adherent than other south Asians (Figure 1, Q19). Whites who indicated that they had an established routine for obtaining and taking medications as prescribed were mostly likely to be consistently or sometimes adherent (Figure 1, Q21). All participants indicated that traveling or leaving home caused some lack of consistency in taking their medications (Figure 1, Q23) and this happened more than 3–4 times per year (Figure 1, Q24). Only white participants indicated that being free of heart disease signs and symptoms and/or side effects from their medications led to them being consistent with taking their cardiac medications (Figure 1, Q25). These white participants were also most likely to accept that they needed to adapt to the signs and symptoms and/or side effects of their medications (Figure 1, Q29). Chinese and south Asian participants who believed they needed all of their prescribed medications were most likely to consistently take their medications (Figure 1, Q28). Those participants that were consistently adherent also indicated that they did not decide for themselves which cardiac medications to take or not to take, while those who were sometimes or not adherent did so (Figure 1, Q31).
To identify questions upon which white, Chinese and south Asian participants significantly differed, we examined each question response relative to the participants’ ethnicity. As seen in Table 3, white participants were most likely to respond affirmatively to the question regarding their belief in only western medicine (Figure 1, Q11). South Asian participants were least likely to identify that they had been free of new heart disease signs and symptoms and/or side effects from their cardiac mediations (Figure 1, Q25). There were slight differences between groups about whether or not they continued to consult with their doctor about their cardiac medications (Figure 1, Q30). Whites were most likely to do so, followed by south Asians, then Chinese.
  | Table 3 How ethnicity affected question responsea |
Finally, there were no significant differences between ethnic groups in outcomes based on their self-report or in model outcomes (Table 4). The overall concordance of the participants’ self-report of adherence with the model outcomes was 67.1%. The model was most successful with the white participants (69.2%), followed by the Chinese (65.8%), and south Asians (65.6%). There were 94 failures in total. Most failures (55/94) occurred because participants (whites and south Asians more than Chinese) overreported relative to underreported adherence.
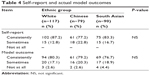  | Table 4 Self-report and actual model outcomes |
Discussion
We used descriptive decision-modeling to develop a more in-depth understanding of the contextual factors that influence how white, Chinese, and south Asian cardiac patients decide to (or not) take their cardiac medications. The model outcomes had a 67.1% concordance with participants’ self-reported adherence to their cardiac medications. We noted that more than half of the instances in which there was a lack of concordance was because the participants tended to over-report as opposed to underreport their adherence, relative to the model outcome. We did not consider the participants’ self-report as a “gold standard” of measurement, yet this finding is consistent with the general and cardiovascular literature focused on medication adherence.33,34
Each participant group (white, Chinese, and south Asian) identified that affordability of medications increased their medication adherence. Though Canada has universal health care, outpatient medications are not part of that benefit. In fact, 10%–12% of Canadians with chronic disease, such as cardio-vascular disease, face financial barriers to managing their illness.35,36 Having a financial barrier to accessing medications has a detrimental effect on health. Campbell et al37 showed that after adjustment for relevant demographic variables, chronic disease patients who self-identified having a financial barrier had an increased rate of disease-related hospitalization (incidence rate ratio 1.36 [95% CI: 1.29–1.44]); as well as mortality (incidence rate ratio 1.24 [95% CI: 1.16–1.32]) compared to those without financial barriers. Having a financial barrier to care is a central construct in this model (all but one participant’s path through the model lead to this question) and leads to detrimental outcomes.
Each participant group also identified that challenges in remembering to take their medications, especially while traveling or being away from home put them at risk for nonadherence. Medication adherence can be positively influenced by developing regular routines (though this related to the model outcomes only for the white participants). Costa et al38 identified that comprehensive self-management programs can improve medication adherence in some patients with chronic illness, but this has not been shown conclusively in patients with cardiovascular disease. They posited that the reason for a lack of significant success in enhancing medication adherence is interventions often lack a strong behavior theory basis. Our earlier qualitative work revealed that Chinese and south Asian patients, in particular, travel for extended periods of time and rely heavily on their pharmacist to assist in ensuring that sufficient medication is dispensed. Thereafter having a regular routine in taking medications enhanced adherence.30
The model revealed that south Asians participants believed that having good communication with health care provider regarding their medications was an important factor in their adherence. In a related item, having decreased confidence in their health care provider negatively influenced adherence.
A systematic review by Sohal et al39 revealed that “language and communication discordance with the health care provider” (p. 7) played an important role in reducing south Asian’s capacity to understand information critical to adhering to their diabetes medications. The review also revealed that south Asian diabetic patients tended to want to follow their physician’s advice and be adherent, but when lack of communication and mistrust ensued, adherence was decreased. The qualitative work by Ens et al40 also revealed that “relationships with health care professionals who demonstrated clear communication and cultural awareness was associated with enhanced medication adherence” (p. 1472). Indeed, we found for all patients in our foundational qualitative work, that physician’s communication was central to adherence for all participants.30
Having some doubt about the need to take all of the prescribed cardiac medications was associated with variability in medication adherence in Chinese and south Asian participants. Our earlier qualitative work revealed that Chinese and south Asian cardiac patients took medications with the hope of being able to reduce or quit taking medications in the future.30 Further, the systematic review by Sohal et al39 identified that concerns about “long-term safety” were also central to south Asians’ adherence. Indeed, Li and Froelicher41 also identified that Chinese were less likely to adhere to hypertension medications when they had a lower perceived benefit from taking the medication. Furthermore, differences in health beliefs (eg, viewing disease as a result of fate and preferring self-management over medical visits) are associated with poor adherence to treatment recommendations.42
Finally, there were central elements to this inductively generated decision-model that are not currently included in medication adherence scales and may warrant inclusion in further study of medication adherence. Indeed, patients’ medication adherence occurs as a result of complex factors,10–12 and not merely having a routine. This study has revealed that having financial barriers to accessing medications, being able to communicate effectively with the health care provider (eg, physician, pharmacist), and believing in western medicine (eg, the effectiveness and safety of the medication) are additional factors that ought to be considered.
There were limitations to this study. The characteristics of the study sample do not necessarily reflect those whites, Chinese and south Asians who are from the general population (and meet inclusion criteria). For example, there was an obvious gender imbalance in the south Asian group. It is not uncommon to have difficulty recruiting south Asian women into studies as they are less likely to speak English than men and are often more protected by their family members against intrusion.43 Also, the Chinese participants were older than expected. This is likely due to participant recruitment from a senior’s cultural center. There is no mechanism using Gladwin’s23 methods to control for these differences. Thus, these study findings may lack some generalizability.
Conclusion
It has not been clear why there are ethno-cultural differences in cardiac patients’ adherence to medications. Key elements associated with adherence for all participants included affordability of the medications and creating a routine (eg, remembering). South Asian participants were less likely to be adherent when they did not perceive having “good” communication with their health care provider (eg, physician, pharmacist). Both Chinese and south Asian participants were less likely to be adherent when they had doubts about western medicine (eg, the effects and safety of the medication). These elements of the decision-making process are not included in the traditionally used medication adherence questionnaires. Importantly these elements are modifiable and ought to be the focus of both interventions and measurement of medication adherence.
Acknowledgments
This study was funded by the Heart and Stroke Foundation of Canada. Kathryn King-Shier is funded by the Guru Nanak Dev Ji DIL Research Chair.
Disclosure
The authors report no conflicts of interest in this work.
References
Canada S. National Household Survey; 2011. Available from: http://www12.statcan.gc.ca/nhs-enm/2011/dp-pd/dttd/Rpeng.cfm?LANG=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GID=0&GK=0&GRP=0&PID=105470&PRID=0&PTYPE=105277&S=0&SHOWALL=0&SUB=0&Temporal=2013&THEME=95&VID=0&VNAMEE=&VNAMEF=. Accessed August 17, 2018. | ||
Li H, Ge J. Cardiovascular diseases in China: current status and future perspectives. IJC Heart Vasculature. 2015;6:25–31. | ||
Rana A, de Souza RJ, Kandasamy S, Lear SA, Anand SS. Cardiovascular risk among South Asians living in Canada: a systematic review and meta-analysis. CMAJ Open. 2014;2(3):E183–E191. | ||
Yusuf S, Reddy S, Ounpuu S, Anand S, et al. Global burden of cardiovascular diseases: Part I: General considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation. 2001;104(22):2746–2753. | ||
Khan NA, Grubisic M, Hemmelgarn B, et al. Outcomes after acute myocardial infarction in South Asian, Chinese, and white patients. Circulation. 2010;122(16):1570–1577. | ||
Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97(6):596–601. | ||
Sheth T, Nair C, Nargundkar M, et al. Cardiovascular and cancer mortality among Canadians of European, south Asian and Chinese origin from 1979 to 1993: an analysis of 1.2 million deaths. Can Med Assoc J. 1999;161(2):132–138. | ||
Tunstall-Pedoe H, Kuulasmaa K, Mähönen M, Tolonen H, Ruokokoski E, Amouyel P. Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10-year results from 37 WHO MONICA project populations. Monitoring trends and determinants in cardiovascular disease. Lancet. 1999;353(9164):1547–1557. | ||
Vrijens B, de Geest S, Hughes DA, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharm. 2012;73(5):691–705. | ||
Krousel-Wood M, Thomas S, Muntner P, Morisky D. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19(4):357–362. | ||
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med Overseas Ed. 2005;353(5):487–497. | ||
Banning M. A review of interventions used to improve adherence to medication in older people. Int J Nurs Stud. 2009;46(11):1505–1515. | ||
Liem SS, van der Hoeven BL, Oemrawsingh PV, et al. MISSION!: optimization of acute and chronic care for patients with acute myocardial infarction. Am Heart J. 2007;153(1):14-e1. | ||
Townsend N, Nichols M, Scarborough P, et al. Cardiovascular disease in Europe – epidemiological update 2015. Eur Heart J. 2015;36(40):2696–2705. | ||
O’Gara PT, Kushner FG, Ascheim DD, et al. ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Amer Coll Cardiol. 2013;61(4):e78–e140. | ||
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Euro Heart J. 2018;39(2):119–177. | ||
Heart Outcomes Prevention Evaluation Study Investigators; Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342(3):145–153. | ||
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360(9326):7–22. | ||
Sackett DL, Snow JC. The magnitude of adherence and nonadherence. In: Haynes RB, Taylor DW, Sackett DL, editors. Compliance in Health Care. Vol. 11. Baltimore, MA: Johns Hopkins University Press; 1979. | ||
Sabate E. Adherence to Long-term Therapies: Evidence for Action. Geneva: World Health Organization; 2003. http://www.who.int/chronic_conditions/en/adherence_report.pdf | ||
Rasmussen JN, Chong A, Alter DA. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007;297(2):177–186. | ||
Chong E, Wang H, King-Shier KM, et al. Prescribing patterns and adherence to medication among South-Asian, Chinese and white people with type 2 diabetes mellitus: a population-based cohort study. Diabet Med. 2014;31(12):1586–1593. | ||
Gladwin CH. Ethnographic Decision-tree Modeling. Newbury Park, CA: Sage Publications; 1989. | ||
Beck KA. Ethnographic decision tree modeling: a research method for counseling psychology. J Couns Psychol. 2005;52(2):243–249. | ||
Oh HS, Park HA. Decision tree model of the treatment-seeking behaviors among Korean cancer patients. Cancer Nurs. 2004;27(4):259–266. | ||
King-Shier KM, Quan H, Mather C, et al. Understanding coronary artery disease patients’ decisions regarding the use of chelation therapy for coronary artery disease: descriptive decision modeling. Int J Nurs Stud. 2012;49(9):1074–1083. | ||
King-Shier KM, Mather CM, Leblanc P. Understanding the influence of urban- or rural-living and cardiac patient’s decisions about diet and exercise. Intern J Nurs Stud. 2013;50:1513–1523. | ||
Mathews HF, Hill CE. Applying cognitive decision theory to the study of regional patterns of illness treatment choice. Am Anthropol. 1990;92(1):155–170. | ||
Montbriand MJ. Decision tree model describing alternate health care choices made by oncology patients. Cancer Nurs. 1995;18(2):104–117. | ||
King-Shier KM, Singh S, Khan NA, et al. Ethno-cultural considerations in cardiac patients’ medication adherence. Clin Nurs Res. 2017;26(5):576–591. | ||
King KM, Khan N, Leblanc P, Quan H. Examining and establishing translational and conceptual equivalence of survey questionnaires for a multi-ethnic, multi-language study. J Adv Nurs. 2011;67(10):2267–2274. | ||
Gupta M, Brister S, Verma S. Is South Asian ethnicity an independent cardiovascular risk factor? Can J Cardiol. 2006;22(3):193–197. | ||
Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int. 2015;2015:1–12. | ||
Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119(23):3028–3035. | ||
Campbell D, King-Shier K, Hemmelgarn B, et al. The association between financial barriers and care and outcomes for patients with chronic disease. Health Report. 2014;25(5):3–12 (Statistics Canada Catalogue No 82-003-X). | ||
Law MR, Cheng L, Dhalla IA, et al. The effect of cost on adherence to prescription medications in Canada. Can Med Assoc J. 2012;184(3):297–302. | ||
Campbell DJ, Manns BJ, Weaver RG, et al. Financial barriers and adverse clinical outcomes among patients with cardiovascular-related chronic diseases: a cohort study. BMC Med. 2017;15(1):33. | ||
Costa E, Giardini A, Savin M, et al. Interventional tools to improve medication adherence: review of literature. Pat Pref Adher. 2015;9:1303–1314. | ||
Sohal T, Sohal P, King-Shier KM, Khan NA. Barriers and facilitators for type-2 diabetes management in South Asians: a systematic review. PLoS One. 2015;10(9):e0136202. | ||
Ens TA, Seneviratne C, Jones C, King-Shier KM. Factors influencing South Asian cardiac patients’ compliance to their medication regimen. Intern J Nurs Stud. 2014;51(11):1472–1481. | ||
Li WW, Froelicher ES. Gender differences in Chinese immigrants: predictors for antihypertensive medication adherence. J Transcult Nurs. 2007;18(4):331–338. | ||
Li WW, Stotts NA, Froelicher ES. Compliance with antihypertensive medication in Chinese immigrants: cultural specific issues and theoretical application. Res Theory Nurs Pract. 2007;21(4):236–254. | ||
Quay TA, Frimer L, Janssen PA, Lamers Y. Barriers and facilitators to recruitment of South Asians to health research: a scoping review. BMJ Open. 2017;7(5):e014889. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

