Back to Journals » Clinical Ophthalmology » Volume 14
Three-Year Outcomes of Simultaneous Accelerated Corneal Crosslinking and Femto-LASIK for the Treatment of High Myopia in Asian Eyes
Authors Lim L , Lim EWL, Rosman M , Koh JCW, Htoon HM
Received 26 April 2020
Accepted for publication 12 June 2020
Published 25 September 2020 Volume 2020:14 Pages 2865—2872
DOI https://doi.org/10.2147/OPTH.S260088
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Li Lim,1– 3,* Elizabeth Wen Ling Lim,4,* Mohamad Rosman,1– 3 Jane Chwee Wah Koh,1 Hla Myint Htoon1,3
1Singapore National Eye Centre, Singapore 168751, Singapore; 2Singapore Eye Research Institute, Singapore 169856, Singapore; 3Duke-NUS Medical School, Singapore 169857, Singapore; 4Yong Loo Lin School of Medicine, National University of Singapore, Singapore 119228, Singapore
*These authors contributed equally to this work
Correspondence: Li Lim
Singapore National Eye Centre, 11 Third Hospital Ave, Singapore 168751, Singapore
Tel +65 62277255
Fax +65 62277290
Email [email protected]
Purpose: To determine the long-term visual outcomes of simultaneous femtosecond laser-assisted laser in situ keratomileusis (femto-LASIK) and accelerated cross-linking (CXL) [LASIK Xtra] for the treatment of high myopia.
Patients and Methods: All 163 consecutive eyes of 85 patients who underwent LASIK Xtra for the treatment of high myopia and/or myopic astigmatism (spherical equivalent ≥ − 6.00 D) in Singapore National Eye Centre from the years 2013 to 2017 were included in this retrospective case series. Post-operative follow-up was up to 3 years.
Results: Of the 163 eyes, 67 were followed up for 1 year (mean 12.9 months), 69 for 2 years (mean 24.0 months) and 43 for 3 years (mean 36.4 months). Overall mean follow-up was 22.8 months (9– 46 months). The mean pre-operative spherical equivalent (SE) was − 8.60 ± 1.47 D [range: − 11.75 to − 4.75] (n = 163) and mean attempted correction SE was − 8.84 ± 1.41 D [range: − 11.88 to − 5.25]. Most eyes (> 95%) maintained an uncorrected distance visual acuity of 6/12 or better over 3 years. Visual outcomes were predictable with ≥ 95% of eyes achieving a SE correction within ± 1D of attempted correction over 3 years. There was a mild regression in SE refraction over 3 years with a mean of − 0.10 ± 0.45 D three years post-operatively (p = 0.03). The safety index was > 1.05 at 3 years follow-up. There were no significant post-operative complications though 24 eyes had mild haze and 2 eyes had grade 1 diffuse lamellar keratitis that resolved within 1 month.
Conclusion: Our 3-year LASIK Xtra results show favorable safety, efficacy, predictability and stability outcomes in Asian patients with high myopia.
Keywords: LASIK Xtra, refractive surgery, cross-linking
Introduction
Laser in situ keratomileusis (LASIK), although a common and popular refractive surgical procedure, can have rare but potentially sight-threatening complications such as post-LASIK ectasia. Post-LASIK regression could also occur resulting in the need for retreatment. The exact mechanism of post-LASIK ectasia is unknown but it is postulated that the creation of a corneal flap during the LASIK procedure may decrease corneal rigidity and weaken the corneal biomechanical structure, increasing the chances of post-LASIK ectasia.1,2
The first cases of post-LASIK ectasia were reported by Seiler et al in 1998.3,4 Currently, the prevalence of post-LASIK ectasia ranges from 0.02% to 0.6%.2,5 Risk factors include thin corneas, pre-operative high myopia or hyperopia and patients with abnormal topography (such as forme fruste keratoconus).3,4,6 Corneal collagen cross-linking (CXL) has been shown to prevent further progression of keratoconus and post-LASIK ectasia.7–11 In recent times, however, the focus has shifted towards the prevention of post-LASIK ectasia by performing simultaneous LASIK and accelerated CXL (LASIK Xtra). It has also been suggested that LASIK Xtra not only has the potential to prevent post-LASIK ectasia but could also reduce post-LASIK regression.12–15
As LASIK Xtra is a relatively new technique, literature comparing its long-term safety and efficacy in the treatment of myopia is limited, especially in the Asian population.16 Kanellopoulos et al reported good safety and efficacy outcomes in a case series of LASIK Xtra patients with an average follow-up time of 3.5 years (1–4.5 years).17 In a two-year comparative study, Kanellopoulos et al reported better refractive and keratometric stability in patients with LASIK Xtra as compared to LASIK in the treatment of myopia.14 Xu et al performed a two-year follow-up case series which also reported favourable outcomes.18 Other one-year follow-up studies have also been reported.19–23 Since post-LASIK ectasia can occur from as early as 1 week to several years post-LASIK,24,25 long-term studies on LASIK Xtra are important to determine whether it is effective in the prevention of post-LASIK ectasia.
Our study reports three-year data analysing the safety and efficacy of LASIK Xtra in Asians with high myopia. To the best of our knowledge, apart from Kanellopoulos et al17 there have been no other reports with ≥3-year follow-up in literature on the safety and efficacy of LASIK Xtra in myopia.
Methodology
This is a retrospective clinical audit of 163 consecutive eyes of 85 patients who underwent the LASIK Xtra procedure for the treatment of high myopia and/or myopic astigmatism at the Laser Vision Centre, Singapore National Eye Centre (SNEC) from November 2013 to December 2017. High myopia was defined as greater than −6.00 diopters (D) of spherical equivalent. Patients were followed-up for up to a period of 3 years. A comprehensive 100% clinical audit of all LASIK Xtra cases in SNEC was performed independently by our Clinical Audit Department. This study was exempted from institutional review by the Singhealth Centralised Institutional Review Board. All patient data complied with Singhealth data protection privacy rules.
The following were the inclusion criteria for surgery: (1) no contact lens wear prior to surgery for 1 week and 3 weeks for soft contact lenses and rigid contact lenses, respectively; (2) stable refractive error for 1 year before surgery; (3) normal peripheral retina or after prophylactic treatment with photocoagulation; (4) no previous ocular surgery; (5) no corneal diseases; (6) no glaucoma; (7) no history of ocular trauma. The following patients were excluded from surgery: (1) corneal topographic evidence of keratoconus or forme fruste keratoconus; (2) active ocular or systemic disease which may affect corneal wound healing; (3) pregnant or lactating women; (4) patients requiring monovision correction.
Pre-operative evaluation before LASIK Xtra surgery included measurement of uncorrected distance visual acuity (UDVA), best corrected visual acuity (BCVA), subjective and cycloplegic refraction, slit lamp and fundal examination, corneal topography (Orbscan II corneal topography system [Bausch & Lomb Surgical, Orbtek Inc, Salt Lake City, Utah, USA] and Pentacam HR [Oculus, Germany]) and endothelial cell counts (ECC) (Konan Medical Corporation, Hyogo, Japan).
Surgical Technique
LASIK Xtra procedures were performed by two ophthalmologists (LL and MR). Femto-LASIK was performed as per normal, followed by the CXL procedure. The surgical steps are as follows: (1) a 100–110μm LASIK flap was created using the IntraLase IFS femtosecond laser (Abbott Medical Optics, Irvine, CA); (2) LASIK ablation was performed using WaveLight EX500 (Alcon Laboratories, Fort Worth, TX), wavefront optimised profile. The nomogram obtained from the WaveLight EX500 was used and the refractive target was plano to +0.5D; (3) the bare cornea stromal bed was soaked in 0.22% saline-diluted riboflavin solution (VibeX Xtra [Avedro, Inc., Waltham, MA, USA]) for 45 seconds with special care taken to prevent contact of the riboflavin with the LASIK flap; (4) the cornea stromal bed was subsequently irrigated to remove residual riboflavin and the LASIK flap was carefully repositioned; (5) a UVA fluence of 30 mW/cm2 was then applied for 46 seconds, total energy 1.4 J/cm2 (KXL® CXL system [Avedro, Inc., Waltham, MA, USA]). These irradiation parameters were previously used in another study and were also recommended by Avedro;26 (6) a bandage contact lens was placed at the end of the procedure and the following topical medications were instituted: topical moxifloxacin (Vigamox®, Alcon Laboratories, Inc, Fort Worth, TX, USA), dexamethasone phosphate 0.1% (Maxidex®, Alcon Laboratories, Inc, Fort Worth, TX, USA) for a week and hypromellose 0.3% and dextran 0.1% (Tears Naturale Free®, Alcon Laboratories, Fort Worth, TX, USA) for 1 to 2 months.
Statistical Analysis
The efficacy, predictability and safety of LASIK Xtra were evaluated. The following measures were used to determine efficacy: (1) the proportion of cases that achieved a UDVA of 20/40 or better; (2) the proportion of cases that achieved a UDVA of 20/20 or better; (3) the efficacy index (postoperative UDVA/preoperative BCVA). For predictability, the proportion of cases within 1.0D and within 0.5D of the refractive aim was calculated. The safety of LASIK Xtra was evaluated with the following measures: (1) presence of intra-operative and post-operative complications; (2) the proportion of cases with improved or unchanged post-operative BCVA compared to pre-operative BCVA; (3) the safety index (post-operative BCVA/pre-operative BCVA).
Descriptive statistics for estimates were presented as mean, standard deviation, and range (min-max) for continuous variables. For categorical variables, estimates were described for frequency, percentage and 95% confidence intervals of the percentage. For continuous variables, the one way-ANOVA test was used to make group comparisons. For categorical variables, we used Chi–Squared test, Fisher’s Exact test, as well as pair-wise McNemar test evaluations. Statistical significance was set at <0.05. SPSS version 24.0 was used for the statistical analysis (Released 2016. IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp. USA).
Results
Baseline Characteristics
Between the years 2013 to 2017, 163 eyes of 85 patients underwent LASIK Xtra performed by 2 surgeons (LL and MR) at SNEC for the treatment of high myopia. 67 eyes were followed up for 1 year (9–16 months, mean 12.9 months), 69 eyes for 2 years (18–30 months, mean 24.0 months) and 43 eyes for 3 years (28–46 months, mean 36.4 months). Overall mean follow-up was 22.8 months (9–46 months). The mean age of the patients was 29 ± 6 years (range: 21–46 years) and 54 patients (63% of total) were female. The majority of the patients (n = 65, 77%) were Chinese, 7% were Malay, 3% were Indian and 13% were of other races. The mean pre-operative SE was −8.60 ± 1.47 D (n = 163) and mean attempted correction SE was −8.84 ± 1.41 D.
Efficacy
Overall, LASIK Xtra was effective in treating high myopia as evidenced by good post-operative uncorrected distance visual acuity (UDVA). Over 3 years, most eyes (>95%) maintained a UDVA of 6/12 or better and >65% of eyes maintained a UDVA of 6/6 or better. Specifically, 98.5% of eyes achieved a UDVA of 6/12 or better at 1 year follow-up, 95.4% at 2 years follow-up and 97.7% at 3 years follow-up. 71.6% of eyes achieved a UDVA of 6/6 or better at 1 year follow-up, 73.8% at 2 years follow-up and 65.1% at 3 years follow-up. There was no statistically significant difference between the percentage of eyes that achieved a UDVA of 6/12 (p = 0.64, one way ANOVA test) or 6/6 (p = 0.63, one way ANOVA test) at 1, 2 or 3-year follow-up. The efficacy index remained close to 1 throughout all 3 years of follow-up: 0.95 at 1 year follow-up, 0.97 at 2 years follow-up and 0.92 at 3 years follow-up (Table 1; Figure 1).
 |
Table 1 Postoperative Uncorrected Distance Visual Acuity (UDVA) and Efficacy Index |
 |
Figure 1 Bar chart showing the percentage of eyes with uncorrected distance visual acuities (UDVA) pre-operatively and up to 3 years post-operatively. |
Predictability
More than 95% of eyes achieved an SE correction within ± 1D of attempted correction. 95.2% achieved an SE correction within ± 1D of attempted correction at 1 year follow-up, 95.2% at 2 years follow-up and 97.7% at 3 years follow-up. 85.5% achieved an SE correction within ± 0.5D of attempted correction at 1 year follow-up, 90.8% at 2 years follow-up and 83.3% at 3 years follow-up. There was no statistically significant difference between the percentage of eyes that achieved an SE correction within ± 1D or ± 0.5D at 1, 2 or 3-year follow-up (p values: 0.54 [for ± 1D], 0.48 [for ± 0.5D]). (Table 2; Figure 2)
 |
Table 2 Percentage of Eyes with Spherical Equivalent (SE) Within ± 1D and ± 0.5D of Attempted Correction |
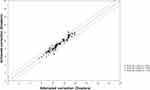 |
Figure 2 Graph showing the correlation between the attempted and achieved spherical equivalent (SE) corrections. |
Stability
There was a mild regression in SE refraction over 3 years post-operatively with a mean of 0.14 ± 0.43 D (1 year post-operatively), 0.07 ± 0.40 D (2 years post-operatively) and −0.10 ± 0.45 D (3 years post-operatively). There was an overall statistically significant difference between the post-operative SE refraction over 3 years (p value = 0.03, one way ANOVA). Pairwise analysis showed that the statistically significant difference was between post-operative year 1 and year 3 (p value = 0.03, adjusted Bonferroni correction) (Table 3; Figure 3)
 |
Table 3 Preoperative and Postoperative Mean Spherical Equivalent (SE) |
 |
Figure 3 Graph showing the stability of mean spherical equivalent (SE) refraction post LASIK Xtra over 3 years of follow-up. |
Safety
The safety index of the LASIK Xtra procedure was 1.13 at 1 year follow-up, 1.12 at 2 years follow-up and 1.07 at 3 years follow-up. Post-operatively, 3 cases (4.9%) had a drop in BCVA of 1 Snellen line from 6/4.5 to 6/6 at 1 year. Two cases (2.9%) had a drop in BCVA of 1 Snellen line while 1 case (1.5%) had a drop in BCVA of 2 Snellen lines at 2 years. Two cases (4.8%) had a drop in BCVA of 1 Snellen line 3 years post-operatively. (Figure 4) No significant intra or post-operative complications were observed in the LASIK Xtra patients. There was the presence of mild post-operative haze in 24 eyes (14.7%) but this resolved within 12 months. Grade 1 diffuse lamellar keratitis (DLK) that resolved within 1 month post-operatively was observed in 2 eyes. Postoperative mean endothelial cell counts (ECC) were not significantly different from preoperative ECC (preoperative ECC = 2968.9 ± 313.3, n = 145, postoperative ECC = 2945.4 ± 414.0, n = 84, 3–16 months post-operatively) (p value = 0.925, non-parametric Wilcoxon Signed Ranks test).
 |
Figure 4 Bar chart showing the percentage of eyes that had changes in Snellen lines of best corrected visual acuity (BCVA) over 3 years of follow-up. |
Discussion
Our results show that LASIK Xtra has good efficacy, predictability, stability and safety outcomes over a 3-year follow-up period. Our findings are similar to other studies done on LASIK Xtra. To date, there are 8 published studies with ≥1 year follow-up on LASIK Xtra for myopia, 6 of which are comparative studies and 2 of which are case series.14,17–23 In the previous studies, the mean SE was −4 to −7.5D. The cross-linking settings during the LASIK Xtra procedure varied with UV power ranging from 9 to 30mW, riboflavin soak times from 1 to 2 mins and riboflavin concentrations from 0.1 to 0.25%. In 1 and 2 year comparative studies by Kanellopoulos et al, statistically significant reductions in refractive shift and increases in keratometric stability were found in LASIK Xtra patients as compared to LASIK-only patients.14,21 In the 2-year randomised comparative study by Kanellopoulos et al, 93.8% of patients in the LASIK Xtra group achieved a UDVA of 20/20 or better while only 84.9% of LASIK-only patients achieved this (p = 0.045).14 The lower efficacy observed in our study (71.6% of patients achieving a UDVA of 6/6) could be explained by the higher myopia present in our study population (mean pre-operative SE: −8.60 ± 1.47 D) as compared to Kanellopoulos et al (mean pre-operative SE: −6.67 ± 2.14 D).14 The keratometric stability in Kanellopoulos et al was also better in the LASIK Xtra group, with no forward shift as compared to the LASIK-only group (p = 0.032).14 As for the predictability reported in Kanellopoulos et al, 84.6% of LASIK Xtra patients achieved an SE correction within ± 0.5D of attempted correction whereas 81.3% of LASIK-only patients achieved this (p = 0.0754).14 This predictability is similar to our study where 83.3% of LASIK Xtra patients achieved an SE correction within ± 0.5D of attempted correction at 3 years follow-up.
However, in 1 year comparative studies by Tomita et al and Seiler et al, no significant differences between the 2 groups were observed.20,22 None of the studies reported any significant adverse events associated with LASIK Xtra for myopia such as ectasia or significant regression. In the 1 year comparative study by Seiler et al, patients with an ectasia score of 3 to 6 were recruited and a higher prevalence of transient diffuse lamellar keratitis (DLK) was observed in the LASIK Xtra group even though the riboflavin used was dextran free.20
A one-year prospective randomized trial by Kohnen et al compared between femto-LASIK with combined accelerated CXL versus femto-LASIK alone in patients with high myopia and showed that while apparently safe, LASIK Xtra showed no advantages over conventional LASIK.23 Both groups showed no difference in UDVA and refractive stability and no signs of keratectasia 1 year post-operatively.23
Our 3-year LASIK Xtra results showed a statistically significant mild myopic regression from a mean SE of +0.14D at 1 year follow up to a mean of −0.1D at 3 years follow-up. In comparison, studies on patients with high myopia who underwent LASIK-only procedures reported a higher incidence and amplitude of myopic regression over time. In 4 cohort studies, the average LASIK retreatment rate was 12%.27–30 However, when LASIK is used to treat high myopia, the retreatment rate went up to 30%.31,32 In a 10-year follow-up study by Alio et al on patients with LASIK treatment for high myopia (mean pre-operative spherical equivalent of −13.95 ± 2.79D, range −10.00 to −24.50D), myopic regression in patients who did not undergo retreatment was −0.25 ± 0.18D per year.28 Predictability was relatively poor with only 42% of patients achieving correction of within ± 1D of attempted correction. Only 40% showed a post-operative UDVA of 20/40 or better.28 In contrast, our study showed a predictability of 83.3% of LASIK Xtra patients achieving an SE correction within ± 0.5D of attempted correction at 3 years followup and 97.7% of eyes achieving UDVA of 6/12 at 3 years follow-up.
The improved refractive and keratometric stability seen could be explained by the creation of additional chemical bonds between the collagen fibres of the corneal stroma during the CXL procedure, thereby improving the biomechanical stability of the cornea.33,34 A possible explanation for reduced myopic regression rates seen in LASIK Xtra could be due to reduced epithelial hyperplasia seen in LASIK Xtra as compared to LASIK-only. In a study done on LASIK patients with high myopia (attempted SE correction: −8.50 to −12.25D), Spadea et al found a negative correlation between epithelium thickness and post-operative manifest refraction, indicating that increased epithelial thickness has a role in myopic regression.35 Kanellopoulos et al found a positive correlation between increase in post-operative epithelial thickness and SE myopic correction, indicating a greater epithelial thickness increase with a greater amount of myopic ablation.36 This could explain the higher regression and retreatment rates seen in highly myopic patients.31,32 In another study done on matched highly myopic patients, Kanellopoulos et al found reduced epithelial increase in LASIK Xtra as compared to LASIK-only, suggesting a possible mechanism for the reduction in regression seen in LASIK Xtra.37
Of all the published studies with ≥1 year follow up, only 1 case series had a follow-up of more than 2 years. Kanellopoulos et al performed a consecutive case series of 43 patients with an average of 42 months (range: 12–54 months) follow-up.17 Apart from Kanellopoulos et al17 our study is currently the longest follow-up study of LASIK Xtra patients with up to 3 years of follow-up.
When CXL was first developed, the Dresden protocol with a UV-A irradiation of 3mW/cm2 for 30 minutes (5.4J/cm2) was used.38 Following the Bunsen-Roscoe Law of Reciprocity, the biological effect of the UV light is proportionate to the total energy delivered to the tissue regardless of irradiance level and time.39 In order to shorten the time of UV irradiation, accelerated CXL techniques have been developed with irradiation ranging from 7mW/cm2 in 15 minutes to 30mW/cm2 for 3 minutes while maintaining a total energy exposure of 5.4J/cm2.40,41 For LASIK Xtra, however, total UV energy exposure varies from as low as 1.4J/cm2 to as high as 5.4J/cm2.14,19,42 Since CXL is used as a form of prophylaxis in LASIK Xtra rather than therapeutic treatment, most studies use a lower total UV energy exposure as compared to keratoconus treatment. Our study demonstrates that although a lower UVA energy of 1.4 J/cm2 (UVA fluence of 30 mW/cm2, 46 seconds duration) was utilized compared with the other LASIK Xtra studies with >1 year follow-up with UVA energy utilization ranging from 1.8–5.4J/cm2, it had similar refractive stability and reduced myopic regression to the other studies. This suggests that a low UVA energy of 1.4 J/cm2 may be sufficient for the purpose of achieving refractive stability for high myopia treatment without inducing a hyperopic shift over time. Further long-term studies would be useful in evaluating optimal UV irradiation settings for LASIK Xtra.
The limitations of our study are: it is a retrospective clinical audit and not a comparative study; it has a relatively high number of patients lost to follow-up and that corneal biomechanical properties are not measured in our study. Our study also did not address the question of whether LASIK Xtra is effective in preventing or reducing the incidence of post LASIK ectasia. Further long-term comparative studies would be required to determine if LASIK Xtra is able to prevent or reduce the incidence of post-LASIK ectasia.
In conclusion, LASIK Xtra showed favorable efficacy, predictability, stability and safety outcomes in an Asian population with high myopia over a 3-year follow-up period. Further long-term comparative studies with larger sample sizes would be useful for continued evaluations of the clinical outcomes of this procedure.
Acknowledgment
Oral Paper Presentation Session: Refractive Outcomes, SPS-206: LASIK with Simultaneous Accelerated Corneal Crosslinking for Treatment of High Myopia: Long-Term Outcomes. American Society of Cataract and Refractive Surgeons Annual Symposium and Congress, 3–7 May 2019, San Diego, USA. Li Lim and Elizabeth Wen Ling Lim are co-first authors for this work.
Disclosure
LL has received travel reimbursement and honorarium from Avedro in the past 1 year. Otherwise, the authors did not receive any sources of public or private financial support. The authors do not have any financial or proprietary interests in any product, material or method.
References
1. Jaycock PD, Lobo L, Ibrahim J, Tyrer J, Marshall J. Interferometric technique to measure biomechanical changes in the cornea induced by refractive surgery. J Cataract Refract Surg. 2005;31(1):175–184. doi:10.1016/j.jcrs.2004.10.038
2. Binder PS. Analysis of ectasia after laser in situ keratomileusis: risk factors. J Cataract Refract Surg. 2007;33(9):1530–1538. doi:10.1016/j.jcrs.2007.04.043
3. Seiler T, Koufala K, Richter G. Iatrogenic keratectasia after laser in situ keratomileusis. J Refract Surg. 1998;14(3):312–317.
4. Seiler T, Quurke AW. Iatrogenic keratectasia after LASIK in a case of forme fruste keratoconus. J Cataract Refract Surg. 1998;24(7):1007–1009. doi:10.1016/S0886-3350(98)80057-6
5. Chen MC, Lee N, Bourla N, Hamilton DR. Corneal biomechanical measurements before and after laser in situ keratomileusis. J Cataract Refract Surg. 2008;34(11):1886–1891. doi:10.1016/j.jcrs.2008.06.035
6. Buzard KA, Tuengler A, Febbraro JL. Treatment of mild to moderate keratoconus with laser in situ keratomileusis. J Cataract Refract Surg. 1999;25(12):1600–1609. doi:10.1016/S0886-3350(99)00284-9
7. Wittig-Silva C, Whiting M, Lamoureux E, Lindsay RG, Sullivan LJ, Snibson GR. A randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: preliminary results. J Refract Surg. 2008;24(7):S720–725. doi:10.3928/1081597X-20080901-15
8. Vinciguerra P, Camesasca FI, Albe E, Trazza S. Corneal collagen cross-linking for ectasia after excimer laser refractive surgery: 1-year results. J Refract Surg. 2010;26(7):486–497. doi:10.3928/1081597X-20090910-02
9. Salgado JP, Khoramnia R, Lohmann CP, Winkler von Mohrenfels C. Corneal collagen crosslinking in post-LASIK keratectasia. Br J Ophthalmol. 2011;95(4):493–497. doi:10.1136/bjo.2010.179424
10. Kymionis GD, Bouzoukis D, Diakonis V, et al. Long-term results of thin corneas after refractive laser surgery. Am J Ophthalmol. 2007;144(2):181–185. doi:10.1016/j.ajo.2007.04.010
11. Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the athens protocol. J Refract Surg. 2011;27(5):323–331. doi:10.3928/1081597X-20101105-01
12. Rajpal RK, Wisecarver CB, Williams D, et al. Lasik Xtra((R)) provides corneal stability and improved outcomes. Ophthalmol Ther. 2015;4(2):89–102. doi:10.1007/s40123-015-0039-x
13. Aslanides IM, Mukherjee AN. Adjuvant corneal crosslinking to prevent hyperopic LASIK regression. Clin Ophthalmol. 2013;7:637–641.
14. Kanellopoulos AJ, Asimellis G. Combined laser in situ keratomileusis and prophylactic high-fluence corneal collagen crosslinking for high myopia: two-year safety and efficacy. J Cataract Refract Surg. 2015;41(7):1426–1433. doi:10.1016/j.jcrs.2014.10.045
15. Kanellopoulos AJ, Kahn J. Topography-guided hyperopic LASIK with and without high irradiance collagen cross-linking: initial comparative clinical findings in a contralateral eye study of 34 consecutive patients. J Refract Surg. 2012;28(11 Suppl):S837–840. doi:10.3928/1081597X-20121005-05
16. Lim EWL, Lim L. Review of laser vision correction (LASIK, PRK and smile) with simultaneous accelerated corneal crosslinking − long-term results. Curr Eye Res. 2019;1–10.
17. Kanellopoulos AJ. Long-term safety and efficacy follow-up of prophylactic higher fluence collagen cross-linking in high myopic laser-assisted in situ keratomileusis. Clin Ophthalmol. 2012;6:1125–1130. doi:10.2147/OPTH.S31256
18. Xu W, Tao Y, Wang L, Huang Y. Evaluation of biomechanical changes in myopia patients with unsatisfactory corneas after femto second-laser in situ keratomileusis (fs-lasik) concurrent with accelerated corneal collagen cross-linking using corvis-st: two-year follow-up results. Med Sci Monit. 2017;23:3649–3656. doi:10.12659/MSM.905493
19. Celik HU, Alagoz N, Yildirim Y, et al. Accelerated corneal crosslinking concurrent with laser in situ keratomileusis. J Cataract Refract Surg. 2012;38(8):1424–1431. doi:10.1016/j.jcrs.2012.03.034
20. Seiler TG, Fischinger I, Koller T, Derhartunian V, Seiler T. Superficial corneal crosslinking during laser in situ keratomileusis. J Cataract Refract Surg. 2015;41(10):2165–2170. doi:10.1016/j.jcrs.2015.03.020
21. Kanellopoulos AJ, Asimellis G, Karabatsas C. Comparison of prophylactic higher fluence corneal cross-linking to control, in myopic LASIK, one year results. Clin Ophthalmol. 2014;8:2373–2381. doi:10.2147/OPTH.S68372
22. Tomita M, Yoshida Y, Yamamoto Y, Mita M, Waring G. In vivo confocal laser microscopy of morphologic changes after simultaneous LASIK and accelerated collagen crosslinking for myopia: one-year results. J Cataract Refract Surg. 2014;40(6):981–990. doi:10.1016/j.jcrs.2013.10.044
23. Kohnen T, Lwowski C, Hemkeppler E, et al. Comparison of femto-LASIK with combined accelerated cross-linking to femto-LASIK in high myopic eyes: a prospective randomized trial. Am J Ophthalmol. 2020;211:42–55. doi:10.1016/j.ajo.2019.10.024
24. Rao SN, Epstein RJ. Early onset ectasia following laser in situ keratomileusus: case report and literature review. J Refract Surg. 2002;18(2):177–184.
25. Lifshitz T, Levy J, Klemperer I, Levinger S. Late bilateral keratectasia after LASIK in a low myopic patient. J Refract Surg. 2005;21(5):494–496. doi:10.3928/1081-597X-20050901-12
26. Tan J, Lytle GE, Marshall J. Consecutive laser in situ keratomileusis and accelerated corneal crosslinking in highly myopic patients: preliminary results. Eur J Ophthalmol. 2014.
27. Yuen LH, Chan WK, Koh J, Mehta JS, Tan DT, SingLasik Research G. A 10-year prospective audit of LASIK outcomes for myopia in 37,932 eyes at a single institution in Asia. Ophthalmology. 2010;117(6):1236–1244e1231. doi:10.1016/j.ophtha.2009.10.042
28. Alio JL, Muftuoglu O, Ortiz D, et al. Ten-year follow-up of laser in situ keratomileusis for high myopia. Am J Ophthalmol. 2008;145(1):55–64. doi:10.1016/j.ajo.2007.08.035
29. Hersh PS, Fry KL, Bishop DS. Incidence and associations of retreatment after LASIK. Ophthalmology. 2003;110(4):748–754. doi:10.1016/S0161-6420(02)01981-4
30. Randleman JB, White AJ
31. Sugar A, Rapuano CJ, Culbertson WW, et al. Laser in situ keratomileusis for myopia and astigmatism: safety and efficacy: a report by the American Academy of Ophthalmology. Ophthalmology. 2002;109(1):175–187. doi:10.1016/S0161-6420(01)00966-6
32. Alio JL, Soria F, Abbouda A, Pena-Garcia P. Laser in situ keratomileusis for −6.00 to −18.00 diopters of myopia and up to −5.00 diopters of astigmatism: 15-year follow-up. J Cataract Refract Surg. 2015;41(1):33–40. doi:10.1016/j.jcrs.2014.08.029
33. McCall AS, Kraft S, Edelhauser HF, et al. Mechanisms of corneal tissue cross-linking in response to treatment with topical riboflavin and long-wavelength ultraviolet radiation (UVA). Invest Ophthalmol Vis Sci. 2010;51(1):129–138. doi:10.1167/iovs.09-3738
34. Hovakimyan M, Guthoff RF, Stachs O. Collagen cross-linking: current status and future directions. J Ophthalmol. 2012;2012:406850. doi:10.1155/2012/406850
35. Spadea L, Fasciani R, Necozione S, Balestrazzi E. Role of the corneal epithelium in refractive changes following laser in situ keratomileusis for high myopia. J Refract Surg. 2000;16(2):133–139.
36. Kanellopoulos AJ, Asimellis G. Longitudinal postoperative lasik epithelial thickness profile changes in correlation with degree of myopia correction. J Refract Surg. 2014;30(3):166–171.
37. Kanellopoulos AJ, Asimellis G. Epithelial remodeling after femtosecond laser-assisted high myopic LASIK: comparison of stand-alone with LASIK combined with prophylactic high-fluence cross-linking. Cornea. 2014;33(5):463–469. doi:10.1097/ICO.0000000000000087
38. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135(5):620–627.
39. Bunsen RRH. Photochemische Untersuchungen. Poggendorff Ann. 1855;96:373–394.
40. Kanellopoulos AJ. Long term results of a prospective randomized bilateral eye comparison trial of higher fluence, shorter duration ultraviolet a radiation, and riboflavin collagen cross linking for progressive keratoconus. Clin Ophthalmol. 2012;6:97–101. doi:10.2147/OPTH.S27170
41. Tomita M, Mita M, Huseynova T. Accelerated versus conventional corneal collagen crosslinking. J Cataract Refract Surg. 2014;40(6):1013–1020. doi:10.1016/j.jcrs.2013.12.012
42. Low JR, Lim L, Koh JCW, Chua DKP, Rosman M. Simultaneous accelerated corneal crosslinking and laser in situ keratomileusis for the treatment of high myopia in Asian eyes. Open Ophthalmol J. 2018;12(1):143–153. doi:10.2174/1874364101812010143
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
