Back to Journals » Clinical Ophthalmology » Volume 14
Three-Year Effect of Phakic Intraocular Lenses on the Corneal Endothelial Cell Density
Authors Shaaban YM, Badran TAF
Received 29 October 2019
Accepted for publication 10 January 2020
Published 20 January 2020 Volume 2020:14 Pages 149—155
DOI https://doi.org/10.2147/OPTH.S236041
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yasmine Maher Shaaban, 1, 2 Tamer Abdel Fattah Badran 1, 2
1Department of Ophthalmology, Faculty of Medicine, Ain Shams University, Cairo 11566, Egypt; 2The Eye Subspecialty Center (ESC), Cairo 11402, Egypt
Correspondence: Yasmine Maher Shaaban 49 Mohamed Farid Street, Heliopolis, Cairo 11351, Egypt
Tel +20 128 893 1888
Email [email protected]
Purpose: To compare the effect of three different phakic intraocular lenses (pIOLs) on the corneal endothelial cell density (ECD).
Patients and Methods: This was a prospective observational cohort study that included 60 eyes (30 patients) with axial myopia of − 6.50 to − 22.00 diopters (D). The Verisyse anterior chamber (AC) rigid iris fixated pIOL, the Veriflex (AC) flexible iris fixated pIOL, and the Visian posterior chamber (PC) implantable collamer lens (ICL) were implanted in three equal groups of patients. The effect of the three pIOLs on the ECD was compared over a follow-up period of one week, and one, three, and six months, and one, two, and three years. Specular microscopy was done to evaluate the cornea before the surgery and throughout the study. Changes were statistically analyzed and compared.
Results: In the first three postoperative months, Verisyse and Veriflex pIOLs induced almost the same amount of endothelial cells loss of 10.3% and 10.6%, respectively, while ICLs showed endothelial cells loss of 3.5%. At the end of the three-year study, Veriflex pIOLs induced the highest rate of endothelial cell loss of 25%, while Verisyse and ICL lenses showed endothelial cells loss of 15.7% and 13.4%, respectively. The main effect of time and type of lens was statistically significant (p< 0.001).
Conclusion: All pIOLs cause a decrease in ECD. The AC pIOLs tend to be associated with more cell loss than PC pIOLs. Surgical insult is the important factor responsible for the early endothelial cell loss, while the material from which the pIOL is made may be an important factor for the continuous corneal endothelial cell loss over a long time.
Keywords: refractive intraocular lenses, cornea, specular microscopy
Introduction
Patients with high myopia who have an inadequate vision with spectacles or are intolerant to contact lenses always seek other ways to correct their vision. Laser in situ keratomileusis (LASIK) can achieve a good result up to-12.00 diopters (D) of myopia, but patients with a higher degree of myopia are always at risk of corneal ectasia. Refractive lens exchange with IOL implantation can correct myopia, but lensectomy results in a complete loss of accommodation for presbyopic patients and carries the risk of retinal detachment. Phakic IOL is surgically placed either in the anterior chamber (AC), or in the posterior chamber (PC), to improve visual acuity (VA) without removing the crystalline lens, and with preservation of the accommodation.
The purpose of this study is to compare the effect of Verisyse pIOL (Abbott Medical Optics, Santa Ana, CA, USA), Veriflex pIOL (AMO, Santa Ana, CA, USA), and Visian Implantable Collamer Lens (ICL, Staar Surgical, Monrovia, CA, USA), on the corneal ECD over three years. Phakic IOLs are implanted in young individuals and are expected to stay in their eyes throughout their life. Our objective is to study the possible corneal complications that can occur due to phakic IOL implantation.
Patients and Methods
All the participants in this study were selected from subjects seeking refractive surgery in the Refractive Surgery Unit in The Eye Subspecialty Center, (ESC) Heliopolis, 11402, Cairo, Egypt. All procedures in this study adhered to the Declaration of Helsinki (2008) Ethical Principles for Medical Research Involving Human Subjects, and approved by the ESC committee. Written informed consent was obtained from all the candidates. Case recruiting started in December 2015, and all were followed up for three years.
This prospective observational cohort study included 60 eyes divided into three groups (20 eyes in each group). In the Verisyse group, patient age ranged between 21–35 years with refraction of - 6.50 to −21.00D, in the Veriflex group, patient age ranged between 19–32 years with refraction of −7.00 to −22.00D, and in the ICL group, patient age ranged between 19–30 years with refraction of −7.50 to −18.00D.
The Verisyse lens is a single-piece lens made from Perspex CQ-UV, a clinical-quality ultraviolet light-absorbing polymethyl methacrylate (PMMA). The lens has an overall length of 8.50 mm with a 5 and 6mm optic for correction of myopia, its power ranges from - 3.00 to - 23.50 D and is placed in the AC.1 The Veriflex lens is made of a flexible material called polysiloxane (silicone material), the haptics are rigid and made from PMMA. The overall length is 8.50 mm, the optic diameters are 5 and 6 mm, its power ranges from −2.00 D to −14.50 D and is inserted in the AC.2 The ICL is a rectangular single piece lens made of Collamer (a copolymer of hydroxyethyl methacrylate and porcine collagen), available in four diameters with variable optical zones, its power ranges from −3.00 to −23.00D and is injected in the PC.3
Inclusion and Exclusion Criteria
Corneal ECC of 2800 cells/mm2 for age 19 −25 years, 2650 cells/mm2 for age 26–30 years, and 2400 cells/mm2 for age 31–35 years, were included in the study. Other factors included AC depth of ≥3 mm, stable refraction (<0.50D change for one year), clear crystalline lens, ametropia beyond the range of laser surgery and contact lens intolerance.
The exclusion criteria included ECC<2000 cell/mm2, ACD<3mm, iris or pupil abnormalities, congenital bilateral cataracts, recurrent anterior or posterior segment diseases, history of retinal detachment, single-eyed patient, glaucoma, proliferative diabetic retinopathy, compromised corneal endothelium or dystrophy, pregnancy, and lactation.
The Preoperative Evaluation
It included medical history, a complete ophthalmic examination, best-corrected VA, cycloplegic refraction, slit-lamp examination, ocular tension, pupil size, and indirect ophthalmoscopy to rule out possible retinal breaks in highly myopic eyes. Before the preoperative evaluation, soft and hard contact lenses were discontinued for 48 hrs, and one week respectively. Before the surgery, IOL Master (The ZEISS IOL Master 500), was used to measure the pIOL power, the ACD, and the white to white (WTW) diameter. The (WTW) diameter is measured to select the pIOL diameter. Specular microscopy (EM-3000 CBD/Tomey, Phoenix), was used to evaluate the corneal ECD before the surgery and throughout the study.
Surgical Methods
All surgeries had been done by the same surgeon under local peribulbar anesthesia using the same surgical microscope (Carl Zeiss OPMI Lumera i, Meditec, USA). For eyes undergoing implantation of Verisyse AC rigid iris-fixated pIOL, an MVR 20-gauge needle was used to make two side ports 9 mm incisions apart at 3 and 9 o’clock. The main limbal incision was made in the steepest corneal meridian using microkeratome 3.2 mm and enlarged to 5.2–6.2 mm according to the lens optic size. Carbachol intraocular solution 0.01% (Carbakol, Optitech®) was injected inside AC, followed by injection of hydroxypropyl methylcellulose 2% (Aurovisc, Aurolab®). The lens was introduced inside the AC, rotated horizontally, and the inclavation was done, followed by peripheral iridectomy. The viscoelastic material was removed, and one stitch was taken to secure the wound. In the case of the Veriflex AC flexible iris fixated pIOL, the steps were the same except that the main corneal incision was done using 2.4 mm keratome and enlarged to 2.8 mm. The lens was introduced in the AC, followed by stromal hydration. In case of the PC ICL lens, the steps were the same except that the pupil was dilated before the surgery, 2.8 mm temporal clear corneal incision was done, the lens was introduced into the AC through an injector, the four footplates of the lens were tucked under the iris into the sulcus, followed by peripheral iridectomy and stromal hydration.
Postoperative Follow-Up
Topical steroid (Prednisone acetate 1% Pred Forte, Allergan®), and antibiotic (Moxifloxacin hydrochloride 0.5% Vigamox, Alcon®), were used five times per day for a week then tapered gradually over one month to decrease inflammation and to prevent infection. The patient was instructed not to rub or to put pressure on the eye during sleep, and not to lift heavy objects. Long-term follow-up visits were scheduled from a few days to a few weeks apart then from several weeks to several months apart, followed by annual eye examinations. Specular microscopy was performed after one week, one, three, and six months, one, two, and three years. Slit-lamp examination and ocular tension measurements were done at each visit. All the data were collected, recorded, and statistically analyzed.
Statistics
Mean and standard deviations were used to present quantitative data. One-way analysis of variance (ANOVA) was used to compare age and refraction error between the three groups. Proportions were used to present qualitative data with the Chi-square test as a test of significance. Data of ECD and ECD percentage drop from the preoperative level was analyzed using repeated measure ANOVA with between-group factor (the lens type). The full model was used, and when the interaction term proved to be statistically significant, the simple effects rather than the main effects were tested using post-hoc Bonferroni correction. In all tests, a p-value of ≤0.05 was considered statistically significant. The Statistical Package for the Social Sciences (SPSS version 23, IBM Corporation, Chicago, IL, USA) was used for the statistical analysis.
Results
The age was 26.1± 3.8 years in the Verisyse group, 25.5±5.0 years in the Veriflex group, and 24.4±3.5 years in the ICL group. The refraction was −13.30±4.00D in the Verisyse group, −12.40±7.50D in the Veriflex group, and −11.30±7.00D in the ICL group. Females represent 60% of both Verisyse and Veriflex groups, and 65% of the ICL group. Males represent 40% of both Verisyse and Veriflex groups, and 35% of the ICL group. No statistically significant difference between the three groups of patients regarding the mean age (p = 0.427), the mean refraction (p = 0.595), and the sex (p = 0.932). The ECD in Verisyse, Veriflex and ICL groups showed a mean drop of 429, 726 and 392 cells respectively at the end of the three-year study (Table 1).
 |
Table 1 Mean and SD of the Corneal ECD Preoperatively and at Different Follow-Up Points in the Three Types of pIOLs |
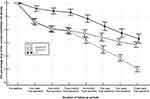
The ECD percentage drop in Verisyse, Veriflex, and in ICL group at one week, one, three, and six months, one, two, and three years are shown in (Figure 1).
There was less drop in ECD in association with ICL when compared to both Verisyse and Veriflex at different points of the follow-up period (p<0.05). Comparing both Verisyse and Veriflex, there was no statistically significant difference in the first 3 months, but later, at 6 months, and through the three- year follow-up period, there was a statistically significant difference between both lenses (p<0.05). With Veriflex, the percentage of ECD drop was the highest after the third month, and through the three years follow -up, p<0.05 (Table 2).
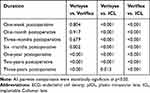 |
Table 2 Comparisons Between the Percentage Drop of the Corneal ECD at Different Follow- Up Points in the Three Types of pIOLs |
Verisyse pIOL showed +2 AC reaction in the first week and decreased by time. Veriflex pIOL showed +2 to +3 reaction in the first week and stayed for a longer time with a possibility of recurrence when the steroids were tapered. The ICL showed +1 reaction in the first week and decreased with time.
Morphological changes were monitored in the three groups of patients. Using the coefficient of variation (CV), there was an early (first three months) postoperative increase in cell size diversity (polymegathism) of 0.32–0.39, which tends to be stable six months postoperatively. Also, the percentage of hexagonality (HEX) showed a slight early postoperative (first three months) decrease which tends to be stable six months postoperatively. All cases showed HEX more than 65% by the end of the study.
Discussion
Although several studies have demonstrated that the Artisan/Verisyse, Artiflex/Veriflex, and Visian ICL have good predictability, stability, and long-term safety, there are complications especially concerning corneal ECD. Corneal endothelial cells do not regenerate and are important in keeping the cornea clear. Normal corneal ECD at birth ranges between 4000–5000 (cells/mm2), which declines with aging at a rate of 0.3–0.6% per year with an approximate value of 2000–3000 cells/mm2 in a normal adult eye. At age 40, people tend to have about 3000 cells/mm2, and by age 70, the count has decreased to about 2000 cells/mm2. It is established that ECD decreases with age, trauma, glaucoma, corneal dystrophies, diabetes mellitus, refractive surgery, and intraocular surgery.4
In this study, we did review some other studies relevant to ours regarding the three pIOLs, and their effect on ECD, and we did find a lot of discrepancies between results. In this study, there was a statistically significant difference among the three groups of patients. The percentage drop in ECC was 15.7 ± 2.2%, 25 ± 2.1% and 13.5 ± 3.8% in the Verisyse, Veriflex, and ICL groups, respectively at the end of the study (p<0.001). In a study done by Karimian et al5 comparing the three pIOLs in 112 (40 Artisan, 36 Artiflex, and 36 ICL) eyes for a mean of 30±11 months follow-up period. They reported no statistically significant difference among the three studied groups. At the end of the follow-up period, the level of decrease in ECC was 10%, 9% and 9% in the Artisan, Artiflex, and ICL groups, respectively. Also, Bohac et al6 reported no significant difference in the mean ECC postoperatively in both Artisan (198 eyes) and Artiflex (212 eyes) over 36 months. Stulting et al1 showed EC loss in 684 eyes implanted with Artisan pIOL within a mean of 4.76% over three years. In a ten-year study of the ECD after iris fixated pIOL implantation, Chelbi et al7 reported a mean decrease in annual ECD of 0.87%. Budo et al8 studied 518 eyes implanted with Artisan pIOL over 36 months, they reported a decline in the ECD of 4.8%, 2.4%, 1.7% and 0.7% at 6 months, one, two, and three years respectively. Benedetti et al9 reported a decline in ECD of 5.4% in 93 Artisan pIOL over ten years. Tahzib et al10 reported a decline in ECD of 8.86% in 89 Artisan pIOL over ten years. These results are in controversy with our results that reported 12.9%, 14.6%, and 15.7% decline in the ECD in the Verisyse group throughout one, two, and three years respectively.
In accordance with our study regarding the Artisan/Verisyse pIOL, Landesz et al11 reported a drop of 10.9% of ECD at 36 months in 67 eyes. Silva et al12 reported a drop in the mean ECD of 14.05% at 5 years in 26 eyes. Jonker et al13 implanted 127 eyes with the Artisan pIOL. The ECD showed a total loss of 16.6% over10 years of follow-up. ECD had decreased by ≥25% in 7.9% of cases, the count was <1500 cells/mm2 in 3.9% of cases, and the explantation of the pIOL was done in 6.0% of cases. The authors claimed that a smaller ACD was a risk factor for the loss.
Concerning the Artiflex/Veriflex pIOL, a study done by Dick et al14 to assess the ECD of 290 eyes implanted with Artiflex pIOL for two years, reported a mean EC loss of 0.05%, 1.79%, and 1.07% at six months, one, and two years respectively. In another study by Nassiri et al15 55 eyes underwent Artiflex lens implantation for correction of myopia, there was no statistically significant change in the ECD after six months of follow-up. The opposite was reported by Jonker et al.2 They reported chronic EC loss of 10% over 5 years in eyes implanted with the Artiflex myopic pIOL. In up to 3.1% of eyes, significant EC loss resulted in subsequent pIOL explantation. In our study, there was no statistically significant difference between both Verisyse and Veriflex lenses till the third postoperative month but starting from the six months and throughout the study, there was a significant difference between both lenses. Veriflex showed a more decrease in the ECC (Table 2, Figure 1).
Regarding the Implantable Collamer lens (ICL), Sachdev et al16 reported a non-significant EC loss of 2.01% ± 4.12% in 134 eyes implanted with ICL over 36 months. Moya et al17 implanted 144 eyes with ICL for myopia. Twelve years postoperatively, the mean ECC decreased by 19.75%. Dejaco-Ruhswurm et al18 implanted 34 eyes with ICL, ECC decreased by 7.9% and 12.9% after two and three years, respectively. This percentage is close to our percentage which is an ECC drop of 11.4% and 13.4% after two and three years, respectively.
Comparing Artiflex/Veriflex versus ICL, Sayman Muslubas et al19 compared Artiflex with ICL in two groups of 15 eyes each for 12 months, the mean ECD was significantly less in the Artiflex group than the ICL group. This was similar to our study in which the mean ECD was statistically significantly less in the Veriflex group than the ICL group from the first week postoperatively and throughout the study (Table 2).
Generally, all pIOLs cause a chronic corneal EC loss. Artiflex/Veriflex pIOLs are reported to be associated with more flare in the AC and more corneal EC loss.20,21 Edelhauser et al22 think that EC loss one to three years after surgery is intraoperative trauma and subsequent prolonged endothelial cell remodeling following the surgical procedure rather than ongoing cell loss. Kohnen et al21 claimed that the complications of pIOL are primarily related to pIOL position and type.
In this study, regardless of the type of implanted pIOL, there was a continuous postoperative EC loss which was statistically significant. We think the impact of the surgery is the factor causing the early EC loss. This includes the surgical manipulations, the implantation techniques, the size of the wound, the process of lens inclavation or lens unfolding, the possibility of contact between the implanted lens and endothelium, intraoperative bleeding, and postoperative ocular tension rise. In general, the iris fixated lenses (Verisyse, Veriflex), induced more EC loss in the early three months postoperatively (10.3% and 10.6%), respectively, while the ICL shows the least EC loss of (3.5%). This may be because the ocular tissue and corneal shape are less disturbed during ICL implantation.
We think that the material from which the pIOL is made is an important factor that causes a continuous EC loss over a long time. Silicone is well known for its complications when implanted in the human eye. Its effect on the cornea, angle, tension, and retina are well known.23 Veriflex pIOL being made mostly of silicone is expected to cause AC reaction and subclinical chronic uveitis with a subsequent drop of ECC. Although both AC iris-fixated lenses (Verisyse and Veriflex) are implanted almost in the same location in the AC, the response of the eye to each lens is different. An ICL made of silicone and implanted in the PC as usual resulted in total bilateral corneal decompensation which required corneal transplantation one year after surgery.20
We also think that the discrepancies in the results between different studies are due to the many involved variables, some related to the eye such as the preoperative ECC, the AC depth, and the endothelial cell tolerance, or related to the implanted lens such as location, design, and material from which the lens is made. Different surgeons’ experience, techniques and using different surgical and diagnostic equipment during different studies can also influence the outcomes.
Some limitations of the present study were the relatively low number of participants and a short period of follow-up. Studies with a larger number of candidates and longer follow-up periods are necessary to determine the endothelial safety profile.
Conclusions
All pIOLs cause a decrease in the ECD. Surgical insult is an important factor responsible for the early endothelial cell loss. The material from which the pIOL is made may be the factor causing endothelial cell loss over a long time. The silicone material may play a part in this continuous cell loss.
Improvement of the surgeons’ experience, surgical technique, lens design, lens material, proper choice of the appropriate pIOL for each case is very important. All patients should be followed-up regularly for the rest of their life. The ECC, AC reaction and the ocular tension should be monitored regularly. Trauma should be avoided as it is a risk factor for plOL dislocation.
Abbreviations
AC, Anterior chamber; ACD, Anterior chamber depth; EC, Endothelial cell; ECC, Endothelial cell count; ECD, Endothelial cell density; ICL, Implantable Collamer lens; LASIK, Laser In situ keratomileusis; PC, Posterior chamber; pIOL, Phakic intraocular lenses; VA, Visual acuity; WTW, White to white.
Ethics Approval and Informed Consent
All procedures performed in the study adhered to the Declaration of Helsinki (2008) Ethical Principles for Medical Research Involving Human Subjects. Written informed consent was obtained from all of the candidates and approved by the Ethics Committee of the Eye Subspecialty Center (ESC),18 El Khalifa El Maamoun Street, Heliopolis, 11402, Cairo.
Data Sharing Statement
The data used to support the findings of this study are included in the article.
Acknowledgments
The authors acknowledge the support of Dr. Mustafa HM, Professor of Community and Public Health, Faculty of Medicine, Ain Shams University, for performing the statistics of this study.
Author Contributions
Both authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Stulting RD, John ME, Maloney RK, Assil KK, Arrowsmith PN, Thompson VM; U.S. Verisyse Study Group. Three-year results of artisan/verisyse phakic intraocular lens implantation. Results of the United States food and drug administration clinical trial. Ophthalmology. 2008;115:464–472. doi:10.1016/j.ophtha.2007.08.039
2. Jonker SMR, Berendschot TTJM, Ronden AE, Saelens IEY, Bauer NJC, Nuijts RMMA. Five-year endothelial cell loss after implantation with artiflex myopia and artiflex toric phakic intraocular lenses. Am J Ophthalmol. 2018;194:110–119. doi:10.1016/j.ajo.2018.07.015
3. Lisa C, Alfonso JF, Alfonso-Bartolozzi B, Fernández-Vega L, Pérez-Vives C, Montés-Micó R. Collagen copolymer posterior chamber phakic intraocular lens supported by the ciliary sulcus to treat myopia: one-year follow-up. J Cataract Refract Surg. 2015;41(1):98–104. doi:10.1016/j.jcrs.2014.05.036
4. Joyce NC. Proliferative capacity of corneal endothelial cells. Exp Eye Res. 2012;95(1):16–23. doi:10.1016/j.exer.2011.08.014
5. Karimian F, Baradaran-Rafii A, Hashemian SJ, et al. Comparison of three phakic intraocular lenses for correction of myopia. J Ophthalmic Vis Res. 2014;9(4):427–433. doi:10.4103/2008-322X.150805
6. Bohac M, Anticic M, Draca N, et al. Comparison of verisyse and veriflex phakic intraocular lenses for treatment of moderate to high myopia 36 months after surgery. Semin Ophthalmol. 2017;32(6):725–733. doi:10.3109/08820538.2016.1170163
7. Chelbi S, Rabilloud M, Burillon C, Kocaba V. Corneal endothelial tolerance after iris-fixated phakic intraocular lens implantation: a model to predict endothelial cell survival. Cornea. 2018;37(5):591–595. doi:10.1097/ICO.0000000000001527
8. Budo C, Hessloehl JC, Izak M, et al. Multicenter study of the artisan phakic intraocular lens. J Cataract Refract Surg. 2000;26:1163–1171. doi:10.1016/S0886-3350(00)00545-9
9. Benedetti S, Casamenti V, Marcaccio L, Brogioni C, Assetto V. Correction of myopia of 7 to 24 diopters with the artisan phakic intraocular lens: two-year follow-up. J Refract Surg. 2005;21(2):116–126. doi:10.3928/1081-597X-20050301-05
10. Tahzib NG, Nuijts RM, Wu WY, Budo CJ. A long-term study of artisan phakic intraocular lens implantation for the correction of moderate to high myopia: ten-year follow-up results. Ophthalmology. 2007;114:1133–1142. doi:10.1016/j.ophtha.2006.09.029
11. Landesz M, Worst JG, van Rij G. Long-term results of correction of high myopia with an iris-claw phakic intraocular lens. J Refract Surg. 2000;16:310–316.
12. Silva RA, Jain A, Manche EE. Prospective long-term evaluation of the efficacy, safety, and stability of the phakic intraocular lens for high myopia. Arch Ophthalmol. 2008;126:775–781. doi:10.1001/archopht.126.6.775
13. Jonker SMR, Berendschot TTJM, Ronden AE, Saelens IEY, Bauer NJC, Nuijts RMMA. Long-Term endothelial cell loss in patients with artisan myopia and artisan toric phakic intraocular lenses. 5- and 10-year results. Ophthalmology. 2018;125(4):486–494. doi:10.1016/j.ophtha.2017.08.011
14. Dick HB, Budo C, Malecaze F, et al. Foldable artiflex phakic intraocular lens for the correction of myopia: two-year follow-up results of a prospective European multicenter study. Ophthalmology. 2009;116:671–677. doi:10.1016/j.ophtha.2008.12.059
15. Nassiri N, Ghorbanhosseini S, Jafarzadehpur E, Kavousnezhad S, Nassiri N, Sheibani K. Visual acuity, endothelial cell density and, polymegathism after iris-fixated lens implantation. Clin Ophthalmol. 2018;12:601–605. doi:10.2147/OPTH.S157501
16. Sachdev G, Ramamurthy D. Long-term safety of posterior chamber implantable phakic contact lens for the correction of myopia. Clin Ophthalmol. 2019;13:137–142. doi:10.2147/OPTH
17. Moya T, Javaloy J, Montés-Micó R, Beltrán J, Muñoz G, Montalbán R. Implantable collamer lens for myopia: assessment 12 years after implantation. J Refract Surg. 2015;31(8):548–556. doi:10.3928/1081597X-20150727-05
18. Dejaco-Ruhswurm I, Scholz U, Pieh S, et al. Long-term endothelial changes in phakic eyes with posterior chamber intraocular lenses. J Cataract Refract Surg. 2002;28:1589–1593. doi:10.1016/S0886-3350(02)01210-5
19. Sayman Muslubas IB, Cabi C, Aydin Oral AY, et al. Comparison of outcomes of posterior chamber and iris-claw anterior chamber phakic intraocular lens implantation for moderate to high myopia. J Clin Exp Ophthalmol. 2013;4:263–267.
20. Marcon GB, Galan A, Rappo G, Altafini R, Zanotto D, Carlentini S. Edematous decompensation of the cornea after silicon implant of the posterior chamber in phakic eyes in myopia. J Fr Ophtalmol. 1996;19(2):149–152.
21. Kohen T, Kook D, Morral M, Guell JL. Phakic intraocular lenses: part 2: results and complications. J Cataract Refract Surg. 2010;36(12):2168–2194. doi:10.1016/j.jcrs.2010.10.007
22. Edelhauser HF, Sanders DR, Azar R, Lamielle H; ICL in Treatment of Myopia Study Group. Corneal endothelial assessment after ICL implantation. J Cataract Refract Surg. 2004;30:576–583. doi:10.1016/j.jcrs.2003.09.047
23. Morphis G, Irigoyen C, Eleuteri A, Stappler T, Pearce I, Heimann H. Retrospective review of 50 eyes with long-term silicone oil tamponade for more than 12 months. Graefes Arch Clin Exp Ophthalmol. 2012;250(5):645–652. doi:10.1007/s00417-011-1873-8
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.