Back to Journals » Clinical Ophthalmology » Volume 10
Therapeutic effect of dexamethasone implant in retinal vein occlusions resistant to anti-VEGF therapy
Authors Wallsh J , Sharareh B, Gallemore R
Received 30 January 2016
Accepted for publication 8 March 2016
Published 25 May 2016 Volume 2016:10 Pages 947—954
DOI https://doi.org/10.2147/OPTH.S105412
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Josh Wallsh, Behnam Sharareh, Ron Gallemore
Retina Macula Institute, Torrance, CA, USA
Purpose: To test the efficacy of the intravitreal dexamethasone (DEX) implant in patients with retinal vein occlusions (RVOs) who have failed multiple anti-vascular endothelial growth factor (anti-VEGF) treatments.
Methods: A randomized exploratory study of ten patients with branch RVO or central RVO who received at least two previous anti-VEGF treatments and had persistent or unresponsive cystoid macular edema. Treatment with the DEX implant was either every 4 months or pro re nata (PRN) depending on their group assignment for 1 year. Multifocal electroretinography and microperimetry were the primary end points, with high-resolution optical coherence tomography and best-corrected visual acuity as the secondary end points.
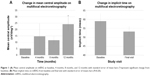
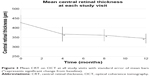
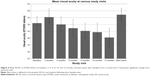
Results: All patients in both the every 4 month and PRN cohorts who completed the study received the three maximal injections of DEX; therefore, the data from both cohorts were combined and reported as a case series. On average, the multifocal electroretinography amplitude increased significantly from 5.11±0.66 to 24.19±5.30 nV/deg2 at 12 months (P<0.005), mean macular sensitivity increased from 7.67±2.10 to 8.01±1.98 dB at 4 months (P=0.32), best-corrected visual acuity increased significantly from 51.0±5.1 to 55.4±5.1 early treatment of diabetic retinopathy study letters at 2 months (P<0.05), and central retinal thickness decreased from 427.6±39.5 to 367.1±37.8 µm at 4 months (P<0.05). Intraocular pressure increased significantly in one patient, with that patient requiring an additional glaucoma medication for management. Additionally, cataract progression increased significantly (P<0.05) in this patient population and partially limited analysis of other end points.
Conclusion: DEX should be considered as a treatment option in patients with RVOs who have failed anti-VEGF therapy, as the results of this study demonstrated an improvement in retinal morphology and macular function. Cataract progression did occur following multiple consecutive injections; however, steroid-induced glaucoma was not a limiting factor.
Keywords: retinal vein occlusion, intravitreal dexamethasone implant, multifocal electroretinography, anti-VEGF, cataract progression
A Letter to the Editor has been received and published for this article.
Introduction
Macular edema may cause significant vision loss in retinal vein occlusions (RVOs).1,2 Current treatment modalities include focal laser photocoagulation,3,4 intravitreal anti-vascular endothelial growth factor (anti-VEGF),5–8 and intravitreal steroid injections.9–11 Repeated intravitreal anti-VEGF injections are now the preferred treatment for macular edema, but there is a subset of patients who fail to respond to such treatment or develop rebound edema.12,13 In such cases, an intravitreal steroid injection may be beneficial. A single administration of the US Food and Drug Administration approved 0.7 mg intravitreal dexamethasone (DEX) implant (Ozurdex; Allergan, Irvine, CA, USA) was shown to be effective at improving macular edema and visual acuity (VA) in a retrospective study of patients with RVO recalcitrant to anti-VEGF therapy.14 To date, no study has tested the efficacy of repeated DEX injections in the treatment of anti-VEGF-resistant macular edema associated with RVO.
For the present study, we determine the efficacy of multiple DEX injections on macular function and edema for patients diagnosed with RVO resistant to anti-VEGF therapy. Macular function was assessed using multifocal electroretinography (mfERG), microperimetry (MP), and optical coherence tomography (OCT).
Methods
Patient population
A randomized clinical trial was performed in a single retina center on patients diagnosed with central retinal vein occlusion (CRVO) or branch retinal vein occlusion (BRVO) who previously received at least two intravitreal anti-VEGF injections. Patients were required to have a central foveal thickness of at least 275 μm on OCT studies and best-corrected visual acuity (BCVA) between 3 and 72 letters based on the early treatment of diabetic retinopathy study (ETDRS) at screening visit. Patients were excluded if they had a history of steroid-induced glaucoma requiring more than one antiglaucoma medication for management. All patients gave written informed consent. Ethics approval was obtained from Western Institutional Review Board for the study protocol, and the study was registered on clinicaltrials.gov as NCT01449682. Support for this investigator-sponsored trial was provided by Allergan.
Study treatment and outcome measures
Patients were randomized by coin flip 1:1 to a treatment every 4 months (q4 months) group or a pro re nata (PRN) group to be treated based on the presence of macular edema on OCT as determined by the treating physician. Both groups received the 0.7 mg intravitreal DEX at each treatment utilizing the following injection protocol: topical proparacaine application and a drop of betadine placed into the inferior fornix followed by a subconjunctival 2% lidocaine injection. Subsequently, another drop of betadine was applied to the inferior fornix followed by inferotemporal injection of the DEX implant 4 mm posterior to the limbus. All enrolled patients were treated at their baseline visit. Patients were followed-up for 1 year at 4-month intervals, receiving a maximum of three DEX injections. For the PRN group, decision to treat was made at the 4-month interval visits only. The primary outcome measures assessed at baseline and every 4 months thereafter were mean central amplitude on mfERG (UTAS-E300; LKC Technologies, Gaithersburg, MD, USA) and mean macular sensitivity on MP (MP-1 microperimeter; Nidek Technologies, Padova, Italy). The mean central amplitude was determined based on the difference in the first positive peak (P1) and first negative peak (N1) from the central hexagon on mfERG. In addition, the secondary outcome measures assessed were BCVA in ETDRS letters and central retinal thickness (CRT) on OCT studies. All OCT imaging was performed on a Cirrus high-definition OCT (Cirrus HD-OCT; Carl Zeiss Meditec, Dublin, CA, USA), with calculations of CRT determined using macular thickness maps based on the average of the central five ETDRS subfields surrounding the fovea. Complications such as increased intraocular pressure (IOP) and cataract progression were assessed at baseline and every 4 months thereafter. Intermediate visits were performed every 2 months after an injection, with BCVA and IOP measurements and examination.
Statistical analysis
Cataract progression obscured the view for OCT and MP studies in certain circumstances, precluding the ability to measure CRT and mean macular sensitivity, respectively. Data analysis for OCT and MP studies under these circumstances and for patients lost to follow-up were handled using a last observation carried forward technique. For all study outcomes, the q4 months and PRN groups were compared using Student’s t-test and considered significant for P-values <0.05. At the conclusion of the study, it was noted that all patients in both the q4 months and PRN groups received the maximal therapy of three DEX injections; therefore, analysis of the combined cohorts was performed using paired Student’s t-test and considered significant for P-values <0.05.
Results
Ten patients (nine BRVO, one CRVO) with an average age of 66.2±4.7 years were enrolled. All but one enrolled patient received the maximum of three DEX injections, a single patient in the q4 months group died after receiving two implants (Table 1). Another patient from the PRN group was removed from the study following the 10-month visit (after receiving all three treatments) because of severe cataracts and need for urgent surgery. Between the q4 months and PRN groups, baseline characteristics demonstrated significantly lower values for mean central amplitude and macular sensitivity and significantly higher values for CRT in the PRN group. There was no significant difference in the percent change in mean central amplitude, macular sensitivity, or BCVA from baseline to final visit. However, percent change in CRT was significantly greater in the PRN group, 27.9%, than the q4 months group, 7.0% (P<0.05) (Table 2).
This exploratory study was designed as a small randomized controlled clinical trial. In the end, however, the limited number of patients did not allow enough statistical power to analyze the randomized and control groups separately. In addition, the two groups underwent the same treatments – all patients who completed the study received the equivalent number of implants at 4-month intervals. Thus, the data were combined and reported as a case series. For all eyes, mean central amplitude measurements on mfERG increased for 90% (n=9) of eyes when comparing their final value to baseline value. The average mean central amplitude in all studied eyes improved significantly from baseline to 12 months from 5.11±0.66 to 24.19±5.30 nV/deg2, respectively (P<0.05) (Figure 1A). Implicit time to N1 decreased for seven (70%) patients, with a mean decrease in duration for all studied eyes from 59.0±4.3 to 53.2±2.8 msec (P=0.20) (Figure 1B).
Mean macular sensitivity measured with MP increased at 4 months, following a single treatment, from 7.7±2.1 to 8.0±2.0 dB (P=0.32), but decreased at the final visit to 7.5±1.6 dB (P=0.42) (Figure 2).
  | Figure 2 Mean macular sensitivity on MP at baseline, 4 months, and final visit with standard error of mean bars. |
A decrease in CRT on OCT studies was appreciated in 90% (n=9) of eyes when comparing their final image to the baseline measurement. The mean CRT improved following each DEX injection, with a significant improvement (P<0.05) following the first treatment from 427.6±39.5 to 367.1±37.8 μm. Throughout the course of the study, the mean CRT continued to decrease, and at the 12-month visit reached a thickness of 344.0±25.1 μm, which was significant when compared with baseline (P<0.05) (Figure 3).
Following a single treatment, at the 2-month interval visit, an increase in VA was observed in six (60%) patients, with a significant mean improvement for all patients from 51.0±5.1 to 55.4±5.1 ETDRS letters (P<0.05). Thereafter, ETDRS chart results steadily decreased to a final value of 40.5±7.0 letters (Figure 4).
Tables 3 and 4 detail the commonly expected complications associated with DEX. Mean IOP increased subtly over the 1-year series, with peaks witnessed at 2 months following each treatment. There was only a single incidence of IOP increase of >10 mmHg requiring an additional glaucoma topical medication for management (Table 3). Cataract progression was noted in six of seven (85.7%) phakic patients with a significant increase (P<0.05) in grading for nuclear sclerotic, cortical, and posterior subcapsular cataracts from baseline to final visit (Table 4).
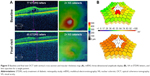
Baseline and final visit macular cross-sections, macular thickness maps, mfERG, BCVA in ETDRS letters, and cataract assessment are shown for a single studied eye demonstrating the response associated with the treatment protocol in Figure 5.
Discussion
In this randomized exploratory study, we found that consecutive DEX injections for macular edema resistant to anti-VEGF injections in patients with RVO significantly improved macular function as assessed with mfERG testing. This improvement correlated well with the improvement in macular edema.
PRN and q4 months groups
Comparison of the PRN and q4 months groups revealed baseline characteristics that were significantly worse for the PRN group (Table 2). Not surprisingly, all patients in the PRN group required three DEX injections. Percent change comparisons from baseline to final visit alone demonstrated a significant difference in CRT, with the PRN group showing greater decrease than the q4 months group. Given these results and that both groups were treated equivalently with DEX injections every 4 months, there were few conclusions to be drawn from cohort comparisons. However, this allowed combined analysis of all enrolled patients to assess the response to consecutive DEX injections over time.
mfERG and OCT
There are limited prior reports on the effect of DEX injections on mfERG. Querques et al15 reported 12 patients diagnosed with CRVO who received a single DEX injection. These patients were found to have an insignificant improvement in central amplitude at 1 and 3 months following treatment.15 In our study, a significant improvement in mean central amplitude from 5.11±0.66 to 24.19±5.30 nV/deg2 was witnessed following three DEX injections along with a decrease in implicit time from 59.0±4.3 to 53.2±2.8 msec. A shorter implicit time also indicates improved retinal function. Most traditional measures of retinal function can become severely diminished by anterior segment pathology, such as cataract progression in the case of steroid management.16,17 Although cataracts can influence mfERG results,18,19 we show that this effect is overwhelmed by the vast improvement that multiple DEX injections can have on anti-VEGF-resistant RVOs. To our knowledge, we are the first to present mfERG results following DEX injections in patients with BRVO.
In patients with RVO, much of the vision loss has been attributed to the development of macular edema from the hypoxic state and promotion of VEGF.20,21 In a previous study, we demonstrated a decrease in central foveal thickness from 423.7±27.9 to 277.0±33.7 μm in 18 patients with RVO resistant to anti-VEGF therapy following a single DEX injection.14 The ten patients in our study witnessed a similar significant improvement in mean CRT from 427.6±39.5 to 344.0±25.1 μm following an average of 2.9 implants. Although assessment with OCT imaging has commonly been used to monitor response to treatment in patients with RVO, the associated improvement in retinal morphology may fail to demonstrate underlying damage from prolonged edema. Therefore, combining mfERG, which can demonstrate damage to outer retinal layers,22,23 with OCT imaging can provide a better understanding of the functional implications of morphological improvement following treatment of macular edema,24–26 we demonstrated significant improvements in both, indicating that macular function did indeed improve dramatically concomitant with the improvement in macular edema.
Cataract progression, VA, and MP
Although previous studies of DEX have demonstrated this class of steroid as less toxic to the lens than alternative steroid injections, including triamcinolone and fluocinolone acetonide,27,28 cataract formation nonetheless occurs. Haller et al10 reported cataract progression in 7.6% and 29.8% of phakic eyes with RVO treated with 0.7 mg intravitreal DEX implants every 6 months following one or two treatments, respectively. In 2013, Mayer et al29 treated eyes with RVO as needed with DEX for 1 year and noted cataract progression in 59.6% (n=31) of phakic eyes. In the present study, six of seven phakic eyes (86.7%) developed a significant increase in nuclear sclerotic, cortical, and posterior subcapsular cataracts. The only patient who did not have cataract progression was the youngest enrolled patient and the only patient under 50 years old. This level of cataract progression is more pronounced than the previously reported studies, which may be due to the more frequent administration of DEX in the present study. This has implications for current clinical practice because patients often require treatment for a year or more for macular edema associated with RVO, and we can expect a higher incidence of cataract progression in clinical practice than reported in the initial RVO studies of DEX. Patients must be informed of this high probability of clinically significant cataract progression before embarking on a course of treatment.
The unexpectedly significant progression of all forms of cataracts resulted in an associated diminishment in VA and MP values. Previous studies of eyes with RVO have demonstrated significant improvements in VA following treatment with DEX.10,15 In 2013, we reported a 0.17 logMAR improvement in VA following a single DEX injection in 18 eyes diagnosed with RVO resistant to anti-VEGF therapy.14 Similarly, in our current study, an immediate increase in VA was appreciated after 2 months from 51.0±5.1 to 55.4±5.1 ETDRS letters, but eventually decreased to 40.5±7.0 letters at the final visit. Given the extent of cataract progression, limited conclusions can be drawn from the final VA results without following up with these patients after cataract surgery; however, this was outside of the scope of this study. It is important to note that the one phakic patient without noted cataract progression showed an eight-letter increase in ETDRS letters (Figure 5).
MP has been used before to assess retinal function after treatment for RVO.30,31 Recently, Querques et al15 demonstrated a significant improvement in mean sensitivity in 12 CRVO patients 3 months after a single DEX injection from 9.6±4.3 to 11.0±5.7 dB. Similarly, an increase in mean sensitivity was seen in our study population following a single treatment from 7.7±2.1 to 8.0±2.0 dB. However, following additional treatments, mean sensitivity diminished to a final value of 7.5±1.6 dB, which was essentially unchanged from baseline. This result may also be correlated to cataract progression, as Richter-Mueksch et al32 demonstrated a 1 dB decrease in mean sensitivity associated with each point of lens opacity.
IOP
Ocular steroid treatments have commonly been associated with elevations in IOP and steroid-induced glaucoma.33,34 Haller et al10 reported an incidence of an IOP increase of >10 mmHg in 32.8% of patients treated with two DEX injections over 1 year. Within the first 6 months of that study, following a single DEX injection, 25.0% of patients required the addition of glaucoma medication and an additional 10.3% of patients required medical management following retreatment with a second DEX injection during the next 6 months.10 Overall, the repeated DEX injections in our study were well tolerated with only one (10%) patient having a single incidence of IOP increase of >10 mmHg. This patient was the only patient requiring one additional glaucoma medication for IOP management during our study. However, we excluded patients from our study who were on more than one glaucoma medication, so we may have preselected patients at a lower risk of developing secondary glaucoma.
Conclusion
Our study is limited by its size; with only ten patients, strong conclusions are difficult to establish. In addition, the failure of a positive response in one of our primary outcomes, MP, is another limitation. Given the severity of cataract progression, it is difficult to draw strong conclusions from either the MP or VA results. Finally, although eyes with either CRVO or BRVO were included in our study design, only one eye with CRVO was recruited, and individual studies analyzing each entity separately would be required to ascertain response differences between the two subgroups of RVO. Even with these limitations, our significant improvements in mfERG and macular edema demonstrate that the intravitreal DEX implant can improve retinal morphology and function in anti-VEGF-resistant cases. Thus, intravitreal DEX implants should be considered in such patients, although further research with a larger cohort of pseudophakic patients is warranted.
Acknowledgments
Financial support for this study was provided by Allergan, Irvine, CA, USA. The sponsor or funding organization had no role in the design or conduct of this research. The results of this study have been presented at American Society of Retina Specialists, Toronto, ON, USA, August 2013 and American Academy of Ophthalmology, New Orleans, LA, USA, November 2013.
Disclosure
The authors report no conflicts of interest in this work.
References
Rogers SL, McIntosh RL, Lim L, et al. Natural history of branch retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117(6):1094–1101. | ||
McIntosh RL, Rogers SL, Lim L, et al. Natural history of central retinal vein occlusion: an evidence-based systematic review. Ophthalmology. 2010;117(6):1113.e15–1123.e15. | ||
[No authors listed] A randomized clinical trial of early panretinal photocoagulation for ischemic central vein occlusion. The Central Vein Occlusion Study Group N report. Ophthalmology. 1995;102(10):1434–1444. | ||
The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol. 1984;98:271–282. | ||
Campochiaro PA, Heier JS, Feiner L, et al. Ranibizumab for macular edema following branch retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010;117(6):1102–1112. | ||
Brown DM, Campochiaro PA, Singh RP, et al. Ranibizumab for macular edema following central retinal vein occlusion: six-month primary end point results of a phase III study. Ophthalmology. 2010;117(6):1124–1133. | ||
Prager F, Michaels S, Kriechbaum K, et al. Intravitreal bevacizumab (Avastin) for macular edema secondary to retinal vein occlusion: 12-month results of a prospective clinical trial. Br J Ophthalmol. 2009;93(4):452–456. | ||
Boyer D, Heier J, Brown DM, et al. Vascular endothelial growth factor Trap-Eye for macular edema secondary to central retinal vein occlusion: six-month results of the phase 3 COPERNICUS study. Ophthalmology. 2012;119(5):1024–1032. | ||
SCORE Study Research Group. A randomized trial comparing the efficacy and safety of intravitreal triamcinolone with standard care to treat vision loss associated with macular edema secondary to branch retinal vein occlusion: the Standard Care vs Corticosteroid for Retinal Vein Occlusion (SCORE) study report 6. Arch Ophthalmol. 2009;127(9):1115–1128. | ||
Haller JA, Bandello F, Belfort R Jr, et al. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion: twelve-month study results. Ophthalmology. 2011;118(12):2453–2460. | ||
Haller JA, Bandello F, Belfort R Jr, et al. Randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with macular edema due to retinal vein occlusion. Ophthalmology. 2010;117(6):1134–1146. | ||
Matsumoto Y, Freund KB, Peiretti E, et al. Rebound macular edema following bevacizumab (Avastin) therapy for retinal venous occlusive disease. Retina. 2007;27(4):426–431. | ||
Yasuda S, Kondo M, Kachi S, et al. Rebound of macular edema after intravitreal bevacizumab therapy in eyes with macular edema secondary to branch retinal vein occlusion. Retina. 2011;31(6):1075–1082. | ||
Sharareh B, Gallemore R, Taban M, Onishi S, Wallsh J. Recalcitrant macular edema after intravitreal bevacizumab is responsive to an intravitreal dexamethasone implant in retinal vein occlusion. Retina. 2013;33(6):1227–1231. | ||
Querques G, Lattanzio R, Querques L, et al. Impact of intravitreal dexamethasone implant (Ozurdex) on macular morphology and function. Retina. 2014;34(2):330–341. | ||
Bambo MP, Garcia-Martin E, Otin S, et al. Influence of cataract surgery on repeatability and measurements of spectral domain optical coherence tomography. Br J Ophthalmol. 2014;98(1):52–58. | ||
Kim NR, Lee H, Lee ES, et al. Influence of cataract on time domain and spectral domain optical coherence tomography retinal nerve fiber layer measurements. J Glaucoma. 2012;21(2):116–122. | ||
Wordehoff UV, Palmowski AM, Heinemann-Vernaleken B, Allgayer R, Ruprecht KW. Influence of cataract on the multifocal ERG recording – a pre- and postoperative comparison. Doc Ophthalmol. 2004;108(1):67–75. | ||
Tam WK, Chan H, Brown B, et al. Comparing the multifocal electroretinogram topography before and after cataract surgery. Curr Eye Res. 2005;30(7):593–599. | ||
Karia N. Retinal vein occlusion: pathophysiology and treatment options. Clin Ophthalmol. 2010;4:809–816. | ||
Wang P, Zhu F, Konstantopoulos K, et al. Prostaglandin E2 induces interleukin-6 expression in human chondrocytes via cAMP/protein kinase A- and phosphatidylinositol 3-kinase-dependent NF-κB activation. Am J Physiol Cell Physiol. 2010;298(6):C1445–C1456. | ||
Hood DC. Assessing retinal function with the multifocal technique. Prog Retin Eye Res. 2000;19(5):607–646. | ||
Hood DC, Frishman LJ, Saszik S, Viswanathan S. Retinal origins of the primate multifocal ERG: implications for the human response. Invest Ophthalmol Vis Sci. 2002;43(5):1673–1685. | ||
Yip VW, Ngai JW, Fok AC, et al. Correlation between functional and anatomical assessments by multifocal electroretinography and optical coherence tomography in central serous chorioretinopathy. Doc Ophthalmol. 2010;120(2):193–200. | ||
Shetty R, Pai SA, Vincent A, et al. Electrophysiological and structural assessment of the central retina following intravitreal injection of bevacizumab for treatment of macular edema. Doc Ophthalmol. 2008;116(2):129–135. | ||
Moschos MM, Moschos M. Intraocular bevacizumab for macular edema due to CRVO. A multifocal-ERG and OCT study. Doc Ophthalmol. 2008;116(2):147–152. | ||
Arcinue CA, Cerón OM, Foster CS. A comparison between the fluocinoclone acetonide (Retisert) and dexamethasone (Ozurdex) intravitreal implants in uveitis. J Ocul Pharmacol Ther. 2013;29(5):501–507. | ||
Lee J, Freeman WR, Azen SP, et al. Prospective, randomized clinical trial of intravitreal triamcinolone treatment of neovascular age-related macular degeneration: one-year results. Retina. 2007;27(9):1205–1213. | ||
Mayer WJ, Wolf A, Kernt M, et al. Twelve-month experience with Ozurdex for the treatment of macular edema associated with retinal vein occlusion. Eye. 2013;27(7):816–822. | ||
Yamaike N, Tsujikawa A, Sakamoto A, et al. Retinal sensitivity after intravitreal injection of bevacizumab for the treatment of macular edema secondary to retinal vein occlusion. Retina. 2009;29(6):757–767. | ||
Winterhalter S, Lux A, Maier AK, et al. Microperimetry as a routine diagnostic test in the follow-up of retinal vein occlusion? Graefes Arch Clin Exp Ophthalmol. 2012;250(2):175–183. | ||
Richter-Mueksch S, Sacu S, Weingessel B, Vécsei-Marlovits VP, Schmidt-Erfurth U. The influence of cortical, nuclear, subcortical posterior, and mixed cataract on the results of microperimetry. Eye (Lond). 2011;25(10):1317–1321. | ||
Razeghinejad MR, Katz LJ. Steroid-induced iatrogenic glaucoma. Ophthalmic Res. 2012;47(2):66–80. | ||
Mahar PS, Mermon AS. Frequency and management of raised intraocular pressure following intravitreal triamcinolone acetonide. J Coll Physicians Surg Pak. 2012;22(11):699–702. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.