Back to Journals » Clinical Interventions in Aging » Volume 10
The predictive capacity and additional prognostic power of N-terminal pro-B-type natriuretic peptide in Chinese elderly with chronic heart failure
Authors Fu S, Xie L, Li D, Ye P, Luo L
Received 12 November 2014
Accepted for publication 9 December 2014
Published 27 January 2015 Volume 2015:10 Pages 359—365
DOI https://doi.org/10.2147/CIA.S77417
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Zhi-Ying Wu
Shihui Fu,1,2,* Leixing Xie,2,* Dongyun Li,1,2 Ping Ye,1 Leiming Luo1
1Department of Geriatric Cardiology, 2Department of Cardiology and Hainan Branch, Chinese People’s Liberation Army General Hospital, Beijing, People’s Republic of China
*These authors are joint first authors
Objective: This study was conducted to research the prognostic utility of N-terminal pro-B-type natriuretic peptide (NT-proBNP), compare the utility of the Seattle Heart Failure Score (SHFS) with NT-proBNP, develop a risk-evaluation model based on NT-proBNP, assess the associations of NT-proBNP with patient characteristics, and screen for decisive factors of NT-proBNP in Chinese elderly with chronic heart failure (CHF).
Patients and methods: There were 306 patients (≥60 years) with CHF chosen as study subjects. Each one received an assessment of NT-proBNP on serum. The end point was all-cause mortality during a mean follow-up period of 471 days.
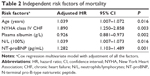
Results: Subjects had a median age of 85 (60–100) years, a median NT-proBNP of 1,743.4 pg/mL, and a median SHFS of 1.87. During the follow-up period, 104 deaths occurred. NT-proBNP was significantly related to mortality (odds ratio 1.603, 95% confidence interval 1.407–1.826; P<0.001) and the significance persisted after full adjustment (odds ratio 1.282, 95% confidence interval 1.103–1.489; P=0.001). Age, New York Heart Association class IV CHF, plasma albumin, and neutrophils/lymphocytes were also independent predictors for mortality (P<0.05 for all). NT-proBNP and the SHFS showed similar predictive capacities (0.736 versus 0.796, P=0.105). The addition of NT-proBNP to the SHFS (0.818 versus 0.796, P=0.168) generated marginal growth in the c-statistic. The model based on NT-proBNP consisting of all selected predictors in this study, including age, New York Heart Association class IV CHF, plasma albumin, neutrophils/lymphocytes, and NT-proBNP, had a moderately higher c-statistic compared with the SHFS (0.846 versus 0.796, P=0.066). NT-proBNP was bound with the SHFS (r=0.500, P<0.001). Characteristics regarding general condition, inflammation, and cardiac and renal function were the decisive factors of NT-proBNP (P<0.05 for all).
Conclusion: As a comprehensive representation of the patient characteristics described earlier, NT-proBNP values provided significant prognostic power similar to the SHFS in Chinese elderly with CHF. A novel model based on NT-proBNP could offer help for risk stratification.
Keywords: NT-proBNP, prognosis, chronic heart failure, elderly
Introduction
The elderly represent a growing proportion of patients with chronic heart failure (CHF), and CHF is a leading source of morbidity and mortality in the elderly.1,2 Accurate prognostic evaluation of elderly with CHF is an increasingly important clinical goal for physicians. Current understanding of the risk factors for survival of the elderly with CHF has been derived largely from former studies, which mainly focused on traditional risk factors and did not aim directly at contemporary elderly. Moreover, ethnicity plays a significant role in prognostic evaluation of elderly with CHF, and the same risk factors might have different influences on mortality, due to ethnicity disparities. Specific and newer risk factors for contemporary elderly have been less thoroughly investigated, especially in the People’s Republic of China.
N-terminal pro-B-type natriuretic peptide (NT-proBNP) is recognized as a prognostically meaningful biomarker in patients with CHF.3,4 However, few investigators have attempted to make use of NT-proBNP values to assess the risk of elderly with CHF.5 The Seattle Heart Failure Score (SHFS) has been developed to determine the risk of dying, and has been validated as a useful tool in estimating CHF mortality in several data sets.6 Whether NT-proBNP values have similar or superior predictive capacities compared to the SHFS is uncertain.7 In addition, the novel risk-evaluation model combining NT-proBNP values and other significant risk factors is more likely to provide better prognostic evaluation of patients with CHF. Meanwhile, for the convenience of a better understanding of the prognostic information of NT-proBNP values, their correlations with traditional risk factors have received attention.
To address these issues, the purposes of the current analysis were the following: 1) to research the prognostic utility of NT-proBNP values, compare the utility of the SHFS with NT-proBNP values, and tentatively develop the risk-evaluation model based on NT-proBNP values in older Chinese patients with CHF; and 2) to assess the associations between NT-proBNP values and characteristics of older Chinese patients with CHF and screen for decisive factors of NT-proBNP values.
Patients and methods
Study population
There were 306 older patients (≥60 years) chosen as study subjects. They had long-standing symptoms (dyspnea and/or fatigue), signs (edema and/or pulmonary rales), and abnormalities of cardiac structure or function, and was diagnosed with CHF by chief physicians or associate chief physicians according to European Society of Cardiology (ESC) 2008 guidelines.8 Each patient received an assessment of serum NT-proBNP. Excluded from the current analysis were patients with severe aortic stenosis, anticipated cardiac transplantation, and left ventricular assist devices. The Chinese People’s Liberation Army General Hospital was their designated hospital and held their integrated long-term medical and death records, which made it easier for us to follow them up effectively and judge end points accurately.
Physical measurements
Baseline characteristics were collected from all patients after admission to the Chinese People’s Liberation Army General Hospital, and the measurements were completed by physicians who were well trained by the research team. Body mass index (BMI) was defined as weight in kilograms divided by the square of height in meters. Mean systolic blood pressure (MSBP) and mean diastolic blood pressure (MDBP) were the averages of five separate measurements. Standardized echocardiography was performed. Left ventricular ejection fraction was measured by Simpson’s method. Left ventricular mass was calculated as 0.80×1.04× ([IVST + LVPWTd + LVDd]3 – LVDd3) +0.60, and was indexed to body surface area ([m2=0.0061×height [cm] +0.0128× weight [kg] – 0.153) to compute the left ventricular mass index.
Biochemical analyses
Blood assays were carried out at the central laboratory in the Department of Biochemistry, Chinese People’s Liberation Army General Hospital. The technicians who performed the tests were blinded to the clinical data of the subjects. Serum NT-proBNP values were measured by the NT-proBNP Flex Reagent Cartridge (PBNP/LPBN), produced by Siemens Healthcare Diagnostics, on the Dimension RXL Max (AMR 10–30,000 pg/mL). Estimated glomerular filtration rate (eGFR) was calculated by a modified Modification of Diet in Renal Disease (MDRD) equation based on data from Chinese patients: 175× serum creatinine (mg/dL)−1.234 × age (years)−0.179 ×0.79 (if female).9
Definitions
Acute myocardial infarction and atrial fibrillation (AF) were defined on the grounds of the universal definition of myocardial infarction and the American College of Cardiology/American Heart Association/ESC 2006 guidelines for AF.10,11 Subjects with MSBP ≥140 mmHg, MDBP ≥90 mmHg, or receiving medication for treatment of hypertension were defined as having hypertension, and with fasting glucose concentration ≥7 mmol/L or treatment with an oral hypoglycemic agent/insulin as having diabetes mellitus. Metabolic syndrome was determined as the presence of at least three of the following criteria of the Chinese Diabetes Society: 1) BMI ≥25 kg/m2; 2) triglycerides ≥1.7 mmol/L; 3) high-density lipoprotein cholesterol <0.9 mmol/L in men and <1.0 mmol/L in women; 4) MSBP ≥140 mmHg or MDBP ≥90 mmHg; and 5) fasting glucose concentration ≥6.1 mmol/L. Smoking status was categorized as current, former, and never. Subjects were considered to be current smokers if they had smoked one or more cigarettes per day for the last year. Former smoking was defined as a history of cigarette consumption on a regular basis (one or more cigarettes per day), but no current smoking.
End point
Given the obviously high incidence of multiple organ failure in the elderly, as well as the priority of all-cause mortality in outcome studies, the end point assessed in the current analysis was all-cause death. The study population had a mean follow-up period of 471 days (median 342 days). Follow-up data were obtained from a review of medical records and telephone contact. No patients were lost to follow-up. Death was ascertained from the death record, a legal document including time, site, and other information.
Calculation of the score
The SHFS was derived in the PRAISE1 database, and provided an estimate of survival of patients with CHF.6 The hazard ratios for certain CHF medications in the SHFS could not be effectively estimated in PRAISE1, because of either widespread or rare use, and were results directly from prior clinical trials. They might not be generalizable to a wider population with CHF, and were abandoned in the current analysis.6
Statistical methods
Continuous variables were described using mean and standard deviation for variables with normal distribution and by median and interquartile range for nonnormally distributed variables. Categorical data were expressed as number and percentage of total. NT-proBNP values were logarithmically transformed to meet the multinormality assumption. In order to test prognostic abilities of NT-proBNP values and other risk factors for mortality, covariates with P<0.10 were picked up by Cox regression univariate analysis and taken into a Cox regression multivariate model with death as the dependent variable. Survival curves were generated by means of Kaplan–Meier estimates. The added predictive abilities of NT-proBNP values to the SHFS regarding mortality were investigated by comparison of areas under the curve (c-statistics) between the score and score + NT-proBNP values. Correlations between NT-proBNP values and other variables were determined by Pearson’s or Spearman’s correlation coefficients, and covariates with P<0.10 were taken into a multiple linear regression analysis to decide independent determinants of NT-proBNP values. A two-tailed P-value of less than 0.05 was considered to be statistically significant. All information on the characteristics of patients was entered into the database by trained abstractors and checked by other independent abstractors. SPSS 17 (SPSS, Chicago, USA) and MedCalc 9.6 for Windows (MedCalc Software, Mariakerke, Belgium) were used as the statistical systems.
Results
The whole cohort had a median age of 85 (60–100) years, a median NT-proBNP value of 1,743.4 pg/mL, and a median SHFS of 1.87. Patient characteristics for all patients are given in Table 1. During the follow-up period, 104 deaths occurred (34% of the whole cohort). NT-proBNP values were significantly related to all-cause death (hazard ratio 1.603, 95% confidence interval 1.407–1.826; P<0.001) and the significance persisted (hazard ratio 1.282, 95% confidence interval 1.103–1.489; P=0.001) after adjusting for all the factors in Table 1. In addition to NT-proBNP values, other factors, including age, New York Heart Association class IV CHF, plasma albumin, and neutrophils/lymphocytes, were also independent predictors for mortality (P<0.05 for all). The unadjusted influences of NT-proBNP values and other variables on mortality are displayed in Table 1. The independent prognostic abilities of NT-proBNP values and other predictors for mortality are provided in Table 2.Meanwhile, Kaplan–Meier estimates of survival for all subjects according to the quartile of NT-proBNP values are shown in Figure 1.
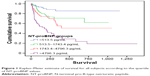  | Figure 1 Kaplan–Meier estimate of survival for all subjects according to the quartile of NT-proBNP values. |
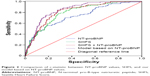
Table 3 demonstrates that NT-proBNP values and the SHFS showed similar predictive capacities (0.736 versus 0.796, P=0.105). The addition of NT-proBNP values to the SHFS (0.818 versus 0.796, P=0.168) generated a marginal growth in the c-statistic (Figure 2). The model based on NT-proBNP values consisting of all selected predictors in the current analysis, including age, New York Heart Association class IV CHF, plasma albumin, neutrophils/lymphocytes, and NT-proBNP values, had a moderately higher c-statistic compared with the SHFS (0.846 versus 0.796, P=0.066).
NT-proBNP values were bound with the SHFS (r=0.500, P<0.001). The univariate correlations of NT-proBNP values with patient characteristics are shown in Table 1. The multivariate regression model indicated that NT-proBNP values were positively linked to acute myocardial infarction, New York Heart Association class IV CHF, AF, C-reactive protein, left ventricular mass index, and right atrial diameter (P<0.05 for all). In turn, there was negative relevance of NT-proBNP values with BMI, MDRD-eGFR, plasma albumin, and ejection fraction (P<0.05 for all). The independent factors associated with NT-proBNP values are listed in Table 4.
Discussion
The current analysis demonstrated that NT-proBNP values were independent predictors of outcome and predictive capacity was comparable between NT-proBNP values and the SHFS in Chinese elderly with CHF. Moreover, this analysis formulated a risk-evaluation model based on NT-proBNP values consisting of all selected predictors in the current analysis, including age, New York Heart Association class IV CHF, plasma albumin, neutrophils/lymphocytes, and NT-proBNP values. Finally, the relationships between NT-proBNP values and several clinical features of Chinese elderly with CHF were thoroughly evaluated.
NT-proBNP values have previously shown their predictive ability in general patients with CHF.3,4 One study tried to determine the effect of age on the short-term prognostic abilities of NT-proBNP values in elderly with CHF.12 However, its study population was restricted to Caucasians with a mean age of 73.1 years, and thus its results might not be suitable for very older patients of other ethnicities. The current analysis verified that NT-proBNP values carried independent prognostic information in Chinese elderly and very elderly with CHF. As a comprehensive representation of the decisive factors described earlier, the predictive power of NT-proBNP values was obvious in Chinese elderly with CHF.
The SHFS is a multimarker and validated model, developed to predict mortality in patients with CHF.6 NT-proBNP values have been observed to have similar or superior predictive capacities compared to the SHFS.7 However, there was no analogous study with Chinese elderly as the study population. In the current analysis, NT-proBNP values showed similar prognostic value with respect to the complex SHFS. The addition of NT-proBNP values to the SHFS resulted in a marginal improvement in risk assessment. Moreover, the model based on NT-proBNP values provided modestly superior predictive ability than the SHFS.
The current analysis demonstrated that in Chinese elderly with CHF, elevated NT-proBNP values reflected the abnormality of cardiac structure and function, as well as lesions of cardiac tissue. Additionally, the elevation of NT-proBNP values had an independent relationship with reduced renal clearance, which was in agreement with other studies.13 The degree to which increased NT-proBNP values tied to AF itself versus its comorbidities, such as left ventricular hypertrophy, was debated, and the current analysis suggests that AF itself had a direct association with NT-proBNP values.14 Moreover, we validated the results of other studies wherein BMI exerted an independently inverse relation with NT-proBNP values.5 The conclusion of the current analysis was in line with prior studies that hypoalbuminemia was independently related to NT-proBNP values. The current analysis showed that C-reactive protein was independently associated with elevated NT-proBNP values, and supported the relevance between NT-proBNP values and inflammation.15
Conclusion
The current analysis showed that as a comprehensive representation of general condition, inflammation, and cardiac and renal function, NT-proBNP values provided significant prognostic power similar to the SHFS in Chinese elderly with CHF. Moreover, a novel model based on NT-proBNP values could offer some help for risk stratification.
Acknowledgments
This study was supported by grants from the National Key Basic Research Project (2012CB517503 and 2013CB530804), the Health Special Scientific Research Subject of the Chinese People’s Liberation Army (12BLZ34), and the Clinical Scientific Research Project of the Chinese People’s Liberation Army General Hospital (2012FC-TSYS1021).
Disclosure
The authors report no conflicts of interest in this work.
References
Redfield MM, Jacobsen SJ, Burnett JC Jr, Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289(2):194–202. | ||
Menotti A, Mulder I, Nissinen A, Giampaoli S, Feskens EJ, Kromhout D. Prevalence of morbidity and multimorbidity in elderly male populations and their impact on 10-year all-cause mortality: the FINE study (Finland, Italy, Netherlands, Elderly). J Clin Epidemiol. 2001;54(7):680–686. | ||
Hartmann F, Packer M, Coats AJ, et al. Prognostic impact of plasma N-terminal pro-brain natriuretic peptide in severe chronic congestive heart failure: a substudy of the Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) trial. Circulation. 2004;110(13):1780–1786. | ||
Correale M, Totaro A, Greco C, Brunetti ND, Di Biase M. Natriuretic peptides in heart failure: where we are, where we are going. Intern Emerg Med. 2011;6(4):381. | ||
Frankenstein L, Remppis A, Nelles M. Relation of N-terminal pro-brain natriuretic peptide levels and their prognostic power in chronic stable heart failure to obesity status. Eur Heart J. 2008;29(21):2634–2640. | ||
Levy WC, Mozaffarian D, Linker DT, et al. The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation. 2006;113(11):1424–1433. | ||
Pfister R, Diedrichs H, Schiedermair A, et al. Prognostic impact of NT-proBNP and renal function in comparison to contemporary multi-marker risk scores in heart failure patients. Eur J Heart Fail. 2008;10(3):315–320. | ||
Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J. 2008;29(19):2388–2442. | ||
Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17(10):2937–2944. | ||
Ryan TJ, Antman EM, Brooks NH, et al. 1999 Update: ACC/AHA guidelines for the management of patients with acute myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol. 1999;34(3):890–911. | ||
Fuster V, Rydén LE, Cannom DS, et al. ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114(7):e257–e354. | ||
Frankenstein L, Clark AL, Goode K, et al. The prognostic value of individual NT-proBNP values in chronic heart failure does not change with advancing age. Heart. 2009;95(10):825–829. | ||
Fabbian F, De Giorgi A, Portaluppi F, Zuliani G. Relationship between N-terminal pro-B-type natriuretic peptide plasma levels and renal function evaluated with different formulae in older adult subjects admitted because of dyspnea. Gerontology. 2012;58(1):50–55. | ||
Knudsen CW, Omland T, Clopton P, et al. Impact of atrial fibrillation on the diagnostic performance of B-type natriuretic peptide concentration in dyspneic patients. J Am Coll Cardiol. 2005;46(5):838–844. | ||
Brueckmann M, Huhle G, Lang S, et al. Prognostic value of plasma N-terminal pro-brain natriuretic peptide in patients with severe sepsis. Circulation. 2005;112(4):227–234. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.