Back to Journals » International Journal of Nephrology and Renovascular Disease » Volume 13
Symptom Clusters in Patients with End-Stage Renal Disease Undergoing Hemodialysis
Authors Chaiviboontham S , Phinitkhajorndech N , Tiansaard J
Received 14 July 2020
Accepted for publication 16 September 2020
Published 28 October 2020 Volume 2020:13 Pages 297—305
DOI https://doi.org/10.2147/IJNRD.S271619
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pravin Singhal
Suchira Chaiviboontham, Noppawan Phinitkhajorndech, Juthamas Tiansaard
Ramathibodi School of Nursing, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok 10400, Thailand
Correspondence: Suchira Chaiviboontham
Ramathibodi School of Nursing, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok 10400, Thailand
Tel +66 873263979
Email [email protected]
Background: End-stage renal disease (ESRD) patients undergoing hemodialysis have to face many symptoms from disease progression and treatment. These symptoms cause suffering and affect physical, psychological, emotional, social, and spiritual of the patients, resulting in decreased quality of life and might increase the death rate of these patients. Therefore, the study of symptoms in ESRD patients undergoing hemodialysis will lead to effective symptom management and maximize benefits for the patients. The purpose of this study was to explore the symptom clusters of ESRD patients undergoing hemodialysis.
Materials and Methods: The sample of this descriptive study consisted of 150 ESRD patients undergoing hemodialysis from two dialysis centre of the university hospital and specialized kidney hospital in Bangkok. The instruments consisted of Personal Information Questionnaire (PIQ) and Dialysis Symptom Index-THAI (DSI-THAI). The data were analyzed by exploratory factor analysis.
Results: The 8 clusters of symptoms were found: 1) gastrointestinal, 2) musculoskeletal and fluid volume 3) neurological 4) irritation of the mucous membranes and skin 5) depression 6) sleep disturbance 7) sexual 8) anemic.
Conclusion: The results of this study can be raised awareness and used as the information for the health-care provider to develop the intervention to manage unpleasant symptoms which lead to improving the quality of life.
Keywords: symptom clusters, end-stage renal disease, hemodialysis
Introduction
ESRD is a non-communication disease which is a worldwide health problem. The disease cannot be cured and need hemodialysis (HD), peritoneal dialysis (PD), or kidney transplant (KT) to maintain the patient’s life.1 HD is one of the most effective and popular treatments. In Thailand, data in the year 2015 found that 54,104 of 85, 848 cases of ESRD patients treated with this HD modality.2 HD can prolong lives, but patients may suffer from physical and psychological symptoms caused by disease progression or treatment.3,4
ESRD patients undergoing hemodialysis have to face many symptoms such as tired/lack of energy/fatigue and discomfort from itching/dry skin or thirsty/dry mouth,5–9 sleep disorders,5,10 pain and anxiety.7–11 These symptoms affected the patient’s life and have led to a decreasing quality of life.3,12 It has been found that these symptoms may affect the death rate in ESRD patients who are receiving dialysis.13 Many patients experience multiple concurrent symptoms or symptom clusters, which may have a more significant effect than isolated symptoms. Symptom clusters are defined as two or more concurrent symptoms that are related to one another and may share a common aetiology.14,15
Current studies have shown that the symptoms tend to occur in a cluster when one of the symptoms occurs, it will also change other symptoms within the group.15,16 There is a limited study of symptom cluster in ESRD patients undergoing hemodialysis, although this group of patients must be faced with many symptoms along the illness trajectory and course of treatment. In Taiwan, a study of 117 hemodialysis patients using the Somatic Symptoms Disturbance Index reported the symptoms in 4 clusters including energy and sensory discomfort (tiredness, dry mouth, muscle weakness, and lack of vitality), GI and cardiac – pulmonary (chest tightness, chest pain, nausea, and vomiting), general symptoms of the uremic syndrome (headache, vertigo, dyspnea, and shortness of breath), and the electrolyte imbalance (numbness, joint-muscle pain, and arrhythmia).9 Another study by Amro, Waldum, Dammen, Miaskowski, and Os12 analyzed the symptoms of 301 patients receiving HD or PD in Norway using the Kidney Disease and Quality-of-Life-Short Form version 1.3 (KDQOL-SF36). Base on the Exploratory factor analysis, three factors were extract included uremic (nausea, lack of appetite, dizziness/faintness, feeling squeezed out, shortness of breath, chest pain), neuromuscular (numbness in extremities, sore muscles, cramps) and skin (itching, dry skin) clusters. The latest study was found in Uruguay, using the KDQOL-SF 36 assessing symptoms in 493 samples. The hierarchical cluster analyses revealed five groups of symptoms include Cutaneous, Cardiac, Digestive, Sensory-Motor and Energy.17 The symptoms from the three studies are similar, but they are different when grouped into clusters. It might result from the different contexts and cultures in each study site, including the use of different assessment tools.
In Thailand, there have not been any studies on the symptom clusters of ESRD patients undergoing hemodialysis. It is expected that the understanding of symptom clusters in patients undergoing HD in Thailand could help the health-care provider develop a comprehensive and effective intervention to relieve suffering and increase QOL. The purpose of this study was to explore the symptom clusters in ESRD patients undergoing hemodialysis.
Materials and Methods
Study Design and Sample
The data of this descriptive research were collected at the dialysis unit of the university hospital and specialized nephrology hospital in Bangkok. The population of this study were ESRD patient undergoing hemodialysis at two hospitals mention above. The sample size calculation base on the exploratory factor analysis, which is recommended to use the rule of five. The Dialysis Symptom Index-THAI has a total of 30 symptoms, so the number of samples is 150 samples.18 The purposive sampling was employed to ESRD patients undergoing HD who were: age of 18 years or more, for those over 60 years old, must pass the set test,19 regularly hemodialysis at least 3 months, able to communicate the Thai language, and willing to participate. The exclusion criteria were diagnosed with communicable disease or cancer in the advanced stage and admitted from hemodialysis complications.
Instruments
- The Set Test was used to screening the cognitive status of patients’ age ≥ 60 years.19 By asking the patients to naming of colours, animals, fruits, and the province with the maximum of 10 items in each set. The correct answer is awarded 1 point while the wrong answer is 0 points, a total score of 40 points. Patients with a score of ≥ 25 points refer to normal cognitive status.
- Personal Information Questionnaire (PIQ) was developed by the researcher to record the data including age, gender, weight, height, religion, education level, marital status, work history, smoking history, alcohol drinking history, duration of receiving hemodialysis, frequency of hemodialysis, co-morbidity, a dose of EPO drug, type of vascular access, and the current results of laboratory blood tests include Electrolyte, BUN, Ca, Cr, PO4, Hb, Hct, Kt/V, Albumin and nPCR.
- Dialysis Symptom Index—THAI (DSI-THAI): The DSI was developed by Weisbord et al20 and translated for this study under permission. The DSI-THAI contains 30 symptoms associated with the patients receiving hemodialysis. The symptoms experienced in the past month were answered as yes-no; if the answer was yes, the amount of the troublesome of this symptom was evaluated as “0 = the symptom had not been troublesome” to “4 = the symptom had been very troublesome” in 5-point Likert scale. The content validity of the DSI-THAI was confirmed by three experts, the CVI was 0.97. The Test-Retest reliability method was employed to try out the instrument in 10 samples who meet the inclusion criteria, and the result was 0.99.
Statistical Analysis
Descriptive statistics were used to analyze the demographic data in the PIQ. Symptoms were clustered by Exploratory Factor Analysis (EFA) via Principle Component Analysis (PCA) and simplified by varimax rotation. The eigenvalue was set at 1.0 and expressed only factor loadings greater than 0.4. Kaiser-Meyer-Olkin values (0.5) and Bartlett’s test of sphericity were evaluated to ensure sufficient unique variance among variables for factoring. The scree plots and their clinical relevance determined the number of factors. Pearson’s correlation coefficient was used to examine the associations between symptom clusters and clinical characteristics. All survey data were managed and analyzed with SPSS (Statistical Package for the Social Science for Windows).
Results
The sample consisted of 150 ESRD patients undergoing hemodialysis with the age of 65.53 ±15.09. The majority were female (52.7%), Buddhists (96.0%), and marriage (70.9%). Most of them had an income of around 1,001–5,000 baht per month, and had health-care costs covered by government welfare (59.6%). Almost half of them undergoing hemodialysis 2 times/week (54.4%) more than 2 years (44.9%) via AVF (46%). The mean time in treatment was 44.9 months (mode 24). Most of them using erythropoietin 4,000–8,000 unit/week (68.4%). The comorbidity mostly found were hypertension (HT) 87.3% and diabetes mellitus (DM) 56.7%. (Table 1). The laboratory data as shown in Table 2.
 |
Table 1 Demographic Characteristics and Clinical Information |
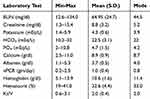 |
Table 2 Laboratory Test |
The symptoms were reported in 148 patients (98.7%), with a total of 30 symptoms. The average number of symptoms was 7.22 ± 6.92. The top five frequent symptoms were itching (71.11%), dry skin (67.82%), muscle soreness (57.23%), dry mouth (55.24%), muscle cramps (52.75%) and trouble staying asleep (52.75%). The most severe symptom was itching followed by dry skin, muscle soreness, dry mouth, trouble staying asleep, and trouble falling asleep, respectively (Table 3).
 |
Table 3 Prevalence and Severity of Symptom |
The symptoms were extracted into 8 factors, with 69.53% of the variance explained. Factor 1 consisted of 5 symptoms, with a factor loading of 0.369–0.839, eigenvalue of 10.65, and explained 11.62% of the factor’s variance. Factor 1 was labelled “gastrointestinal”. Factor 2 consisted of 8 symptoms, with a factor loading of 0.406–0.780, eigenvalue of 2.00, and explained 10.57% of the factor’s variance. Factor 2 was labelled “musculoskeletal and fluid volume”. Factor 3 consisted of 4 symptoms, with a factor loading of 0.563 −0.743, the eigenvalue of 1.81, and explained 10.56% of the factor’s variance. Factor 3 was labelled “Neurological”. Factor 4 consisted of 4 symptoms, with a factor loading of 0.541 −0.723, the eigenvalue of 1.57, and explained 9.91% of the factor’s variance. Factor 4 was labelled “Irritation of the mucous membranes and skin”. Factor 5 consisted of 2 symptoms, with a factor loading of 0.722 −0.773, the eigenvalue of 1.49, and explained 7.68% of the factor’s variance. Factor 5 was labelled “Depression”. Factor 6 consisted of 2 symptoms, with a factor loading of 0.856 −0.896, the eigenvalue of 1.18, and explained 7.50% of the factor’s variance. Factor 6 was labelled “Sleep disturbance”. Factor 7 consisted of 2 symptoms, with a factor loading of 0.975 −0.979, the eigenvalue of 1.13, and explained 6.54% of the factor’s variance. Factor 7 was labelled “Sexual”. Factor 8 consisted of 2 symptoms, with a factor loading of 0.609 −0.739, the eigenvalue of 1.03, and explained 5.16% of the factor’s variance. Factor 8 was labelled “Anemic” (Table 4).
 |
Table 4 Symptom Clusters in ESRD Patients Undergoing Hemodialysis |
Correlation analyses revealed significant correlations between symptom clusters and clinical characteristics including serum BUN with Neurological cluster (r = 0.21, p < 0.01) and BMI with Gastrointestinal cluster, Musculoskeletal and fluid volume cluster, Neurological cluster, Irritation of the mucous membranes and skin cluster, and Anemic cluster (r = 0.17, p < 0.05; r = 0.20, p < 0.05; r = 0.27, p < 0.001; r = 0.28, p < 0.001; r = 0.20, p < 0.05, respectively). Other laboratories were not associated with symptom clusters (Table 5).
 |
Table 5 Association Between Symptom Clusters and Clinical Characteristics |
Discussion
The subjects in this study had reported 1–28 symptoms in each person (Mean = 7.22, SD = 6.92). The top five symptom prevalences are itching, dry skin, muscle soreness, dry mouth, muscle cramps and trouble staying asleep. For the severity, the top five severely symptoms are itching, dry skin, muscle soreness, dry mouth, muscle cramps and trouble falling asleep. The result was consistent with the previous study that reported the most prevalence and severe symptom in dialysis patients in Australia,3 Norway,12 and Uruguay.17 The symptom that most prevalence and severe in this study are itching and dry skin. These symptoms were consistent with the laboratory results which found that the sample had a high phosphate. The accumulation of phosphate under the skin causing the skin dry and itchy.
Eight clusters were identified by using PCA with varimax rotation included: “Gastrointestinal” “Musculoskeletal and fluid volume” “Neurological” “Irritation of the mucous membranes and skin” “Depression” “Sleep disturbance” “Sexual” and “Anemic”
The gastrointestinal cluster consists of five symptoms which are constipation, nausea, vomiting, diarrhoea, and decreased appetite. This cluster was reported in a prior study in Spain4 and Taiwan.9 The vomiting and nausea symptom might be caused by various influences such as insufficient dialysis, drug side effect, and abnormal BUN level. This study reported the average BUN was 64.5 mg/dl which quite high and might induce unpleasant symptom of the GI tract.
The musculoskeletal and fluid volume cluster includes 8 symptoms including muscle cramps, swelling in legs, shortness of breath, restless legs or difficulty keeping legs still, numbness or tingling in feet, bone or joint pain, chest pain and muscle soreness. This cluster was found in the previous study in different symptoms and terms.3,11,12 The symptoms of bone or joint pain and numbness were related to disturbance of the potassium ion. The average potassium in this study was 4.5 mEq/L. The cause of restless legs was unknown, but common in patients with uremia and iron deficiency anemia. The shortness of breath, chest pain, and swelling in legs were defined as fluid volume symptoms in the previous study. These symptoms might occur from the excessive volume in the patients.3
The neurological cluster consists of 4 symptoms including difficulty concentrating, worrying, feeling nervous, and feeling irritable. This cluster has been reported in different terms such as emotional instability21 and psychological symptoms.3
The irritation of the mucous membranes and skin cluster consists of 4 symptoms including cough, dry mouth, dry skin, and itching. The cluster also reported in terms of skin problem.12,13,21 As mentioned earlier that the accumulation of phosphate under the skin resulting in dry skin, and itching. Even though the average phosphate in this study was 4.7 mEq/L but the result shows the wide range at 2–10.8 mEq/L.
The depression cluster consists of 2 symptoms which are feeling sad and feeling anxious. The result was quite differenced from the prior study. Lee and Jeon21 reported nausea, feeling anxious, vomiting, feeling depressed, and poor appetite in the emotional instability and uremia cluster. While Almutary, Douglas, and Bonner3 reported feeling anxious, worrying, feeling sad, depression, and feeling nervous in the psychological symptoms. Those two studies reported a variety of symptoms while the factor loading score of this study strongly supports the distinctiveness of this cluster. Hemodialysis has affected physical and psychosocial well-being because it changes the patient’s lifestyle. As shown in the previous study that depression was found frequently in the dialysis group.4
The sleep disturbance cluster consists of 2 symptoms which are trouble falling asleep and trouble staying asleep. The previous study reported sleep disturbance as a higher symptom burden22 and mix with lack of energy, feeling tired, trouble staying awake, trouble falling asleep, waking in the night, and not getting enough sleep in the fatigue/sleep cluster.23
The sexual cluster consists of 2 symptoms, which include decreased interest in sex and difficulty becoming sexually aroused. The sexual cluster was found in only one study.3 It might from the variation of the instruments that include these items.
The anemic cluster consists of 2 symptoms, which include lightheadedness or dizziness and headache. The prior study put dizziness and headache into the uremic cluster.12,13 For this study, we could explain in terms of the hemodialysis patients mostly had insufficient erythropoietin hormone leading to inhibition of erythropoiesis, decreasing erythrocyte lifespan, or blood loss during HD. When anemia occurs, the reduced oxygen supply might affect the patients feeling dizziness and headache.
As shown in this study and the previous study that the clusters of symptoms have some differences in each study. This variation may be caused by the difference in the instrument used to measure the symptoms and the method of data analysis. The KDQOL-SF was found the most frequently used but it has some limitations. It has a limited number of symptoms and absence of common symptoms which are presented in CKD including fatigue, pain, constipation, sleep disturbance, sexual dysfunction, anorexia, and psychological dysfunction. In this study, we used the Dialysis Symptom Index—THAI (DSI-THAI) which was developed by Weisbord et al (2004) and translated into Thai under permission. This instrument contains 30 comprehensive symptoms related to the patients receiving hemodialysis.
This study revealed the significant correlations between symptom clusters and some clinical characteristics. The serum BUN has a positive relationship with a Neurological cluster in this study. This finding is in accordance with other studies that reported in terms of uremic symptoms in patients with worse kidney function. The studies reported kidney unable to filtering metabolic waste which is clinically represented by lower GFR or higher BUN and serum creatinine levels.11,12,21 The uremic encephalopathy in patient with ESRD may have unclear onset and early manifestation can be non-specific such as fatigue, apathy, irritability and impaired concentration which difficult to early detection.24
BMI has a positive relationship with Gastrointestinal cluster, Musculoskeletal and fluid volume cluster, Neurological cluster, Irritation of the mucous membranes and skin cluster and Anemic cluster. There are two studies11,12 that reported the positive correlation of BMI and Musculoskeletal and fluid volume cluster which consistent with this study. The higher BMI was found to be associated with increased neuromuscular symptoms.12 According to this study reported the actual BMI on dialysis day, this might associate with the interdialytic weight gain (IDWG) particularly in the Musculoskeletal and fluid volume cluster and Anemic cluster. The recent study reported that patients with lower hemoglobin concentrations were older and IDWG ≥6%.25 Hemoglobin concentration varies dynamically depending on body fluid volume changes, these might lead to the presence of anemic symptoms. The remaining relationship between BMI and other symptom clusters still unclear and had no prior evidence. These issues need further investigation.
According to the symptom clusters, which affected the quality of life of patients both physical and psychological dimensions,3,4,12,21–23 the knowledge regarding symptom clusters could provide healthcare providers understanding the patients’ co-occurrence symptom experiences. This led to successfully develop symptom management strategies to relieving symptoms in the cluster, reducing medication use and enhancing the quality of life.
Our study has some limitations. The cross-sectional design limited the data gathering to only one data point, but the symptoms can change over time. The longitudinal studies are needed to explore the symptoms as the disease progresses and its treatment. The results may not be generalizable because this study was conducted in the two dialysis centers in Bangkok. The multicenter study will capture the overall symptom clusters in the Thai population.
Conclusions
The finding indicated eight symptom clusters in patients with End-Stage Renal Disease undergoing hemodialysis. For implication and recommendation, patients undergoing hemodialysis should be routinely assessed symptoms which lead to the proper management resulting in enhancing their quality of life. Further research should be studied on factors related to the symptoms and symptom clusters which leads to the data to develop the comprehensive management for the patients undergoing hemodialysis.
Ethical Consideration
This study complied with the Declaration of Helsinki and approved by the Research Ethics Committees of the Faculty of Medicine Ramathibodi Hospital: reference MURA 2015/283. All participants gave written informed consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research project is funded by the Ramathibodi School of Nursing, Faculty of Medicine Ramathibodi Hospital, Mahidol University.
Disclosure
The authors declare no conflicts of interest regarding this work.
References
1. KDOQI. NKF. KDOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. 2012; Available from: http://www.kidney.org/professionals/kdoqi/guidelines_ckd/toc.htm.
2. Chuasuwan A, Praditpornsilpa P. The Thai renal replacement therapy (TRT). 2015; Available from: ฉบบแกไข.pdf http://www.nephrothai.org/images/Final_TRT_report_2015_ฉบบแกไข.pdf.
3. Almutary H, Bonner A, Douglas C. Which patients with chronic kidney disease have the greatest symptom burden? A comparative study of advanced CKD stage and dialysis modality. J Ren Care. 2016;42(2):73–82. doi:10.1111/jorc.12152
4. Gutiérrez Sánchez D, Leiva-Santos JP, Cuesta-Vargas AI. Symptom burden clustering in chronic kidney disease stage 5. Clin Nurs Res. 2019;28(5):583–601. doi:10.1177/1054773817740671
5. Abdel-Kader K, Unruh ML, Weisbord SD. Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin J Am Soc Nephrol. 2009;4(6):1057–1064. doi:10.2215/CJN.00430109
6. Davison SN, Jhangri GS. Impact of pain and symptom burden on the health-related quality of life of hemodialysis patients. J Pain Symptom Manage. 2010;39(3):477–485. doi:10.1016/j.jpainsymman.2009.08.008
7. Davison SN, Jhangri GS, Johnson JA. Cross-sectional validity of a modified Edmonton symptom assessment system in dialysis patients: a simple assessment of symptom burden. Kidney Int. 2006;69(9):1621–1625. doi:10.1038/sj.ki.5000184
8. Weisbord SD, Fried LF, Arnold RM, et al. Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. J Am Soc Nephrol. 2005;16(8):2487–2494. doi:10.1681/ASN.2005020157
9. Yu IC, Huang J-Y, Tsai Y-F. Symptom cluster among hemodialysis patients in Taiwan. Appl Nurs Res. 2012;25(3):190–196. doi:10.1016/j.apnr.2010.11.002
10. Claxton RN, Blackhall L, Weisbord SD, Holley JL. Undertreatment of symptoms in patients on maintenance hemodialysis. J Pain Symptom Manage. 2010;39(2):211–218. doi:10.1016/j.jpainsymman.2009.07.003
11. Thong MS, van Dijk S, Noordzij M, et al. Symptom clusters in incident dialysis patients: associations with clinical variables and quality of life. Nephrol Dial Transplant. 2009;24(1):225–230. doi:10.1093/ndt/gfn449
12. Amro A, Waldum B, Dammen T, Miaskowski C, Os I. Symptom clusters in patients on dialysis and their association with quality-of-life outcomes. J Ren Care. 2014;40(1):23–33. doi:10.1111/jorc.12051
13. Amro A, Waldum B, von der Lippe N, et al. Symptom clusters predict mortality among dialysis patients in Norway: a prospective observational cohort study. J Pain Symptom Manage. 2015;49(1):27–35. doi:10.1016/j.jpainsymman.2014.04.005
14. Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. J Adv Nurs. 2001;33(5):668–676. doi:10.1046/j.1365-2648.2001.01697.x
15. Kim H-J, McGuire DB, Tulman L, Barsevick AM. Symptom clusters. Cancer Nurs. 2005;28(4):270–282. doi:10.1097/00002820-200507000-00005
16. Dodd MJ, Miaskowski C, Paul SM. Symptom clusters and their effect on the functional status of patients with cancer. Oncol Nurs Forum. 2001;28(3):465–470.
17. Galain AI, Dapueto JJ, Alvarez R, Gadola L. Prevalence of symptoms and symptom clusters of patients on dialysis in Uruguay. Value Health Reg Issues. 2019;20:28–35. doi:10.1016/j.vhri.2018.10.003
18. Aktas A, Walsh D, Rybicki L. Review: symptom clusters: myth or reality? Palliat Med. 2010;24(4):373–385. doi:10.1177/0269216310367842
19. Isaacs B, Akhtar AJ. The set test: a rapid test of mental function in old people. Age Ageing. 1972;1(4):222–226.
20. Weisbord SD, Fried LF, Arnold RM, et al. Development of a symptom assessment instrument for chronic hemodialysis patients: the dialysis symptom index. J Pain Symptom Manage. 2004;27(3):226–240. doi:10.1016/j.jpainsymman.2003.07.004
21. Lee SJ, Jeon J. Relationship between symptom clusters and quality of life in patients at stages 2 to 4 chronic kidney disease in Korea. Appl Nurs Res. 2015;28(4):e13–e9. doi:10.1016/j.apnr.2015.03.004
22. Shim HY, Cho M-K. Factors influencing the quality of life of haemodialysis patients according to symptom cluster. J Clin Nurs. 2018;27(9–10):2132–2141. doi:10.1111/jocn.13904
23. Curtin RB, Bultman DC, Thomas- Hawkins C, Walters BA, Schatell D. Hemodialysis patients’ symptom experiences: effects on physical and mental functioning. Nephrol Nurs J. 2002;29(6):562–598.
24. Brouns R, De Deyn PP. Neurological complications in renal failure: a review. Clin Neurol Neurosurg. 2004;107:1–16. doi:10.1016/j.clineuro.2004.07.012
25. Hara T, Kimachi M, Akizawa T, Fukuhara S, Yamamoto Y. Interdialytic weight gain effects on haemoglobin concentration and cardiovascular events. Kidney Int Rep. 2020. doi:10.1016/j.ekir.2020.07.027
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
