Back to Journals » Clinical Ophthalmology » Volume 15
Sutureless Scleral Fixated IOL: The “Catcher Pole” Technique
Authors Tamburrelli C , Tamburrelli AC
Received 1 November 2020
Accepted for publication 26 November 2020
Published 12 January 2021 Volume 2021:15 Pages 121—128
DOI https://doi.org/10.2147/OPTH.S288769
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Video abstract of "Sutureless scleral fixated IOL: The “Catcher Pole” technique" [ID 288769].
Views: 6751
Ciro Tamburrelli,1 Anna Clara Tamburrelli2
1Oftalmico Hospital of Rome, Rome, Italy; 2La Sapienza University of Rome, Clinica Oculistica Ospedale Umberto I, Rome, Italy
Correspondence: Ciro Tamburrelli
Oftalmico Hospital of Rome, Via Filippo Nicolai 91, Rome 00136, Italy
Email [email protected]
Purpose: To describe a new surgical technique for sutureless intrascleral intraocular lens (IOL) fixation with an adapted retinal scraper used as an instrument “the Catcher Pole” to retrieve the IOL haptic through a scleral tunnel.
Setting: Public Eye Hospital, Roma, Italy.
Design: Retrospective case series.
Methods: Twenty-one eyes from 19 patients who underwent sutureless intrascleral IOL fixation were studied. A standard three-piece posterior chamber IOL (PCIOL) was implanted in aphakia or rescued and fixated in cases of dislocated PCIOL. A 23 to 25 G retinal loop scraper (the “Catcher Pole“) was inserted through a 1.5 mm long tunneled sclerotomy performed on the horizontal meridian, to capture, hold and externalize the tip of the haptic of the IOL. A flange created with an handheld cautery on the externalized haptic tip prevents IOL slippage. The best-corrected visual acuity (BCVA), central corneal pachymetry (CCP), IOL tilt and complications were assessed.
Results: In twenty-one eyes of 19 patients, the mean preoperative BCVA was 0.61 logMAR units ± 0.05 SD, and the mean postoperative BCVA improved significantly to 0.18 logMAR units at three months ± 0.05 SD (P=0.002). The mean preoperative CCP was 610 μ ± 17 SD and the mean postoperative CCP 623 μ ± 16 SD, (P=0.73). In the subgroup that underwent IOL tilt evaluation, mean IOL tilt was 3.19± 2.01. The postoperative complications included iris capture of the IOL in one eye (4,7%) and transient ocular hypertension in two eyes (9,4%).
Conclusions: The “Catcher Pole” sutureless intrascleral IOL fixation technique is easy to perform with reduced anterior chamber manipulations and achieves both anatomical and optical stability.
Keywords: intrascleral intraocular lens fixation, Catcher Pole technique, capsular loss
Purpose
Insertion of intraocular lens (IOL) in the capsular bag at the end of cataract surgery is considered the gold standard because the artificial lens is inserted in the physiological position of the natural lens and maintain a safe distance from ciliary body, iris and corneal endothelium. Sometimes damage to the capsular bag or zonular loss occur during surgery or may be found naturally before surgery, in such cases the IOL cannot be placed in the capsular bag and different surgeries are required to securely implant and fix the IOL. Three types of surgical options are available: anterior chamber IOL (ACIOL), iris-fixed IOL, or intrascleral-fixated IOL. Intrascleral-fixated IOL implantation is gaining interest among anterior and posterior segment surgeons because of its location in the posterior chamber similar to the in the bag implantation.9 The intrascleral IOL fixation techniques are classified as sutured or sutureless. The latter is preferred for the absence of suture-related complications, ie suture degradation and late IOL dislocation and also for the faster surgical time and easier surgical maneuvers.1 However all the sutureless intrascleral IOL techniques share specific complications: IOL haptic damage or dislocation from the intrascleral tunnel.11,13 We performed the intrascleral sutureless IOL implantation with a simplified technique addressing the problem of the haptic extrusion from the posterior chamber. An adapted surgical instrument, specifically designed for vitreo-retinal surgery eases the capture of the prolene tip and its extrusion through a simplified tunneled sclerotomy. The purpose of this paper is to introduce surgical modifications in the intrascleral sutureless IOL fixation techniques and report safety and efficacy in a series of 21 eyes with preexisting partial or total zonular loss or without any posterior and/or anterior capsular support consecutive to ocular trauma, surgery, and congenital or acquired zonular defect.
Methods
Twenty-one eyes of 19 patients who underwent “Catcher Pole” intrascleral IOL fixation between January 2019 and January 2020 were retrospectively evaluated. The inclusion criteria were: secondary implantation of intrascleral-fixated IOL for aphakia, subluxated or dislocated crystalline lens without sufficient capsular support and dislocated IOL. In three eyes a dislocated standard three-piece posterior chamber IOL (PCIOL) was rescued and intrascleral fixated; patients with previous additional surgical procedures were also included, such as primary pars plana vitrectomy (PPV), retinal detachment (RD), or proliferative diabetic retinopathy (PDR). The exclusion criteria were dense corneal leukoma or decompensated preoperative IOP above 26 mmHg, sclerokeratitis, and a postoperative follow-up duration of less than three months. All surgeries were performed by the same experienced surgeon (CT) at Oftalmico Hospital, ASL Roma 1, Rome Italy. This study adhered to the tenets of the Declaration of Helsinki. Ethics Committee approval was obtained from ASL Roma 1 Hospital review board. Informed consent was obtained from all patients or their parents, and the possible complications of the procedure were explained.
Standard ophthalmologic examination records, such as the initial best-corrected visual acuity(BCVA), slit-lamp evaluation (SL-D7, CSO Firenze, Italy), IOP, pre and postoperative central corneal pachymetry (CCP) (Canon TX-20P), follow-up duration, final visual acuity, postoperative IOL position with anterior segment OCT Casia 3 (SS-1000 CASIA; Tomey Corporation, Nagoya, Japan) and, in a smaller subgroup of patients ultrasound biomicroscopy (UBM) (Quantel Medical, Clermont-Ferrand, France) were also obtained.
Casia 3 was used to evaluate accurate positioning of the IOL in a subgroup of nine patients by IOL tilt and decentration. A straight line between the iris and corneal angles was marked as the reference line. IOL tilt was defined as the angle between the reference line and the horizontal axis of the IOL. IOL decentration was defined as the horizontal distance between the midpoint of the reference line and IOL horizontal axis.12,14 UBM images were used in a small subgroup of five patients mostly to analyze proper intrascleral position of the IOL.
The Wilcoxon signed-rank test was used to determine the significance of any association between preoperative and postoperative BCVA or CCP. A P-value less than 0.05 was considered significant. Statistical analyses were performed using SPSS for Mac software (version 25.0, IBM Corporation, Armonk, NY, USA).
Surgical Technique
The present technique is an evolution and simplification of the original technique described by Gabor and Pavlidis.16 Under preoperative preparation and peribulbar anesthesia, two minimal conjunctival peritomy were created at the three o’clock and nine o’clock positions. A superior 3.0 mm corneal incision was created. An inferotemporal valved 23G trocar was placed inferotemporally as a cautionary measure in case PPV becomes necessary, while regular three-port trocars were inserted in cases with planned PPV. In three cases the previously implanted and dislocated PCIOL was rescued and implanted with no need to replace it with another one.
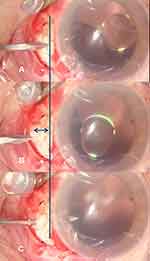
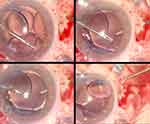
Two sclerotomy were performed on the three o’clock and nine o’clock meridian with an angulated 21 G stiletto knife, starting 1.5 mm posterior to the point corresponding to the iris root on the sclera. The blade was advanced toward the limbus, creating a tunneled sclerotomy approximately 1.5 mm long. Care was taken to create a radial tunnel tangent to the scleral surface from the entrance up to the projection of iris root on the sclera. At this level, the stiletto knife was directed posteriorly entering behind the iris root, in the ciliary sulcus of the posterior chamber with the tip of the blade visible in the pupillary aperture (Figure 1). A three-piece IOL was then inserted into the anterior chamber by the injector, and both haptics were placed over the iris plane to prevent the IOL from falling into the vitreous cavity, a second option was also the placement of a loop over the iris plane and the second loop kept outside of the anterior chamber. A disposable 23 G toothed forceps was used through corneal paracentesis to grasp the distal haptic 2 mm from the tip, while a manually angulated loop retinal scraper (finesse Flex Loop DSP Alcon Grieshaber AG) (Figure 2) was inserted through the nasal or temporal sclerotomy. The adapted loop retinal scraper was used as a catcher pole, brought with the loop open around the prolene tip, retracted and locked to capture the extremity, as close as possible to the terminal end. If care was taken to catch only the tip of the prolene loop, extraction and externalization of the haptic through the sclerotomy occurred with no effort and without any damage to the haptic (Figure 3). Before extraction, the surgeon releases the strength around the captured haptic that opens slightly the wire loop to allow a fine sliding toward the very end of the haptic ensuring with this maneuver no or minimal protrusion of the haptic tip on one side of the wire loop. Cauterization of the externalized tip created a slight enlargement to prevent any retro-displacement or dislocation of the IOL. At the end of surgery the conjunctiva was closed over the externalized prolene tip. According to our experience, satisfactory IOL fixation is obtained mainly by the tight tunnel created with sclerotomy which bends both haptics posteriorly. Topical steroids were used in all patients postoperatively. The duration of surgery was recorded by video.
 |
Figure 2 The “Catcher Pole”, a disposable loop retinal scraper (finesse Flex Loop DSP Alcon Grieshaber AG) with a retractable wired loop used to catch, hold and externalize the tip of the IOL haptic. |
Results
Baseline and postoperative characteristics are shown in Table 1. The haptics were well fixed and the IOL was centrally positioned in all 21 eyes of 19 patients (nine males, 10 females; mean age, 53.6 ±19.14 years old; range: 41–86 years). The mean follow-up period was 10.32±2.67 months (range: 6–14 months). There were four aphakia, 10 dislocated PC IOLs, and seven subluxated crystalline lenses.
 |
Table 1 Baseline Characteristics and Postoperative Data |
All patients had associated ocular conditions, seven patients complicated ocular trauma (eight eyes), primary RD (two eyes) IOL dislocation (11 eyes). Some patients had complications before surgery (eg, iridodialysis, traumatic glaucoma). The decimal BCVA was measured and converted to logarithm of the minimum angle of resolution (logMAR) units for statistical analyses. The Wilcoxon signed-rank test was used to determine the significance of any association between the preoperative and postoperative BCVA and CCP P<0.05 was considered significant. The mean preoperative BCVA was 0.61 logMAR units ±0.05 SD, and the mean postoperative BCVA improved significantly to 0.18 logMAR units at three months ±0.05 SD (P=0.002). The mean preoperative CCP was 610 µ ±17 SD and the mean postoperative CCP increased slightly 623 µ ±16 SD which was not significant (P=0.73). In the subgroup that underwent IOL tilt evaluation mean IOL tilt was 3.19±2.01. The postoperative complications included iris capture of the IOL in one eye (4.7%), transient ocular hypertension in two eyes (9.4%). No other complications, namely cystoid macular edema, retinal detachment, endophthalmitis, IOL dislocation, or vitreous hemorrhage, were detected during the follow-up period.
Discussion
In the group of sutureless intrascleral IOL techniques, handling of the haptics represent a major problem due to the structural properties of the haptic material, prolene or polymethylmethacrylate (PMMA) that can easily be broken with the forceps or markedly damaged when extracted from the posterior chamber through the sclera, in particular for PMMA. Therefore, improvement in all the proposed surgical procedures mainly address the issue of haptic externalization and scleral fixation. Intrascleral IOL fixation techniques could also be classified into those with and without a scleral flap. Agarwal et al and Gabor et al achieved sutureless scleral IOL fixation using fibrin glue to close the scleral flaps.2,15,16 Techniques without a scleral flap are simpler and do not require sutures or fibrin glue. However, there is a potential risk of haptic extrusion. Unstable intrascleral fixation may cause IOL decentration or dislocation, which may impact refraction and visual function.17,18 IOL haptic fixation is easily accomplished using techniques with a scleral flap, but the surgical procedure is relatively complex.12,19,20
Yamane et al developed a double-needle technique and flanged IOL fixation technique to provide firm haptic fixation without using suture or glue.12,21 We have performed sutureless scleral fixation IOL for the past four years, preferred over sutured techniques abandoned for the known set of complications and also because of more time-consuming surgical procedures with higher postoperative astigmatism.8–10
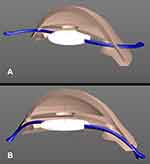
In the last year we have changed our sutureless technique eliminating from our procedure the scleral flap preparation that sometimes results in wound leakage and postoperative hypotony22 in favor of the tunneled radial sclerotomy. More recently, we introduced the “Catcher Pole” instrument to ease the extrusion of the second haptic. The 21 G tunneled radial sclerotomy, tangent to the scleral surface, is easily and rapidly performed and is completely self-sealing. The IOL haptics are pressed between the tight anterior and posterior tunnel walls and an excellent IOL blockage is achieved. The haptics are normally designed with the prolene loop on the same plane of the optic disc or even 10° angulated anteriorly, therefore the posterior angulation of the tunnel of the radial sclerotomy forces the haptics to bend posteriorly for the entire length of the tunnel. The scleral tunnel retains the haptic tendency to remain planar with optic disc or even more to move 10° anteriorly, such opposite forces contribute to fully stabilize the fixated IOL (Figure 4). UBM and anterior segment OCT demonstrated a securely fixated IOL and well-centered optic (Figures 5 and 6). Externalization of IOL haptics is one of the surgically challenging steps in intrascleral-fixated IOL procedures.23 We used this technique for three years before switching to the actual “Catcher Pole”, the intraocular forceps technique,16 although deformation and rupture of the IOL haptics with the forceps was not a rare occurrence during extrusion through the sclerotomy under the scleral flap. In the double-needle technique, reported by Yamane et al, it is also difficult to grasp the second haptic and insert it into a scleral tunnel after the first haptic is externalized.12,21 The most difficult step is threading the trailing haptic with the needle for fixation. If using an IOL with weak haptics, this step can result in haptic kink or breakage, which renders the haptics useless for this technique and necessitating explantation of the IOL. More recent techniques have been reported to overcome these difficulties.3–7,24,25 The major advantage of the “Catcher Pole” technique depends on the adaptation of a disposable 23 or 25 G cannula with a retractile wired loop normally used as retinal scraper, inserted into the temporal and nasal scleral tunnel to externalize the haptic tip with minimal or no damage. Due to the adaptation of an instrument designed for different purposes, the complete retraction of the loop and the metallic structure of the wire may damage the haptic and even cut it if excessive strength is applied on the push button in retraction. A completely redesigned instrument with a different wire material and predefined stop to prevent full retraction of the wire should become available. To avoid cutting or damage to the IOL haptics, the minimum wire loop diameter should equal the diameter of the haptics of the three-piece IOL, which usually is 0.14 to 0.17 mm. The BCVA in eyes with opacification of cataract or proliferated lens tissue in the center of the pupil improved after surgery by removal of the opacification, while the BCVA in eyes with aphakia and in eyes with subluxated lenses or IOLs did not change after secondary IOL surgery, however, the mean BCVA significantly improved after surgery at three months in our series (P=0.002). The mean IOL tilt of an IOL of a sutureless intrascleral fixation technique was 4.31±2.01° considered clinically not significant although higher than reported figures in similar techniques and larger compared with the IOL tilt after in the bag fixation. No postoperative corneal edema was detected and moderate increase in postoperative CCP, 610 µ ±17 SD vs 623 µ ±16 SD was not statistically significant. There are limitations to our study, including a small sample size, short follow-up period, and no control group. Although cases with only six months follow-up were included, the follow-up periods were >12 months in 15 cases. In these 15 cases, there were no cases of IOL decentration, severe complications, or significant changes of the BCVA during the longer follow-up period. Therefore, compared with other techniques, our approach seems to solve the problems in grasping and externalizing the haptic and simplify the scleral tunnel construction. The risk of multiple anterior segment manipulations, therefore, seems minimized. The “Catcher Pole” technique appears to be a simple and reliable surgical technique with a short learning curve, suitable for beginners and surgeons with limited experience.
Disclosure
The article has not been presented at any meeting. The authors did not receive any financial support from any public or private sources. The authors have no financial or proprietary interest in a product, method, or material described herein. The authors report no conflicts of interest in this work.
References
1. Can E. Flapless and sutureless intrascleral fixation of posterior chamber intraocular lens for correction of aphakia. J Cataract Refract Surg. 2018;44(8):929–931. doi:10.1016/j.jcrs.2018.03.037
2. Chantarasorn Y, Techalertsuwan S, Siripanthong P, et al. Reinforced scleral fixation of foldable intraocular lens by double sutures: comparison with intrascleral intraocular lens fixation. Jpn J Ophthalmol. 2018;62(3):365–372. doi:10.1007/s10384-018-0579-4
3. Hwang ES, Warren CC, Koenig SB. Flanged intrascleral intraocular lens fixation with a single needle. J Cataract Refract Surg. 2018;44(12):1526–1527. doi:10.1016/j.jcrs.2018.08.020
4. Maruko I, Koizumi H, Kogurekatakura A, et al. Extraocular technique of Intrascleral intraocular Lens fixation using a pair of the shaft-bended 27-gauge needles. Retina. 2016;37(1):191. doi:10.1097/IAE.0000000000001257
5. Morkin MI, Patterson M. Scleral-sutured intraocular lenses: single-surgeon technique for suture-preloaded intraocular lens insertion through a small-incision corneal wound. J Cataract Refract Surg. 2019;45(2):121–124. doi:10.1016/j.jcrs.2018.09.020
6. Ohta T, Toshida H, Murakami A. Simplified and safe method of sutureless intrascleral posterior chamber intraocular lens fixation: Y-fixation technique. J Cataract Refract Surg. 2014;40(1):2–7. doi:10.1016/j.jcrs.2013.11.003
7. Prenner JL, Feiner L, Wheatley HM, et al. A novel approach for posterior chamber intraocular lens placement or rescue via a sutureless scleral fixation technique. Retina. 2012;32(4):853–855. doi:10.1097/IAE.0b013e3182790ed3
8. Price MO, Price FW
9. Sindal MD, Nakhwa CP, Sengupta S. Comparison of sutured versus sutureless scleral-fixated intraocular lenses. J Cataract Refract Surg. 2016;42(1):27. doi:10.1016/j.jcrs.2015.09.019
10. Stem MS, Wa CA, Todorich B, et al. 27-gauge sutureless intrascleral fixation of intraocular lenses with haptic flanging: short-term clinical outcomes and a Disinsertion force study. Retina. 2018. doi:10.1097/IAE.0000000000002268
11. Takayama K, Akimoto M, Taguchi H, et al. Transconjunctival sutureless intrascleral intraocular lens fixation using intrascleral tunnels guided with catheter and 30-gauge needles. Br J Ophthalmol. 2015;99(11):1457–1459. doi:10.1136/bjophthalmol-2014-306579
12. Yamane S, Inoue M, Arakawa A, et al. Sutureless 27-gauge Needlee guided Intrascleral intraocular Lens implantation with lamellar scleral dissection. Ophthalmology. 2014;121(1):61–66. doi:10.1016/j.ophtha.2013.08.043
13. Zhang Y, He F, Jiang J, et al. Modified technique for intrascleral fixation of posterior chamber intraocular lens without scleral flaps. J Cataract Refract Surg. 2017;43(2):162–166. doi:10.1016/j.jcrs.2016.10.029
14. Zhao H, Wang W, Hu Z, et al. Long-term outcome of scleral-fixated intraocular lens implantation without conjunctival peritomies and sclerotomy in ocular trauma patients. BMC Ophthalmol. 2019;19(1):164. doi:10.1186/s12886-019-1172-4
15. Agarwal A, Kumar DA, Jacob S, et al. Fibrin glue–assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34(9):1433–1438. doi:10.1016/j.jcrs.2008.04.040
16. Gabor S, Pavlidis M. Sutureless intrascleral posterior chamber intraocular lens fixation. J Cataract Refract Surg. 2007;33(11):1851–1854. doi:10.1016/j.jcrs.2017.12.011
17. Chee SP, Chan NS. Suture snare technique for scleral fixation of intraocular lenses and capsular tension device. Br J Ophthalmol. 2018;102(10):1317–1319. doi:10.1136/bjophthalmol-2018-311868
18. Kumar DA, Agarwal A, Packiyalakshmi S, et al. Complications and visual outcomes after glued foldable intraocular lens implantation in eyes with inadequate capsules. J Cataract Refract Surg. 2013;39(8):1211–1218. doi:10.1016/j.jcrs.2013.03.004
19. Matsui Y, Matsubara H, Hanemoto T, et al. Exposure of haptic of posterior chamber intraocular lens after sutureless intrascleral fixation. BMC Ophthalmol. 2015;15(1):104. doi:10.1186/s12886-015-0102-3
20. Saleh M, Heitz A, Bourcier T, et al. Sutureless intrascleral intraocular lens implantation after ocular trauma. J Cataract Refract Surg. 2013;39(1):81–86. doi:10.1016/j.jcrs.2012.08.063
21. Yamane S, Sato S, Maruyama-Inoue M, et al. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136. doi:10.1016/j.ophtha.2017.03.036
22. Todorich B, Stem MS, Kooragayala K, et al. Structural analysis and comprehensive surgical outcomes of the sutureless intrascleral fixation of secondary intraocular lenses in human eyes. Retina. 2017:1. doi:10.1097/IAE.0000000000001941.
23. Yoshida N, Kojima T, Yokoyama S, et al. New surgical approach for intrascleral fixation using an intraocular lens with hook-shaped haptics. J Cataract Refract Surg. 2018;44(2):129–133. doi:10.1016/j.jcrs.2017.12.011
24. Dooho Brian K. MD Trailing-haptic-first modification of double-needle intrascleral haptic fixation technique. J Cataract Refract Surg. 2018;44:424–428Q.
25. Yang Y, Yao T, Zhou Y, Wang Y, Wang Z. A modified intrascleral intraocular lens fixation technique with fewer anterior segment manipulations: 27-gauge needle-guided procedure with built-in 8-0 absorbable sutures. BMC Ophthalmol. 2019;19(1):234. doi:10.1186/s12886-019-1239-2
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.