Back to Journals » Clinical Ophthalmology » Volume 14
Stereopsis After Unilateral Macular Hole Surgery with Internal Limiting Membrane Peeling
Authors Ohta K, Sato A, Senda N, Fukui E
Received 15 April 2020
Accepted for publication 26 May 2020
Published 26 June 2020 Volume 2020:14 Pages 1777—1783
DOI https://doi.org/10.2147/OPTH.S257462
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Kouichi Ohta, Atsuko Sato, Nami Senda, Emi Fukui
Department of Ophthalmology, Matsumoto Dental University, Nagano, Japan
Correspondence: Kouichi Ohta
Department of Ophthalmology, Matsumoto Dental University, 1780 Gobara, Hirooka, Shiojiri, Nagano 399-0781, Japan
Tel/ Fax +81-263-51-2210
Email [email protected]
Purpose: We have shown distinct morphological changes of the foveal retina such as horizontally asymmetrical retinal thicknesses and displacements of the fovea toward the optic disc after successful idiopathic macular hole (MH) closure by MH surgery with internal limiting membrane (ILM) peeling. The purpose of this study was to determine whether these morphological changes will alter the stereoacuity.
Setting: This was a non-randomized, retrospective study conducted on patients who underwent MH surgery at the Matsumoto Dental University Hospital, Nagano, Japan.
Methods: Forty patients (22 women, 18 men) who underwent MH surgery with ILM peeling for a unilateral MH were studied. At > 6 months after the PPV, the stereoacuity was measured with the Titmus stereotest (TST) and the TNO stereotest (TNO). The relationship between the stereoacuity and the age, MH size, best-corrected visual acuity (BCVA), foveal retinal thickness, and amount of nasal shift of the retina was determined.
Results: The mean postoperative BCVA was − 0.05 ± 0.11 logarithm of the minimum angle of resolution (logMAR) units. The percentage of cases with good stereoacuity of ≤ 100 sec of arc was 87.5% with the TST and ≤ 240” was 90% with the TNO test. A better stereoacuity was significantly correlated with a younger age (r = 0.36, P < 0.05; with TNO), smaller MH (r = 0.51, P < 0.001, with TST), better postoperative BCVA (r = 0.43 P < 0.01 with TST; r = 0.49, P < 0.01 with TNO), but not with the parafoveal retinal thickness or degree of nasal shift.
Conclusion: The postoperative stereopsis is relatively good in patients with better postoperative BCVA after MH surgery with ILM peeling, even though foveal morphological changes had occurred.
Keywords: idiopathic macular hole, internal limiting membrane, optical coherence tomography, stereopsis, vitrectomy
Introduction
Idiopathic macular hole (MH) can be closed by pars plana vitrectomy (PPV) with fluid-gas exchange.1 The success rate of closure is improved by combining the PPV with internal limiting membrane (ILM) peeling and gas/air tamponade.2–4 However, even after successful closure and an improvement of the best-corrected visual acuity (BCVA), the postoperative quality of vision, such as distortion, diplopia, and stereopsis may not always be satisfactory. Stereopsis is the ability to perceive the depth of objects in the visual field based on the disparity of the images formed on the two retinas. The binocular visual function after PPV for MH has been evaluated, and the stereopsis was reduced in eyes with a unilateral MH with some recovery observed after surgery.5 The eyes with better postoperative stereopsis were those with better pre-and postoperative BCVA.6
Recent spectral-domain optical coherence tomography (SD-OCT) studies clearly showed changes in the microstructure of the photoreceptors after PPV for MH. For example, a significant correlation was found between a shorter defect of the cone outer segment tips (COST) line (now called the interdigitation zone, IDZ) and a better BCVA.7 It has also been shown that there was a significant correlation between the increased parafoveal nasal retinal thickness and the decreased temporal retinal thickness postoperatively and the microstructural changes after ILM peeling.8–11 Relevant to this study, Kawano et al reported that the distance between the optic disc and the center of MH was significantly shorter after the successful closure of the MH.12 This displacement of the center of MH toward the optic disc has been reported by several groups including ours.13–15
The purpose of this study was to determine whether these morphological changes will alter the stereoacuity.
Methods
This was a non-randomized, retrospective study. The medical charts of 40 eyes of 40 Japanese patients with a unilateral, idiopathic, full-thickness MH (18 men, 22 women) who had been treated at the Matsumoto Dental University Hospital between September 2008 and October 2016 were reviewed. Only eyes successfully closed after the initial surgery were studied. In addition, patients with a BCVA ≥20/30 at 6 months after surgery were used to investigate the stereoacuity. The fellow eyes also had good BCVA of ≥20/20 without retinal diseases. Patients with secondary MH associated with rhegmatogenous retinal detachment, an epiretinal membrane (ERM), high pathological myopia, and diabetic retinopathy were excluded.16 Eyes with glaucoma and uveitis were also excluded. In this retrospective study, the patients with a BCVA < 20/30 were excluded because of these criteria and short follow-up periods.
The MH surgeries were performed after the patients received a detailed explanation of surgical procedures and examinations. The procedures used in this consecutive case series study were approved by the Institutional Review Board and Ethics Committee of Matsumoto Dental University. Approval was also obtained for the review of the data from medical charts of the patients with diseases. A written informed consent was obtained for the surgery and for the use of data for research studies.16 The procedures used conformed to the tenets of the Declaration of Helsinki.
Surgical Procedures
The MHs were at stage 2 in 11 eyes, stage 3 in 22 eyes, and stage 4 in 7 eyes by the Gass classification.17 The PPV was performed with standard 23-gauge (23G; n = 7), 25G (n = 28), or 27G (n = 5) instruments by a single surgeon (KO). Cataract surgery with intraocular lens implantation was also performed on 38 eyes. The other two eyes were pseudophakic. A posterior vitreous detachment was created in 33 eyes with stage 2 and 3 MHs by an intravitreal injection of triamcinolone acetonide (TA, Kenakolt-A; Bristol Pharmaceuticals KK, Tokyo, Japan; or MaQaid, Wakamoto Pharmaceuticals Co., Ltd, Tokyo, Japan) to make the hyaloid membrane more visible. The TA was re-injected to make the ILM more visible.15,16 When the ILM was still not clearly visible, approximately 0.5 mL of 0.25% indocyanine green (ICG; Ophthagreen®, Santen Pharmacy, Osaka, Japan) was injected in 5 eyes, or 0.025% Brilliant Blue G (Brilliant Peel®, Geuder, Heidelberg, Germany) was injected in 26 eyes.15,16 The ILM was peeled off over 2 to 4 disc areas. After fluid/air exchange, 20% sulfur hexafluoride (SF6) was injected for a gas tamponade. The patients were instructed to remain in a prone position for at least 7 days.15,16
Spectral-Domain Optical Coherence Tomography (SD-OCT)
The assessments of the morphology of the retina were performed more than 6 months after the PPV with an SD-OCT device (Spectralis HRA+OCT, Heidelberg Engineering, Heidelberg, Germany). The macular thickness was obtained from the volume scan mode of the OCT instrument as described in detail.8,11,15,16,18,19
The horizontal and vertical images centered on the fovea in the cross-hair mode (30°) were evaluated. The center point of the opened MH was determined manually in the enlarged images of the retina on a monitor screen. Next, the site of a small retinal vessel crossing the temporal-inferior margin of the optic disc was identified. Then, the distance from the selected site on the disc margin to the selected center of the opened or closed MH was manually measured and designated as the disc-to-fovea distance.15
Stereopsis Measurements
The stereoacuity was measured with the Titmus stereotest (TST) and the TNO stereotest (TNO) at the standard viewing distance of 40 cm with appropriate refractive corrections. Both tests were done at more than 6 months after the surgery with a mean of 46.4 ± 30.1 months. To ensure that the patients were not using monocular clues with the Titmus test, the responses were checked by inverting the stereo targets and asking the patient if the target appeared in front or behind the page.5 The relationships between the stereoacuity and the age, best-corrected visual acuity (BCVA), MH size, foveal retinal thickness, and nasal shift were analyzed.
Statistical Analyses
The results are expressed as the means ± standard deviations (SDs). The BCVA was measured with a Landolt C chart, and the decimal values were converted to logarithm of the minimal angle of resolution (logMAR) units.16,19 The significance of the differences in the pre- and postoperative BCVAs was determined by t tests. The results of TST and TNO are expressed as “seconds of arc”. Statistical analysis was done after converting the values to logarithmic units. The significance of the correlations between the stereoacuity and other parameters was determined by the Spearman rank correlation test. The significance of the relationships was also determined by linear regression analyses (Excel; Microsoft Corp, Redmond, WA). A difference was taken to be statistically significant when the P was <0.05.
Results
Best-Corrected Visual Acuity (BCVA) of All Eyes
The MH was closed in all eyes after the first surgery without complications. The mean age at surgery was 67.1 ± 6.3 (range, 54–82) years. The mean preoperative MH size was 372.3 ± 138.9 µm (range, 160 to 828 µm).
The postoperative BCVA was −0.05 ± 0.11 logMAR units which was significantly better than the preoperative BCVA of 0.45 ± 0.19 logMAR units (P <0.0001).
Binocular Function After Successfully Closed MH with Surgery
Postoperatively, 35 of the 40 patients (87.5%) had a stereoacuity at the normal level of 40–100 sec of arc as measured by the Titmus test. Moreover, 25 patients (62.5%) were at a better level of 40”-60”, and 16 (40.0%) were at the best level of 40” (Figure 1A). The mean stereoacuity by the Titmus test was 1.81± 0.24 log units (63.8 sec of arc).
The steroacuities measured by the TNO after surgery were similar. A normal stereoacuity of 60”-240” was observed in 36 of the 40 patients (90.0%; Figure 1B). Although a better stereoacuity, such as 60”-120”, was observed in 22 patients (55.0%), a stereoacuity of 30” or 15” was not. The mean stereoacuity by the TNO stereotests was 2.23 ± 0.34 log units (169.8 sec of arc).
Relationship Between Stereoacuity and Age, Macular Hole Size, and BCVA
The stereoacuity determined by the TNO but not the TST test was significantly correlated with the age at surgery (r = 0.359, P = 0.02; Figure 2A and B). The stereoacuity by TST was significantly correlated with the size of the MH (r = 0.51, P = 0.0008; Figure 3A), although that by TNO was not (Figure 3B). The postoperative BCVA was significantly correlated with stereoacuity by both the TST (r = 0.434, P = 0.005; Figure 4A) and TNO tests (r = 0.4986, P = 0.001; Figure 4B), although the preoperative BCVA was not (data not shown).
 |
Figure 2 Correlation between age and postoperative stereopsis. (A) Titmus stereoacuity and (B) TNO stereoacuity. |
 |
Figure 3 Correlation between size of macular hole (MH) and postoperative stereopsis. (A) Titmus stereoacuity and (B) TNO stereoacuity. |
 |
Figure 4 Correlation between postoperative best-corrected visual acuity and stereoacuity at more than 6 months after surgery. (A) Titmus stereoacuity and (B) TNO stereoacuity. |
Relationship Between Stereoacuity and Parafoveal Microstructural Changes
The mean central retinal thickness (CRT) after MH surgery was 302.0 ± 25.4 µm. The mean parafoveal retinal thickness was 361.3 ± 15.8 µm (nasal), 311.7 ± 17.1 µm (temporal), 338.6 ± 17.3 µm (superior), and 338.6 ± 15.9 µm (inferior). There was no significant correlation between the stereoacuity and CRT and the parafoveal retinal thicknesses (Table 1). Although the distance of the foveal displacement toward the disc was 137.7 ± 110.7 µm, there was no significant correlation between the stereoacuity and the nasal displacement (Table 1).
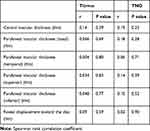 |
Table 1 Correlations Between Stereoacuity and Retinal Thickness and Foveal Shift Toward the Disc |
Discussion
The postoperative stereoacuity in patients with a unilateral idiopathic macular hole that was closed by MH surgery with ILM peeling was significantly correlated with the postoperative BCVA. A younger age and smaller size MH were also significantly correlated with a better stereoacuity. However, the postoperative microstructural changes of the fovea such as the thicker nasal retina and thinner temporal one and foveal displacement toward the optic disc were not significantly correlated with the postoperative stereoacuity.
The stereoacuity has been reported to be reduced in the presence of a unilateral MH with some recovery after closure by vitrectomy.5,6,20,21 However, the number of eyes with a preoperative BCVA better than 6/60 was only 6 in 15 eyes with successful surgery.5 Both the pre- and postoperative visual acuities were worse than those in this study. Cases with cataract requiring combined phacoemulsification and intraocular lens implantation were excluded in that study. Vitrectomy combined with cataract surgery for an MH is often done for elderly patients in Japan, and the stereopsis after phacovitrectomy for an MH has been well studied.6,21 The results showed that a better postoperative stereopsis was significantly correlated with better pre- and postoperative BCVA, smaller size of MH, and a shorter duration of the MH.6,21 Our results are in agreements with these findings.
The mean postoperative stereoacuties, 63.8 sec of arc with Titmus and 169.8 sec of arc with TNO, were much better than that reported.5,6 In general, the stereoacuity decreases with increasing age.22,23 Moreover, the stereoacuity measured by TNO is generally significantly poorer than that determined by other stereoacuity tests. Interestingly, the mean stereoacuity in our cohort was not worse than that reported for elderly individuals.22,23 There were some differences in the age and the size of the MH between the TST and TNO stereotests. This may be due to the different index sizes of both tests. The stimulus used for fine stereopsis in the TNO stereotests is much larger than the Titmus circles. In general, the stereoacuity determined by TNO was worse than that by TST. Moreover, the TNO test is more likely to be influenced by the contrast sensitivity of the eye. The discrepancies in the correlations of the stereoacuity and age and size of MH may arise from these factors.
More recently, Okamoto et al investigated the pre- and postoperative stereopsis in patients with MH.24 The mean preoperative TST value was 2.72 ± 0.53 log units and it improved significantly after surgery to 2.19 ± 0.35 log units (P <0.0001).24 The mean TNO stereoacuity value also improved from 2.82 ± 0.65 log units to 2.32 ± 0.41 log units (P <0.0001).24 The TST value in our cohort was 1.81 ± 0.24 log units which was better than that in their patients although the patients tested with TNO were similar. This discrepancy may be due to the better BCVA in our patients. We included eyes with postoperative BCVA better than 20/30 to investigate the relationship between stereopsis and postoperative microstructures.
A good stereopsis requires bifoveal fixation and good BCVA bilaterally.25 Thus, displacements of the fovea toward the optic disc may cause a decrease in the stereoacuities. It has been shown that the status of the macula was significantly associated with the postoperative displacement of retina after surgery for macula-off retinal detachment.26 This means that macula-off retinal detachment patients could have had a displacement of the retina even after postoperative reattachment which may disrupt the foveal fixation even though none of our patients had diplopia.
The foveal displacement toward the disc after MH surgery with ILM peeling was analyzed earlier by SD-OCT.12 The authors showed that macula was displaced 0.1 disc diameters or 150–160 µm. We reported that the mean displacement was 135.5 µm.15 Similar nasal displacements have been confirmed by several studies.13,14 The nasal and inferior displacements of the fovea have been detected by optical coherence tomography angiography (OCTA).27–29 We suggest that the nasal displacement of the fovea after MH surgery with ILM peeling may affect the postoperative stereopsis. However, there was no significant correlation between the distance of the nasal displacement and stereopsis for both the TST and TNO tests in our cohort. We suggest that the minimum (137.7 µm) foveal displacement may not affect stereoacuity.
The postoperative parafoveal retinal thickness was not significantly correlated with the BCVA although the nasal retina was thicker and the temporal retina was significantly thinner after surgery with ILM peeling.8,11 On the other hand, the BCVA was associated with the status of the outer retinal layer and microstructures, ie, intact external outer limiting membrane, ELM, ellipsoid zone, EZ, and interdigitation zone (IDZ) after successful closure of MH.14 We also examined these microstructural features. The EL and EZ were preserved in all 40 eyes (data not shown). On the other hand, the lack of the IDZ after surgery was found in some cases. Unfortunately, the presence of the IDZ was not confirmed in the other cases in this retrospective study.
There are limitations to this study. We did not evaluate the stereopsis of the patients before they developed the unilateral MH. Second, this was a retrospective study and the number of patients studied was small which may have affected the reliability of the statistical analyses. Third, the analyses were based on the findings at 6 months or more after the MH surgery. The durations of stereotests after surgery were different in each eye. Thus, our results do not reflect the long-term outcomes. Fourth, a single surgeon performed all the surgeries which may limit the broad conclusions. Further prospective studies will be necessary to confirm our results.
Conclusions
A better, but not normal, postoperative stereopsis was found in eyes with better BCVA after MH surgery with ILM peeling. The better postoperative stereopsis was correlated with a younger age, smaller size of MH, and a better postoperative BCVA but not with the foveal shape or the degree of nasal displacement. Thus, stereopsis is preserved after PPV with ILM peeling even though foveal morphological changes had occurred.
Provenance and Peer Review
Not commissioned; externally peer reviewed.
Ethics Approval
Ethics approval was provided by the Institutional Review Board of the Matsumoto Dental University, Shiojiri, Japan.
Patient Consent
Obtained
Acknowledgment
We thank Professor Emeritus Duco Hamasaki of the Bascom Palmer Eye Institute, University of Miami, FL for editing the manuscript.
Disclosure
The authors declare no competing interests.
References
1. Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes: results of a pilot study. Arch Ophthalmol. 1991;109(5):654–659.
2. Brooks HL
3. Christensen UC, Kroyer K, Sander B, et al. Value of internal limiting membrane peeling in surgery for idiopathic macular hole stage 2 and 3: a randomized clinical trial. Br J Ophthalmol. 2009;93(8):1005–1015. doi:10.1136/bjo.2008.151266
4. Lois N, Burr J, Norrie J, et al. Internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole: a pragmatic randomized controlled trial. Invest Ophthalmol Vis Sci. 2011;52(3):1586–1592. doi:10.1167/iovs.10-6287
5. Mireskandari K, Garnham L, Sheard R, Ezra E, Gregor ZJ, Sloper JJ. A prospective study of the effect of a unilateral macular hole on sensory and motor binocular function and recovery following successful surgery. Br J Ophthalmol. 2004;88(10):1320–1324. doi:10.1136/bjo.2004.042093
6. Hikichi T, Onodera A, Ishiko S, Mori F, Yoshida A. Stereo acuity in patients with unilateral macular hole surgery. Graefe’s Arch Clin Exp Ophthalmol. 2001;239(2):128–132. doi:10.1007/s004170100257
7. Itoh Y, Inoue M, Rii T, Hiraoka T, Hirakata A. Correlation between length of foveal cone outer segment tips line defect and visual acuity after macular hole closure. Ophthalmology. 2012;119(7):1438–1446. doi:10.1016/j.ophtha.2012.01.023
8. Ohta K, Sato A, Fukui E. Asymmetrical thickness of parafoveal retina around surgically closed macular hole. Br J Ophthalmol. 2010;94(11):1545–1546. doi:10.1136/bjo.2009.176693
9. Kumagai K, Ogino N, Furukawa M, et al. Retinal thickness after vitrectomy and internal limiting membrane peeling for macular hole and epiretinal membrane. Clin Ophthalmol. 2012;6:679–688. doi:10.2147/OPTH.S30288
10. Kumagai K, Hangai M, Larson E, Ogino N. Progressive changes of regional macular thickness after macular hole surgery with internal limiting membrane peeling. Invest Ophthalmol Vis Sci. 2013;54(7):4491–4497. doi:10.1167/iovs.13-11662
11. Ohta K, Sato A, Fukui E. Retinal thickness in eyes with idiopathic macular hole after vitrectomy with internal limiting membrane peeling. Graefes Arch Clin Exp Ophthalmol. 2013;251(5):1273–1279. doi:10.1007/s00417-012-2173-7
12. Kawano K, Ito Y, Kondo M, et al. Displacement of foveal area toward optic disc after macular hole surgery with internal limiting membrane peeling. Eye. 2013;27(7):871–877. doi:10.1038/eye.2013.99
13. Ishida M, Ichikawa Y, Higashida R, Tsutsumi Y, Ishikawa A, Imamura Y. Retinal displacement toward optic disc after internal limiting membrane peeling for idiopathic macular hole. Am J Ophthalmol. 2014;157(5):971–977. doi:10.1016/j.ajo.2014.01.026
14. Itoh Y, Inoue M, Rii T, Ando Y, Hirakata A. Asymmetrical recovery of cone outer segment tips line and foveal displacement after successful macular hole surgery. Invest Ophthalmol Vis Sci. 2014;55(5):3003–3011. doi:10.1167/iovs.14-13973
15. Ohta K, Sato A, Fukui E. Idiopathic macular hole displaced toward optic disc after vitrectomy with internal limiting membrane peeling. J Clin Exp Ophthalmol. 2014;5:2. doi:10.4172/2155-9570.1000332
16. Ohta K, Sato A, Senda N, Fukui E. Comparisons of foveal thickness and slope after macular hole surgery with and without internal limiting membrane peeling. Clin Ophthalmol. 2018;12:503–510. doi:10.2147/OPTH.S154394
17. Gass JD. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995;119(6):752–759. doi:10.1016/S0002-9394(14)72781-3
18. Grover S, Murthy RK, Brar VS, Chalam KV. Normative data for macular thickness by high-definition spectral-domain optical coherence tomography (Spectralis). Am J Ophthalmol. 2009;148(2):266–271. doi:10.1016/j.ajo.2009.03.006
19. Ohta K, Sato A, Senda N, Fukui E. Asymmetrical steepening of the foveal contour after macular hole surgery with internal limiting membrane peeling. Jpn J Ophthalmol. 2016;60(5):388–394. doi:10.1007/s10384-016-0460-2
20. Eckardt U, Eckardt C. Binocular vison in idiopathic macular foramen. Pre-and postoperative findings. Ophthalmologe. 1995;92(5):626–630.
21. Maeno T, Hattori T, Ninomiya Y, et al. Visual function changes in idiopathic macular holes treated by vitrectomy. J Jpn Ophthalmol Soc. 1996;100(1):40–45.
22. Lee S-Y, Koo N-K. Change of stereoacuity with aging in normal eyes. Korean J Ophthalmol. 2005;19(2):136–139. doi:10.3341/kjo.2005.19.2.136
23. Garnham L, Sloper JJ. Effect of age on adult stereoacuity as measured by different types of stereotest. Br J Ophthalmol. 2006;90(1):91–95. doi:10.1136/bjo.2005.077719
24. Okamoto F, Morikawa S, Moriya Y, et al. Vision-related parameters that affect stereopsis in patients with macular hole. Sci Rep. 2020;10:2805. doi:10.1038/s41589-020-59844-0
25. Wright LA, Cleary M, Barrie T, Hammer HM. Motility and binocularity outcomes in vitrectomy versus scleral buckling in retinal detachment surgery. Graefes Arch Clin Exp Ophthalmol. 1999;237(12):1028–1032. doi:10.1007/s004170050340
26. Shiragami C, Shiraga F, Yamaji H, et al. Unintentional displacement of the retina after standard vitrectomy for rhegmatogenous retinal detachment. Ophthalmology. 2010;117(1):86–92. doi:10.1016/j.ophtha.2009.06.025
27. Cho JH, Yi HC, Bae SH, Kim H. Foveal microvasculature features of surgically closed macular hole using optical coherence tomography. BMC Ophthalmol. 2017;17:217. doi:10.1186/s12886-017-0607-z
28. Kumgai K, Ogino N, Furukawa M, Ooya R, Horie E. Early centripetal displacements of capillaries in macular region caused by internal limiting membrane peeling. Clin Ophthalmol. 2018;12(4):755–763. doi:10.2147/OPTH.S158826
29. Akahori T, Iwase T, Yamamoto K, et al. Macular displacement after vitrectomy in eyes with idiopathic macular hole determined by optical coherence tomography angiography. Am J Ophthalmol. 2018;189(5):111–121. doi:10.1016/j.ajo.2018.02.021
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

