Back to Journals » Research and Reports in Tropical Medicine » Volume 10
Soil-Transmitted Helminths And Other Intestinal Parasites Among Schoolchildren In Southern Ethiopia
Authors Eyamo T, Girma M, Alemayehu T , Bedewi Z
Received 29 March 2019
Accepted for publication 10 October 2019
Published 24 October 2019 Volume 2019:10 Pages 137—143
DOI https://doi.org/10.2147/RRTM.S210200
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Mario Rodriguez-Perez
Tilahun Eyamo,1 Mekonnen Girma,2 Tsegaye Alemayehu,2 Zufan Bedewi1
1Department of Biology, Hawassa University College of Natural and Computational Sciences, Hawassa, Ethiopia; 2School of Medical Laboratory Sciences, Hawassa University College of Medicine and Health Sciences, Hawassa, Ethiopia
Correspondence: Tsegaye Alemayehu
School of Laboratory Sciences, Hawassa University, Hawassa 1560, Ethiopia
Tel +2519-13-872-24-12
Email [email protected]
Background: Intestinal parasitic infections are the neglected tropical diseases that have a devastating effect and leads to malnutrition, morbidity and mortality in schoolchildren. The aim of this study was to determine the presence of soil-transmitted and other intestinal parasites among schoolchildren in southern Ethiopia.
Methods: A cross-sectional study was conducted in Gara Riketa primary school children at Hawassa Tula Sub-City, Southern Ethiopia from March 1 to April 20, 2017. The parent of participating children was interviewed with a structured questionnaire to collect the sociodemographic and risk factors data. Well-trained laboratory technicians were involved in the stool examination through direct and concentration methods. The data were entered and analyzed using SPSS version 20. ORs at 95% CI were considered as a statistically significant association with a p-value < 0.05.
Results: Out of 384 schoolchildren enrolled for the study, 260 (67.7%) were infected with one or more intestinal parasites. The predominantly identified parasite was Ascaris lumbricoides 146 (38.0%) followed by hookworms 12 (3.1%). The study showed that intestinal parasitic infections have a statistically significant association with being in 4th grade, the mother´s educational status (grade 9–12), having cut nails and washing hands before eating.
Conclusion: The rates of soil-transmitted helminths and other intestinal parasitic infections were very high in Gara Riketa primary school children. Based on the statistical analysis, hygiene and nail clipping are important habits to prevent infection with intestinal parasites.
Keywords: Hawassa, intestinal parasites, prevalence, risk factors, schoolchildren
Introduction
Intestinal parasitic infections (IPIs) have a profound impact on human public health and development, affecting approximately one-third of the world’s population, causing high mortality rate mostly in pre and schoolchildren. Some intestinal parasites have significant clinical consequences while others can live for long periods in the bowel without causing any symptoms and requiring treatment.1 IPIs are most common among school-age children who tend to harbour the highest intensities of infection.2
Soil-transmitted helminths (STHs) and intestinal parasitic protozoa cause a significant amount of morbidity, discomfort and often mortality in tropical and sub-tropical regions of the world.3 IPIs can cause a variety of symptoms including abdominal bloating, cramps, constipation, diarrhoea, lack of appetite and vomiting.4 Diagnostic methods for these parasites include laboratory-based examination in which ova, larva, cysts or trophozoites stage detected from a stool sample.5
The rates of IPIs vary in different parts of the world and are particularly high in developing countries where there are poor hygienic conditions and poverty.6 The rates of IPIs vary in different parts of the world. Among primary school children in African countries, the rates of IPIs were reported to be from 19.7% to 90.4%.7–9
Despite continuous efforts to control IPIs during the past decade, IPI infections remained high in Ethiopia.10 In Ethiopia, several studies reported that the prevalence of IPIs varied from 27.7% to 81.0%.11–15 The high rates could be due to low socioeconomic status, poor hygienic conditions, impure drinking water, and a low literacy rate of parents and the large size of the families. This study aimed to determine the rates and associated risk factors of STHs and other IPIs among primary school children in Southern Ethiopia.
Materials And Methods
A cross-sectional study was conducted among Gara Riketa primary school children in southern Ethiopia, Tula Sub-City from March 1-April 20, 2017. Tula Sub-City is located 10 km away from Hawassa, the capital city of Southern Nation Nationality People’s Region (SNNPR). Hawassa is located on the shores of Lake Hawassa, which is one of the Great Rift Valley lakes and 270 km away from Addis Ababa, the capital city of Ethiopia.
In 2017 at Gara Riketa primary school, there were approximately 1711 students registered from grade 1 to 8. Table 1 indicates the number of registered students by grade as well as the number of students randomly selected using a simple crisscross formula.
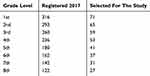 |
Table 1 Total Number Of Registered Gara Riketa Primary School Students In Southern Ethiopia By Grade, And Number By Grade Randomly Selected For Intestinal Parasite Study, March 1-April 20, 2017 |
In total, 384 children were selected for this study. The population that needed to be sampled in this study was defined based on the number of registered students in the school as well as the number in each grade level. Those children who had been treated for any kind of intestinal parasitic infection three months before the start of the study were excluded. Then from each grade level and classes, the participants were chosen using random sampling techniques until the calculated sample size was reached. Students who were willing to provide a stool sample, and who were present at school at the time of the sample collection were enrolled.
Permission to participate was also sent to the students’ house to obtain the parent´s permission. If the parent agreed, a person visited them at their house where they received a structured questionnaire. The questionnaire included socio-demographic characteristics (age, sex, grade level, educational status of father and mother and father´s job. It also included risk factors (regular nail cutting, cleaning of water container, hand washing before a meal, presence of a home latrine, hand washing after defection, source of drinking water, source of water for bathing, use of washed fruits and vegetables, storage of food for later use, food storage conditions and awareness of water availability in school compound)).
From stool samples collected, approximately 2 mg of stool was used for direct wet mount microscopic examination to detect motile parasites. Approximately 3000 μg of stool was used for formalin-ether concentration technique to detect ova, larva and cyst stages of the parasites and increase the detection rate when low amounts of ova, larva or cysts were present.5 A single slide was analyzed for each technique. No adult worms or gravid segments were detected.
Data entry and analysis was performed using SPSS version 20. Descriptive statistics were used to calculate the frequency of specific variables, and cross-tabulations were performed to determine significant associations with IPI. Odds ratios with 95% confidence intervals were calculated, and a p-value <0.05 was considered statistically significant. Logistic regression analysis was used to identify independent predictors of IPI.
The study was presented and approved by the Hawassa University Institutional Review Board. The objectives and purpose of the study were explained to the school principal, school board, the Parents-Teachers Association, and a committee of the school and students. Stool samples were taken with the help of trained professional laboratory technicians. Children diagnosed positive for intestinal parasitic infections were referred to the Gara Riketa health centre for deworming.
Results
A total of 384 school children were enrolled for the study, of whom 199 (51.8%) were male. Students from 10 to 14 years of age and 1st-grade students were those most frequently recruited, 179 (46.6%) and 71(18.5%), respectively. Most fathers and mothers were educated from 9th through 12th grade; 117 (30.5%) fathers and 127 (33.1%) mothers were able to read and write. The occupational status of the fathers was either farming or other private employments 343 (89.3%), while the rest were government employers (Table 2).
In the bivariate analysis, the following characteristics showed significant association with STHs & other IPIs. That is being a 4th grade student (cOR = 3.87, 95% CI (1.32–11.33), P = 0.014), educational status of the mother being 9th to 12th grade (cOR = 0.159, 95% CI (0.033–0.767), P = 0.022) and educational status of the father being 1st to 4th grade (cOR = 0.325, 95% CI (0.123–0.857), P = 0.023). However, in the multivariate analysis only being a 4th grade student (aOR = 4.5 95% CI (1.4–14.7), P = 0.012) and being a mother with 9th to 12th grade education (aOR = 0.14 95% CI (0.03–0.70), P = 0.017) were significantly associated with presence of STHs and other IPIs. The former was associated with increased risk and the latter was associated with decreased risk (Table 2).
The distribution of different potential risk factors for STHs and other IPIs presented in Table 3 showed that, 239 (62.2%) of the children cut their nails regularly, 315 (82%) cleaned their water storage container, 214 (55.7%) practised hand washing before a meal and 347 (90.4%) used a home latrine. In addition, 280 (72.9%) practised hand washing after defecation; 312 (81.3%) got water from hand pumps; 238 (62.0%) take a bath with river water; 291 (75.8%) use washed fruit and vegetables; 338 (88.0%) store food for later use; and 370 (96.4%) use covers to store food.
In the bivariate analysis, the following behaviors were associated with risk of IPIs: not cutting nails regularly (cOR = 0.06, 95% CI, 0.029–0.132, P = 0.000), not cleaning the water container (cOR = 0.100, 95% CI, 0.036–0.28, P = 0.000), and not washing their hand before a meal (cOR = 8.29 95% CI, 4.8–14.5, P = 0.000). However, in multivariate analysis, only not cutting nails regularly (aOR = 0.113, 95% CI, 0.05–0.26, P = 0.000) and not washing hands before a meal (aOR = 3.41, 95% CI, 1.8–6.46, P = 000) were significantly associated with STHs and other IPIs.
STHs and other IPIs identified in the study were Ascaris lumbricoides (A. lumbercoides), 146 (38.0%), Giardia duodenalis (G. duodenalis), 55 (14.3%), Entamoeba histolytica/dispar (E. histolytica/dispar), 26 (6.8%), hookworms, 12 (3.1%), Trichuris trichiura (T. trichiura), 5 (1.3%), Schistosoma mansoni (S. mansoni), 4(1.0%) and Taenia spp., 1 (0.3%).
Mixed infections due to one or more helminths were identified from 37 (9.6%) cases and included: A. lumbricoides + hookworms (16 cases). A. lumbricoides + T. trichiura (13 cases); A. lumbricoides + S. mansoni (4 cases); Hookworms + S. mansoni (1 case); A. lumbricoides + hookworms + T. trichiura (1 case); A. lumbricoides + Teania species + hookworms + S. mansoni (1 case); A. lumbricoides + Teania species +S. mansoni (1 case). Mixed protozoa infections were identified from one of the study participants in which both E. histolytica/dispar and G. duodenalis was detected (Table 4).
 |
Table 4 Total Parasites Isolated By Sex From A Study Of STHs And Other IPIs Among Schoolchildren In Southern Ethiopia From March 1 To April 20, 2017 |
Discussions
This study was performed to determine the prevalence of IPIs and associated risk factors among schoolchildren in Gara Riketa primary school. Due to their poor immune status, their contact with soil and other contaminated materials, and non-compliance with health standards, the prevalence of IPIs were high among children, making them vulnerable to parasite infection.16 Of note, the transmission of some IPIs from infected to non-infected individuals was highly prevalent in communities with high population density.17 The highest levels of infection in communities may be related to school children.18
Millions of school children around the world suffer from different complications of IPIs. These parasites can cause malnutrition, nausea, vomiting, dysentery, anaemia, avitaminosis, loss of immune defence and reduced physical growth.19 Infection with IPIs has been reported across all age groups, but many reports indicate that it is more common in school-age children than other age groups.18 In this study, the highest rates of infections were found in children between 10 and 14 years old and those in 1st, 6th and 4th grades, with a prevalence of 71.8%, 73.0%, and 84.9%, respectively.
The overall prevalence of STH & other intestinal parasites of 67.7% was comparatively similar to reports from Bahir-Dar12 and South Africa,7 but lower than other studies of school children from different parts of Ethiopia.10,11,13–15 Our prevalence was higher when compared with other studies in Ethiopia reported from schoolchildren.20–27 Studies in different countries reported a higher rate, including studies from central Sudan,9 Nigeria28 and in Yemen.29 Differences in parasite prevalence might be due to multiple factors including sample size, climatic condition, geography, and study period.
In terms of specific parasites, the rate of infection with A. lumbricoides was 38%, which is lower compared to a study of primary school children in Chencha town.15 In contrast, other studies elsewhere reported lower rates of A. lumbricoides.7,23,26,30–34 These differences might be due to study period difference, geographical location, and ecological factors, as well as economic, social, and cultural factors. The rate of infection with G. duodenalis was 14.3%, comparable to Ethiopian studies conducted elsewhere.12,15,25 In contrast, higher rates were reported from Amhara region13,33 and a lower rate was reported from Adigrat.14 The prevalence of E. histolytica/dispar was 6.8%, comparable with studies from South Eastern Ethiopia,21 and Adigrat,35 but lower than studies reported from primary school children in Chencha town,15 from the Amhara Region.12,14 These differences might be due to personal and environmental hygiene-related factors among schoolchildren and the community.
According to our results, those who were 4th-grade students were 4.5 times more likely to be infected with IPIs, as compared with 1st grade students. These results contrast to other studies of primary school children performed at Dona Berber in Bahir Dar12 and in Debre Elias, North West Ethiopia.11 We also found that those who cut their nails regularly were less likely to be affected by IPIs, in agreement with studies conducted in North West Ethiopia,27 Amhara region,14 Eastern Ethiopia21 and Bahir Dar.12 In contrast to our finding, a study from Adigrat reported as an insignificant association. The increased risk associated with not cutting nails regularly might reflect a lack of full information about the transmission and control mechanisms of IPIs and less parental support for personal hygiene. In multivariate analysis, a child with a mother whose educational level was a grade (9–12) was less likely affected by IPIs, in contrast to a study from elsewhere.11,27 This association in our study may reflect increased awareness of the mother about means of IPI transmission. We also found that those who did not practice hand washing before a meal were 3.4 times more likely to be affected by IPIs, which was in agreement with a number of other studies from different parts of Ethiopia.12,14,25 However, a different study from South Eastern Ethiopia did not detect a significant relationship between hand washing before a meal and parasitic infection.21
Limitations Of The Study
There were a number of limitations that should be noted in this study. First, the study was conducted on a single stool specimen and using a single slide per technique. Secondly, stool specimens were collected randomly without time specification. Third, only direct and concentration techniques were employed for the diagnosis of intestinal parasites. Finally, we did not detail the stages of parasites and other details from the examination of the stool.
Conclusions
In summary, we found a very high rate of STHs and other intestinal parasitic infections in Gara Riketa primary school children. The most common parasite identified was A. lumbricoides and the least commonly identified parasite was Taenia spp. Being a 4th-grade student and not washing hands before a meal were identified as risk factors for STHs & IPIs while practicing regular nail cutting and having a mother with 9th to 12th -grade education had a protective effect. Our findings support the importance of school-age children of targeting personal and environmental sanitation to help reduce IPI prevalence.
Ethical Clearance
Ethical clearance was obtained from Hawassa University institutional review board and permission from the school committee was obtained. Consent and assent were asked and signed by student and parents. Those who were positive were treated accordingly. This study was conducted in accordance with the declaration of Helsinki.
Availability Of Data And Material
All the raw data supporting the findings can be obtained from all of the authors.
Acknowledgements
We would like to thanks Hawassa University for funding, Gara Riketa primary school staffs, parents and the students for their hospitality and Mr. Alegntaw Abate for his genuine laboratory diagnosis. The study was partially funded by Hawassa University for data collection and laboratory diagnosis.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kidane E, Menkir S, Kebede A, Desta M. Prevalence of intestinal parasitic infections and their associations with anthropometric measurements of school children in selected primary schools, Wukro Town, Eastern Tigray, Ethiopia. Int J Curr Microbiol Appl Sci. 2014;3(3):11–29.
2. Sah RB, Bhattarai S, Yadav S, Baral R, Jha N, Pokharel PK. A study of prevalence of intestinal parasites and associated risk factors among the school children of Itahari, Eastern Region of Nepal. Trop Parasitol. 2013;3(2):140. doi:10.4103/2229-5070.113888
3. Khanal L, Choudhury D, Rai S, et al. Prevalence of intestinal worm infestations among school children in Kathmandu, Nepal. Nepal Med Coll J. 2011;13(4):272–274.
4. Cook GC, Zumla A, Manson P
5. Cheesbrough M. District Laboratory Practice in Tropical Countries, Part 1.
6. Ziegelbauer K, Speich B, Mäusezahl D, Bos R, Keiser J, Utzinger J. Effect of sanitation on soil-transmitted helminth infection: systematic review and meta-analysis. PLoS Med. 2012;9(1):e1001162. doi:10.1371/journal.pmed.1001162
7. Nxasana N, Vasaikar S, Longo-Mbenza B, Apalata T. Epidemiology of intestinal parasites among school children in Mthatha, South Africa. J Innovation Res Health Sci Biotechnol. 2015;1(1):25–30.
8. Mwenji MB. The Influence of Intestinal Parasites on Academic Performance among Primary School Children in Nairobi Province. Kenya: Kenyata Univercity Institutional Reporsitory; 2011.
9. Abdel-Aziz MA, Afifi AA, Malik EM, Adam I. Intestinal protozoa and intestinal helminthic infections among schoolchildren in Central Sudan. Asian Pac J Trop Med. 2010;3(4):292–293. doi:10.1016/S1995-7645(10)60071-5
10. Legesse M, Erko B. Prevalence of intestinal parasites among schoolchildren in a rural area close to the southeast of Lake Langano, Ethiopia. Ethiop J Health Develop. 2004;18.
11. Workneh T, Esmael A, Ayichiluhm M. Prevalence of intestinal parasitic infections and associated factors among Debre Elias primary schools children, East Gojjam Zone, Amhara Region, North West Ethiopia. J Bacteriol Parasitol. 2014;5(1):1. doi:10.4172/2155-9597.1000181
12. Hailegebriel T. Prevalence of intestinal parasitic infections and associated risk factors among students at Dona Berber primary school, Bahir Dar, Ethiopia. BMC Infect Dis. 2017;17(1):362. doi:10.1186/s12879-017-2757-2
13. Ayalew A, Debebe T, Worku A. Prevalence and risk factors of intestinal parasites among Delgi school children, North Gondar, Ethiopia. J Parasitol Vector Biol. 2011;3(5):75–81.
14. Alamir M, Awoke W, Feleke A. Intestinal parasites infection and associated factors among school children in Dagi primary school, Amhara National Regional State, Ethiopia. Health. 2013;5(10):1697–1701. doi:10.4236/health.2013.510228
15. Abossie A, Seid M. Assessment of the prevalence of intestinal parasitosis and associated risk factors among primary school children in Chencha town, Southern Ethiopia. BMC Public Health. 2014;14(1):166. doi:10.1186/1471-2458-14-166
16. Davami M, Kazaii M, Eslamirad Z, MODARESI M, MOUSTOFI M. An investigation on intestinal parasitic infections and the effective demographic factors in children (1–13 years) in Shahrak-e-valiasr Arak during 1999. Arak Med Univ J. 2002;5(2):5–10.
17. Heravi MM, Rasti S, Vakili Z, Moraveji A, Hosseini F. Prevalence of intestinal parasites infections among Afghan children of primary and junior high schools residing Kashan city, Iran, 2009–2010. Iran J Med Microbiol. 2013;7(1):46–52.
18. Kousha A, Hakimi S, Fallah E, Nokhahi I, Sarafraz S, Shahnami A. Prevalence of intestinal parasites among symptomless primary school children attending urban health centers, Tabriz. Med J Tabriz Univ Med Sci. 2011;33(3):15.
19. Barazesh A, Fouladvand M, Tahmasebi R, Heydari A, Kooshesh F. Prevalence of intestinal parasitic infections among primary school children in Bushehr, Iran. Avicenna J Clin Microbiol Infect. 2017;4:1.
20. Yami A, Mamo Y, Kebede S. Prevalence and predictors of intestinal helminthiasis among school children in Jimma zone; a cross-sectional study. Ethiop J Health Sci. 2011;21(3):167–174.
21. Tulu B, Taye S, Amsalu E. Prevalence and its associated risk factors of intestinal parasitic infections among Yadot primary school children of South Eastern Ethiopia: a cross-sectional study. BMC Res Notes. 2014;7(1):848. doi:10.1186/1756-0500-7-848
22. Tadesse G. The prevalence of intestinal helminthic infections and associated risk factors among school children in Babile town, eastern Ethiopia. Ethiop J Health Develop. 2005;19(2):140–147. doi:10.4314/ejhd.v19i2.9983
23. Haftu D, Deyessa N, Agedew E. Prevalence and determinant factors of intestinal parasites among school children in Arba Minch town, Southern Ethiopia. Am J Health Res. 2014;2(5):244–247. doi:10.11648/j.ajhr.20140205.15
24. Gebrselassie M, Tomas Z. Prevalence of intestinal parasites and associated risk factors in school children of Aksum Town, Northern Ethiopia. Acta Parasitologica Globalis. 2015;6(1):42–48.
25. Gebremichael G. Prevalence of intestinal parasites and associated risk factors among schoolchildren of Homesha District (Woreda) in Benishangul-Gumuz Regional State, Western Ethiopia. J Fam Med Health Care. 2016;2(4):57–64. doi:10.11648/j.jfmhc.20160204.16
26. Fetlework A. Prevalence and intensity of intestinal parasitic protozoan and soil-transmitted helminths infections in school children in Alemketema Town, central Ethiopia. Int J Sci Technol. 2016;4(6):75–82.
27. Abera A, Nibret E. Prevalence of gastrointestinal helminthic infections and associated risk factors among schoolchildren in Tilili town, northwest Ethiopia. Asian Pac J Trop Med. 2014;7(7):525–530. doi:10.1016/S1995-7645(14)60088-2
28. Oyewole F, Ariyo F, Sanyaolu A, et al. Intestinal helminthiases and their control with albendazole among primary school children in riverine communities of Ondo state, Nigeria. Southeast Asian J Trop Med Public Health. 2002;33(2):214–217.
29. Alwabr GM, Al-Moayed EE. Prevalence of intestinal parasitic infections among school children of Al-Mahweet Governorate, Yemen. Eur J Biol Res. 2016;6(2):64–73.
30. Wegayehu T, Tsalla T, Seifu B, Teklu T. Prevalence of intestinal parasitic infections among highland and lowland dwellers in Gamo area, South Ethiopia. BMC Public Health. 2013;13(1):151. doi:10.1186/1471-2458-13-151
31. Odo G, Agwu J, Ekeh F, et al. Prevalence of intestinal parasites among school children in Uzo-Uwani local governemnt area of Enugu State. Int J Res Stud Microbiol Biotechnol. 2016;2(2):7–14.
32. Monib M, Hassan A, Attia R, Khalifa M. Prevalence of intestinal parasites among children attending Assiut University Chil-dren’s Hospital, Assiut, Egypt. J Advan Parasitol. 2016;3(4):125–131. doi:10.14737/journal.jap/2016/3.4.125.131
33. Gelaw A, Anagaw B, Nigussie B, et al. Prevalence of intestinal parasitic infections and risk factors among schoolchildren at the University of Gondar Community School, Northwest Ethiopia: a cross-sectional study. BMC Public Health. 2013;13(1):304. doi:10.1186/1471-2458-13-304
34. Derso A, Nibret E, Munshea A. Prevalence of intestinal parasitic infections and associated risk factors among pregnant women attending antenatal care center at Felege Hiwot Referral Hospital, northwest Ethiopia. BMC Infect Dis. 2016;16(1):530. doi:10.1186/s12879-016-1987-z
35. Maru DS. Prevalence of intestinal parasitic infections and associated risk factors among school children in Adigrat town, northern Ethiopia. Int J Emer Trends Technol Comp Sci. 2015;4(1):4943–4948. doi:10.18535/ijetst/v4i1.03
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


