Back to Journals » ClinicoEconomics and Outcomes Research » Volume 10
Societal costs due to meningococcal disease: a national registry-based study
Authors Gustafsson N , Stallknecht SE , Skovdal M, Poulsen PB , Østergaard L
Received 30 May 2018
Accepted for publication 27 August 2018
Published 2 October 2018 Volume 2018:10 Pages 563—572
DOI https://doi.org/10.2147/CEOR.S175835
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Samer Hamidi
Nina Gustafsson,1 Sandra Elkjær Stallknecht,1 Mette Skovdal,2 Peter Bo Poulsen,3 Lars Østergaard4
1Incentive, Holte, Denmark; 2Vaccines, Pfizer Denmark, Ballerup, Denmark; 3Health and Value, Pfizer Denmark, Ballerup, Denmark; 4Department of Infectious Diseases, Aarhus University Hospital, Aarhus, Denmark
Purpose: Limited detailed evidence exists on the societal costs of meningococcal disease. The objective of this study was to estimate the average 5-year societal cost of events attributable to meningococcal disease in Denmark.
Methods: The study was based on the nationwide Danish registries. Incident patients diagnosed with meningococcal disease were identified and each matched with two controls, using direct matching on age, gender, and level of education. Siblings constituted a secondary control population where one patient was matched with one sibling control without meningococcal disease. Costs related to health care in the primary and secondary sectors, prescription medicine, municipality home care services and costs of production loss, ie, estimated loss of yearly earnings, were included (1997–2015).
Results: The incidence of meningococcal disease fluctuated between 1980 and 2015. The average attributable societal costs were highest the first year after diagnosis, with costs equaling USD 18,920 per event in the primary study population (matched controls) and USD 16,169 in the secondary study population (sibling controls). Hospital admission costs accounted for 65% and production loss for 30%; however, having a lifetime perspective and including loss due to premature death further increase the costs of meningococcal disease events.
Conclusion: The costs of meningococcal disease are substantial, and the estimated costs of event may be informative in evaluating the impact of preventive interventions targeting meningococcal disease.
Keywords: meningitis, sepsis, national registries, health care, hospitalization, attributable costs of events
Introduction
The bacterium Neisseria meningitidis is transmitted by direct contact and by droplet spread from the nasal pharynx. The bacterium can cause sepsis, meningitis or a combination of the two. Despite strains A, B, C, W135 and Y being preventable by vaccines, meningococcal disease remains a substantial public health burden worldwide.1 It is potentially fatal within 24 hours of onset, with average fatality rates ranging from 10% to 40%, depending on clinical presentation and geographic location.1 Among survivors, up to 20% may experience long-term sequelae, such as amputations, hearing loss and neurodevelopmental disabilities.2 Incidence rates of meningococcal disease are highest in young children, adolescents and young adults.3 Season and geographic location are known to influence incidence, which ranges from <1 case to more than 1,000 cases per 100,000 people.3 In Denmark, the incidence has decreased in the past decades,4,5 from 4.4 per 100,000 in 1994 to 1.9 per 100,000 in 2002.4 A decreasing incidence is also seen in other European countries. In 2014, the overall European incidence was 0.6 per 100,000.6
Detailed evidence on the societal costs due to meningococcal disease is limited. However, a review estimating the cost burden of meningococcal disease outbreaks has concluded that outbreaks are associated with substantial costs.7 In high-income countries, the average cost per small-containment strategy was USD 299,641 (average cost per patient: USD 41,857), whereas the average cost per large-containment strategy was USD 579,851 (average cost per patient: USD 55,755).
There is a lack of European studies investigating the costs of meningococcal disease, and to our knowledge, no published costs of event estimates of meningococcal disease exist. Thus, the objective of this study was to estimate the average 5-year societal cost of events attributable to incident patients with meningococcal disease in Denmark.
Materials and methods
We applied an incidence-based approach to identify cases of meningococcal disease between 1980 and 2015, as well as to estimate the costs attributable to incident patients diagnosed with meningococcal disease between 1997 and 2015.
Registry data sources
The analyses were based on the nationwide Danish registries covering all Danish residents. In Denmark, there is a long tradition of maintaining registries that provide detailed and exhaustive records, including various types of information at the individual level covering the entire population. Every resident has a personal and permanent identification number (a social security number), which enables linkage between the different registries. The Danish National Patient Registry contains information on all admissions and outpatient visits to hospitals, and it includes diagnosis codes according to the ICD, 10th revision (ICD-10).8 All individual contacts to general practitioners (GPs) and private practicing specialists are registered in the National Health Insurance Service Registry.9 The Registry of Medical Product Statistics includes high-quality data on all prescription drugs sold in community pharmacies applying the Anatomical Therapeutic Chemical Classification System, an international therapeutic chemical classification system.10 The Danish longitudinal database on employment (DREAM database) has information on weekly labor market-related public transfer payments for all Danish residents.
Study population
Incident patients diagnosed with meningococcal disease between 1980 and 2015 were identified in the National Patient Registry. Identification of patients was conditioned on at least one hospital contact (admission, outpatient or emergency room visit) with a primary diagnosis of meningococcal disease (from 1980 to 1993, ICD-8 code 036 “meningococcal infection”, excluding 03612 “chronic meningococcaemia”; from 1994 to 2015, ICD-10 code A39 “meningococcal infection”, excluding A393 “chronic meningococcaemia”). The incidence date was defined as the date of the first hospital contact with meningococcal disease.
Potential controls were identified in the Danish Civil Registration System containing all persons alive and living in Denmark. For each identified case with meningococcal disease, two controls from the general population were selected randomly using direct matching on age and gender, as well as parents’ educational level (in individuals <25 years at the time of diagnosis) or the patient’s own educational level (in individuals ≥25 years at the time of diagnosis). In patients <25 years at the time of diagnosis, we matched on the parents’ educational level instead of the patient’s own educational level as they most likely will be on their way with their own education. Cases were matched with potential controls at the beginning of each calendar year. Thus, a few controls might have died before the incidence date of the case. Siblings with the same registered mother and father as the patient with meningococcal disease constituted a secondary control population. Sibling controls were conditioned on ≤5 years’ difference in age between the case and the sibling control, and if more than one sibling control existed, the one closest in age to the case was chosen. To account for differences in age between the case and the sibling control, we assigned an age-adjusted incidence date to the sibling control, where the control was of the same age as the case at incidence. This ensured that all analyses were performed when the case and the sibling control were of the same age.
Costs
A societal perspective was applied to this study, including both direct and indirect costs. Health care costs comprised the costs in the primary health care sector, including contacts with the GP and other private practicing health care professionals reimbursed by the public health insurance system, as well as the costs in the secondary health care sector, including costs of admissions, outpatient and emergency department visits at the hospital, applying the Diagnosis-Related Group (DRG) and the Danish outpatient Danish Outpatient Grouping System (Dansk Ambulant GrupperingsSystem [DAGS]) charges, respectively. Additionally, prescription medicine costs were included, using pharmacy selling prices (including the Danish value-added tax of 25%) and covering both the public reimbursement and the patient co-payment.
Municipality-provided home care costs were estimated as the allocated hours of home nursing and practical services in the home multiplied by hourly wages for social and health care workers in private homes obtained from Statistics Denmark.11 Data on allocated home care are available only from 2008 and onwards in the Municipalities Electronic Record system. Thus, estimated home care costs are based on a smaller study population.
Yearly employment rates were estimated using the DREAM database, and production values were estimated by multiplying the yearly employment rate with gender-specific gross average annual wages adjusted for the number of effective weekly working hours among males and females.12,13 Only cases and controls between 18 and 65 years of age in a given year were included in the estimation of production loss, as this age range constitutes the majority of the workforce in Denmark.
All costs were inflated to 2015 prices and converted to USD based on the average exchange rate in 2015: USD 1=DKK 6.73.14 Fees in the secondary sector from the National Health Insurance Service Registry, as well as DAGS and DRG charges in the primary sector from the National Patient Registry, were inflated using the relevant combined price and wage index for health care services estimated by the Danish regions.15 Prescription medicine prices were not inflated because the price index inexplicably fluctuates. Production loss and home care costs were estimated using wage indices from 2015.
Statistical analyses
The average 5-year societal costs of meningococcal disease events were estimated on the individual level as actual, direct and attributable costs. All cost components were reported separately as primary sector costs, outpatient costs, hospital admission costs, prescription medicine costs, home care costs and production loss.
Average actual costs are defined as average health care costs in a given year before or after diagnosis. Average direct costs were estimated as the average actual costs among patients with meningococcal disease in a given year minus the average actual costs among controls in the same year. Average total costs are defined as the average actual costs in year t after the diagnosis minus the average actual costs in the baseline year (year 0), ie, the year before the incidence date. The average attributable costs were estimated by applying a difference-in-difference approach, where the average total costs among individuals in the control groups were subtracted from the average total costs among patients with meningococcal disease.
Patients and controls were censored at death and by the end of data access (ie, by the end of 2015), and the individual was included with a weight corresponding to the fraction of the year he or she was available in the data. If an individual died before the conclusion of the study, both the case and the control(s) were censored.
All statistical analyses were conducted in SAS version 9.4 on Statistics Denmark’s research computers via a remote server. To ensure data protection, Statistics Denmark anonymized the data prior to data access.
Simulation of future costs
The future costs due to meningococcal disease were estimated in a simulation model with projections from 2017 to 2060. The simulation was based on elements from the registry-based analysis, Statistics Denmark’s population projections and the estimated net present value of net consumption, including production loss due to premature death, presented in the study by Kruse et al16 The future incidence of meningococcal disease and the occurrence of premature death by age groups were projected based on the average observed incidence and occurrence of premature death in the most recent years multiplied by the population projection. Premature death was defined as the excess mortality within 2 weeks of patients with meningococcal disease. The projected incidence of meningococcal disease and the occurrence of premature death were multiplied by cost estimates found in the cost analysis and estimates of lost production and consumption due to premature death, presented in the study by Kruse et al.16 We estimated two scenarios. The first scenario was based on average attributable costs, ie average total costs for cases minus average total costs for controls, and average attributable production loss, ie average total production for cases minus average total production for controls, as well as the net present value of net consumption as an estimate of loss due to premature death. This scenario was rather conservative. The second scenario was based on average direct health care costs, ie average actual costs for cases minus average actual costs for controls, and average direct production loss, ie, average actual production for cases minus average actual production for controls, as well as production loss due to premature death. Both scenarios were based on cost estimates for the primary study population and presented in fixed 2015 prices.
Ethical considerations
Approval from the Danish Ethics Committee was not required by Danish law because the study applied only retrospective anonymized registry data.
Results
A total of 6,303 incident patients with meningococcal disease were identified during the period from 1980 to 2015 (54% males; mean age in years [SD]: 17.08 [21.06]). In Denmark, the incidence fluctuated during this period, with the highest incidence in 1987 (6.1 per 100,000 persons) and the lowest incidence in 2015 (0.7 per 100,000 persons) (Figure 1). We found a significant increased HR of dying of 2.20 (95% CI: 2.01–2.40) at any time after the diagnosis in patients with meningococcal disease compared with matched controls (Cox regression adjusted for age and gender, data not shown).
The target study population consisted of 6,303 cases diagnosed with meningococcal disease between 1980 and 2015. In the primary target study population, 20 of the assigned controls died before the incidence date of the matched patient with meningococcal disease. Because of limited existence of cost variables in the registries prior to 1997, the cost analyses had to be restricted to patients diagnosed between 1997 and 2015, resulting in a further 4,118 excluded cases. Thus, the primary target study population consisted of 2,165 cases and 4,330 controls (Figure 2). The secondary target study population consisted of 3,617 cases diagnosed with meningococcal disease between 1980 and 2015 who had an identifiable sibling with ≤5 years’ age difference. However, 39 sibling controls died before the incidence date of the matched patient with meningococcal disease, and an additional 674 sibling controls were assigned an age-adjusted incidence date outside the data period. Moreover, the limited data existence of cost variables prior to 1997 resulted in a further 2,010 excluded cases for this cost analysis. Thus, the secondary study population consisted of 894 cases and 894 sibling controls (Figure 2).
  | Figure 2 Flowchart of the primary and secondary study populations. |
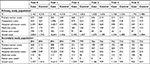
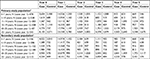
The average actual costs per patient in the year before diagnosis and the first 5 years after diagnosis are presented in Table 1. In general, the differences in actual costs between cases and controls were most profound in the baseline year (case: USD 3,834; control: USD 1,742) and especially in the first year after the meningococcal diagnosis (case: USD 16,641; control: USD 1,426). This also applies to the secondary study population (Table 1). A sensitivity analysis showed that the high costs in the baseline year were not driven by high costs in the month before the registered diagnosis (data not shown). Hospital admission costs were the main driver in the first year after diagnosis (89%). In both the primary and secondary study populations, it was the adult patients, ie patients 20–25 years or 25+ years at the time of the meningococcal diagnosis, who had the highest average costs following their diagnosis (Table 2). These groups were followed by the rather large group of adolescents, aged 15–19 years, with an average actual cost per patient in the first year of USD 16,335 (Table 2). However, the costs in year 1 relative to the baseline year are approximately ten times higher for the age groups 11–19 years, whereas the equivalent relative increases in the age groups 20–25 years and 25+ years are approximately five and three, respectively.
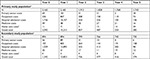
The average direct costs per patient in the year before diagnosis and the first 5 years after diagnosis are presented in Table 3. The average direct costs for cases were highest the first year after the meningococcal diagnosis (primary study population: USD 15,215; secondary study population: USD 13,833). In the second, third, fourth and fifth years after the diagnosis, the costs were all lower than the costs in the baseline year.
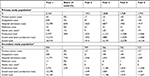
The average attributable costs per patient in the first year after the meningococcal diagnosis were estimated to be USD 18,920 (including production loss) in the primary study population and USD 16,169 (including production loss) in the secondary study population (Table 4). For the primary study population, hospital admission costs accounted for 65% of the total attributable costs in the first year after diagnosis, while production loss accounted for 30%. The contribution of the costs of prescription medicine, home care, primary sector and outpatient visits to the total attributable costs was limited. The negative total costs in the second, third, fourth and fifth years after diagnosis were due to high average actual costs in the baseline year among patients with meningococcal disease.
As the population grows in the coming decades, the future costs of meningococcal disease are estimated to increase too. Based on the data in this study, a conservative estimate on this burden on the one hand showed that the costs in total add up to slightly more than USD 1.5 million per year in 2017, increasing to slightly more than USD 1.7 million per year in 2060, including losses due to premature deaths (Figure 3A). A higher and less conservative estimate on the other hand shows that the costs in total add up to slightly less than USD 4.1 million per year in 2017 and slightly more than USD 4.6 million per year in 2060, including losses due to premature deaths (Figure 3B). For the simulation, the number of premature deaths was estimated based on the average share of premature deaths (defined as within 2 weeks following the diagnosis) in the period 2000–2015, which was about 5%. In the entire study period (1980–2015), about 6% of the cases died prematurely compared to the controls.
Discussion
This study provides estimates of the average 5-year societal costs attributable to incident patients with meningococcal disease in Denmark. The average attributable costs per patient were highest in the first year after the meningococcal diagnosis (USD 18,920 for the primary study population and USD 16,169 for the secondary study population) and negative in the following years. The negative costs in years 2–4 after diagnosis are associated with the observed high average actual costs among cases in the baseline year, which may be explained by more prior comorbidities in the meningococcal population compared with controls (data not shown). Hospital admission costs are a dominant cost driver, and production losses are considerable. Having a lifetime perspective and adding the loss due to premature death further increase the costs of meningococcal disease.
There is a lack of European studies investigating the costs of meningococcal disease. In a study from UK, the authors found that severe cases of meningococcal disease with long-term sequelae can result in costs to the National Health Service and the local authority and Personal Social Services of around GBP 160,000–200,000 (USD 251,643–314,554) in the first year alone (2010–2011 price level).17 In an Italian study, hospitalization costs due to meningococcal disease have been estimated to be EUR 6,800 (USD 9,030) per stay for pediatric patients (average length of stay: 11.40 days) and EUR 8,250 (USD 10,956) per stay for adult patients (average length of stay: 21.64 days) (2013 price level).18 In an Australian study, acute hospitalization costs have been estimated to be AUD 12,311 (USD 12,692) per child at a pediatric hospital (average length of stay: 7.2 days) (2011 price level).19 The total 1-year direct cost burden of initial hospitalizations in patients with meningococcal disease in USA has been estimated to be USD 65,980 (2009 price level).20 In another study from USA, the 1-year health care costs after diagnosis of meningococcal disease have been estimated to be USD 55,702 (2009 price level), including inpatient hospitalizations, emergency department visits, outpatient visits, laboratory tests, prescription drugs, home health care and durable medical equipment services.21 The authors found that the health care costs varied significantly depending on the presence or absence of meningococcal disease-related sequelae during the follow-up year, although inpatient hospitalizations were the largest cost driver regardless of status of disease-related sequelae. Another study has found that the overall average cost of an admission for meningococcal disease was USD 21,891 compared with USD 6,822 for demographically matched control admissions in a population of US children of age <21 years (2009 price level).22 The average cost per admission was highest among infants (<1 year: USD 36,454), followed by young adults (19–20 years: USD 31,433).
Due to structural differences between countries, as well as differences in methodology, study design, population characteristics, time horizon and included costs, and thereby the chosen perspective of the analyses, it is difficult to synthesize and compare the results of this study with cost estimates identified in the literature. Compared with cost estimates from USA,20–22 our estimated average actual health care costs per patient are on the one hand somewhat low; however, our estimates of average actual costs of hospital admissions in year 1 are on the other hand roughly aligned with Italian and Australian cost estimates for hospitalization due to meningococcal disease.18,19
Strengths and limitations
As with every study, there are strengths and limitations with this study regarding design and data. This study has several strengths. First, the use of nationwide registries including all Danish residents means that the study is less prone to selection and information bias; in addition, the data from the national registries are of a high quality. The matched controls were randomly selected from the general population and matched with patients on potential confounders. Thus, the matched controls consisted of both healthy and non-healthy persons (however, free of meningococcal disease) following their representativeness in the Danish society. This identification of controls does not give rise to particular concerns regarding selection bias. Moreover, the registry data entail that there is no loss to follow-up and thus no bias resulting from differential loss to follow-up. Internationally, the Danish registries are considered to be some of the most comprehensive of their kind. The Danish registries contain detailed and exhaustive records at the individual level covering the entire population over a long period of time. This is relatively unique and only some other Nordic countries have the same kind of nationwide registries on their populations. Another strength is the large study population covering all incident cases with meningococcal disease in Denmark between 1997 and 2015, resulting in a high generalizability of the results. Due to the large population, the cost estimates of this study are relatively robust, reducing the risk of random variation. Yet another strength is the broad societal perspective, which includes home care and production loss costs in addition to health care costs.
We acknowledge, however, that the study has some limitations. Not all relevant costs were included, eg, the cost of short-term sick leave, transportation time related to consultations and non-prescription drugs. Moreover, possible costs of informal care contributed by friends and family were not included in the estimation of costs related to meningococcal disease, as these data are not available in the registries. Thus, the presented cost estimates remain conservative. Moreover, it is important to be aware that cost data rarely are normally distributed. This applies in particular to the costs related to home care and production loss, where many patients do not contribute any costs, because far from everyone receives municipality-provided home care, and the majority of people are not in the labor market at the time of diagnosis. Furthermore, there is a risk of misclassification. The identification of patients with meningococcal disease relies on the ICD-10 coding system in the National Patient Registry, which might not be completely accurate. The study aimed to assess the presence of potential confounding by direct matching on age, gender and level of education. However, as in all observational studies without random allocation to the exposure groups, ie, individuals with and without meningococcal disease in this study, unmeasured confounding may still affect validity. Finally, it cannot be ruled out that the matching procedure provides some limitations on the cost analysis comparing the meningococcal population with the controls, which is seen with the greater incidence of prior comorbidities in the meningococcal disease population compared with the controls. In the end, this limits the cost estimates, as the applied method subtracts the high costs in the baseline year from the costs in the first year, etc. In that sense, the conducted cost analysis is conservative.
Conclusion
We found that the societal costs attributable to meningococcal disease events are substantial in the first year after diagnosis. Hospital admission costs and production loss were the main cost drivers. From an age perspective, the analysis shows high actual costs of meningococcal disease per patient that are highest from the age of 14 and onwards. Any kind of preventive activity to target these age groups could therefore be relevant. The costs of event estimates presented in this study may be informative in evaluating the impact of preventive interventions targeting meningococcal disease. Future potential research may include pooled analyses with data from other Nordic countries with similar national registries.
Acknowledgments
This study was supported by Pfizer Denmark. Incentive is a paid vendor of Pfizer Denmark. We would like to acknowledge Jens Olsen from Incentive for his valuable comments and suggestions throughout the research and writing of this paper. Part of the results from the study have been presented as a E-Poster at the 36th Annual Meeting of the European Society for Paediatric Infectious Diseases (ESPID 2018), Malmö, Sweden, May 28–June 2, 2018 (abstract number: ESP18-0806).
Disclosure
Sandra Elkjær Stallknecht and Nina Gustafsson are employees at Incentive. Lars Østergaard was a paid clinical consultant of Pfizer Denmark. Peter Bo Poulsen and Mette Skovdal are employees at Pfizer Denmark. The authors report no other conflicts of interest in this work.
References
Martinón-Torres F. Deciphering the Burden of Meningococcal Disease: Conventional and Under-recognized Elements. J Adolesc Health. 2016;59(2 Suppl):S12–S20. | ||
Pace D, Pollard AJ. Meningococcal disease: clinical presentation and sequelae. Vaccine. 2012;30(Suppl 2):B3–B9. | ||
Stephens DS, Greenwood B, Brandtzaeg P. Epidemic meningitis, meningococcaemia, and Neisseria meningitidis. Lancet. 2007;369(9580):2196–2210. | ||
Howitz MF, Samuelsson S, Mølbak K. Declining incidence of meningococcal disease in Denmark, confirmed by a capture-recapture analysis for 1994 and 2002. Epidemiol Infect. 2008;136(8):1088–1095. | ||
Statens Serum Institut [webpage on the Internet]. Meningococcal Disease, Individual Notifiable Diseases – SSI (Danish: Meningokoksygdom, Individuelle anmeldelsespligtige sygdomme – Statens Serum Institut). Available from: https://www.ssi.dk/Smitteberedskab/Sygdomsovervaagning/Sygdomsdata.aspx?sygdomskode=MENI&xaxis=Aar&show=&datatype=Individual&extendedfilters=False#HeaderText. Published 2018. Accessed February 15, 2018. | ||
Whittaker R, Dias JG, Ramliden M, et al; ECDC network members for invasive meningococcal disease. The epidemiology of invasive meningococcal disease in EU/EEA countries, 2004-2014. Vaccine. 2017;35(16):2034–2041. | ||
Anonychuk A, Woo G, Vyse A, Demarteau N, Tricco AC. The cost and public health burden of invasive meningococcal disease outbreaks: a systematic review. Pharmacoeconomics. 2013;31(7):563–576. | ||
Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 Suppl):30–33. | ||
Andersen JS, Olivarius NF, Krasnik A. The Danish National Health Service Register. Scand J Public Health. 2011;39(7 Suppl):34–37. | ||
Kildemoes HW, Sørensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39(7 Suppl):38–41. | ||
Statistics Denmark [webpage on the Internet]. Statistikbanken, Table LONS20, Arbejdsfunktion 5322. Available from: http://www.statistik-banken.dk/LONS20. Accessed September 26, 2017. | ||
Statistics Denmark [webpage on the Internet]. Statistikbanken, Table SAO01. Available from: http://www.statistikbanken.dk/SAO01. Accessed September 27, 2017. | ||
Statistics Denmark [webpage on the Internet]. Statistikbanken, Table AKU502. Available from: http://www.statistikbanken.dk/aku502. Accessed September 27, 2017. | ||
Danmarks Nationalbank [webpage on the Internet]. Exchange Rates. Available from: http://www.nationalbanken.dk/en/statistics/exchange_rates/Pages/default.aspx. Accessed February 1, 2018. | ||
Regions D [webpage on the Internet]. Vejledning Økonomisk; 2017. Available from: http://www.regioner.dk/aftaler-og-oekonomi/oekonomisk-vejledning/oekonomisk-vejledning-2017. Accessed September 27, 2017. | ||
Kruse M, Sørensen J, Gyrd-Hansen D. Future costs in cost-effectiveness analysis: an empirical assessment. Eur J Health Econ. 2012;13(1):63–70. | ||
Wright C, Wordsworth R, Glennie L. Counting the cost of meningococcal disease: scenarios of severe meningitis and septicemia. Paediatr Drugs. 2013;15(1):49–58. | ||
Tirani M, Meregaglia M, Melegaro A. Health and economic outcomes of introducing the new MenB vaccine (Bexsero) into the Italian routine infant immunisation programme. PLoS One. 2015;10(4):e0123383. | ||
Wang B, Haji Ali Afzali H, Marshall H. The inpatient costs and hospital service use associated with invasive meningococcal disease in South Australian children. Vaccine. 2014;32(37):4791–4798. | ||
Davis KL, Misurski D, Miller JM, Bell TJ, Bapat B. Cost of acute hospitalization and post-discharge follow-up care for meningococcal disease in the US. Hum Vaccin. 2011;7(1):96–101. | ||
Davis KL, Misurski D, Miller J, Karve S. Cost impact of complications in meningococcal disease: evidence from a United States managed care population. Hum Vaccin. 2011;7(4):458–465. | ||
Davis KL, Bell TJ, Miller JM, Misurski DA, Bapat B. Hospital costs, length of stay and mortality associated with childhood, adolescent and young adult meningococcal disease in the US. Appl Health Econ Health Policy. 2011;9(3):197–207. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.