Back to Journals » Clinical Ophthalmology » Volume 14
Short-Term Non-Infectious Outcomes After a Pars Plana Intravitreal Antibiotic-Steroid Injection of Triamcinolone, Moxifloxacin, and Vancomycin During Cataract Surgery versus a Standard Postoperative Topical Regimen
Authors Haq Z, Zhang MH , Benjamin MJ, Riaz KM
Received 31 January 2020
Accepted for publication 7 April 2020
Published 23 April 2020 Volume 2020:14 Pages 1117—1125
DOI https://doi.org/10.2147/OPTH.S247739
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Supplementary video of "Outcomes of an intraoperative IVAS injection after cataract surgery“ [ID 247739]
Views: 108973
Zeeshan Haq,1 Michael H Zhang,1 Mark J Benjamin,2 Kamran M Riaz1
1Department of Ophthalmology and Visual Science, University of Chicago, Chicago, IL, USA; 2Benjamin Eye Care Center, La Grange, IL, USA
Correspondence: Kamran M Riaz
Dean McGee Eye Institute, University of Oklahoma, 608 Stanton L. Young Blvd, Suite 313, OK 73104, Oklahoma City Tel +1 405 271-1095
Fax +1 405 271-3680
Email [email protected]
Purpose: To compare short-term non-infectious clinical outcomes after cataract surgery with an intraoperative pars plana intravitreal antibiotic-steroid (IVAS) injection of triamcinolone, moxifloxacin, and vancomycin (TMV) versus a standard postoperative topical regimen.
Patients and Methods: A retrospective comparative case series of 1058 eyes (control = 487, treatment = 571) undergoing cataract surgery were included. Endpoints included best-corrected visual acuity (BCVA), intraocular pressure (IOP), and the unplanned use of anti-inflammatory topical medication in the postoperative period. The follow-up period ranged from 1 to 6 months.
Results: A final monocular BCVA of 20/25 or better was achieved in 78.8% and 87.4% of eyes in the control and treatment groups, respectively (p = 0.001). The overall incidence of an IOP spike (Δ ≥ 10 mm Hg) was not significantly different between the two groups (0.4% versus 1.9%, p = 0.027). The rates of persistent anterior chamber inflammation (PACI), rebound anterior chamber inflammation (RACI), and cystoid macular edema (CME) in the control and treatment groups were 8.0% vs 2.6% (p < 0.001), 6.4% vs 2.6% (p = 0.003), and 3.9% vs 4.7% (p = 0.511), respectively. The use of an IVAS injection of TMV conferred an increased risk of CME (odds ratio [OR] = 3.21, 95% confidence interval [CI] = 1.42 to 7.23) but no significant effect on the risk of PACI (OR = 0.34, 95% CI = 0.10 to 1.14) or RACI (OR = 0.52, 95% CI = 0.18 to 1.54) when compared to a topical regimen.
Conclusion: An intraoperative IVAS injection after uncomplicated cataract surgery may be as safe and effective as a standard topical regimen in terms of postoperative IOP and anterior chamber inflammatory events, respectively. However, the efficacy of a TMV formulation for CME prophylaxis appears to be unsatisfactory. Future studies with prospective and randomized designs are needed to further evaluate this technique.
Keywords: dropless cataract surgery, inflammation prophylaxis, intraocular pressure spike, cystoid macular edema
Introduction
Modern phacoemulsification cataract surgery has benefited from significant innovation in techniques and technology over the last half century. Despite these advancements, strategies for infection and inflammation prophylaxis have remained largely unchanged. Beyond standard ophthalmic surgical site antisepsis measures, current guidelines recommend topical medication in the postoperative period.1,2 However, compliance with eye drop regimens in this setting can be challenging due to financial considerations, complex treatment schedules, and difficulty with self-administration.3,4 Moreover, potential complications of improper instillation range from wound disruption and infection to uncontrolled inflammation and antibiotic resistance. Furthermore, standard postoperative topical regimens incite a high volume of queries from both patients and pharmacies that can result in significant temporal overhead.5
An alternative approach for anterior chamber drug delivery is the use of an intraoperative bolus intracameral (IC) injection. The strongest evidence in support of this technique comes from the landmark ESCRS prospective multicenter randomized controlled trial that revealed a 5-fold increase in the risk of endophthalmitis in the absence of IC cefuroxime.6 Enthusiasm for IC infection prophylaxis has continued to rise with favorable results from multiple large retrospective cohort studies and case series and increased adoption among surgeons.7–12 In addition, while the use of an IC injection of corticosteroids for control of inflammation is far less studied, early results with triamcinolone and dexamethasone are promising.13–16
In this setting, the concept of intravitreal delivery of antibiotics and steroids has emerged. This strategy involves the use of an intravitreal antibiotic-steroid (IVAS) combination medication injected by a transzonular or pars plana technique at the conclusion of cataract surgery. Antibiotics and corticosteroids are delivered directly into the vitreous cavity, where drug activity may be critical and is not limited by rapid aqueous turnover.17 To date, initial outcomes after transzonular IVAS injection have demonstrated no cases of endophthalmitis and rates of anterior segment breakthrough inflammation and cystoid macular edema (CME) comparable to prophylaxis with a topical approach.5,18 However, results after a pars plana technique for IVAS with a direct comparison against the current standard-of-care approach for postoperative inflammation prophylaxis in a large cohort have not been described.
Herein, we compare short-term non-infectious clinical outcomes after cataract surgery between eyes that received an intraoperative pars plana IVAS injection and eyes that received a standard postoperative topical regimen in a retrospective comparative case series.
Patients and Methods
A retrospective chart review of consecutive eyes that had uncomplicated cataract surgery with either a standard postoperative topical regimen (control group) or an intraoperative IVAS injection (treatment group) between November 2014 and December 2017 at the Benjamin Eye Care Center (La Grange, IL, USA) or the University of Chicago (Chicago, IL, USA) was performed. Each patient chose the postoperative prophylaxis strategy for their cataract surgery after the procedural steps, benefits, and risks of both approaches were discussed with them. Exclusion criteria for this study included: use of systemic corticosteroids at the time of cataract surgery, performance of an additional procedure other than trabecular microbypass stent (TMS, iStent®, Glaukos Corporation, San Clemente, CA, USA) placement at the time of cataract surgery, and occurrence of a significant intraoperative (posterior capsular tear, large descemet membrane detachment etc.) or postoperative (retained lens fragment etc.) surgical complication. Any control group eyes that received an extended course (6 to 8 weeks) of topical anti-inflammatory drops on a predetermined basis in the postoperative period were excluded. Any treatment group eyes that received topical anti-inflammatory drops on a predetermined basis in the postoperative period were excluded. The Institutional Review Board at the University of Chicago approved this study and waived the requirement for informed consent. This work adhered to the tenets of the Declaration of Helsinki. Patient data confidentiality was maintained throughout the study process.
All operations were performed by an experienced anterior segment surgeon (MJB or KMR) using standard surgical protocols for modern phacoemulsification surgery under topical anesthesia with intravenous sedation. Patients underwent preoperative antisepsis with 5% povidone iodine solution applied to the ocular surface and eye lids for approximately 3 minutes followed by irrigation with balanced salt solution (BSS). A 2.4 mm temporal clear corneal incision was made in all cases. This was followed by cataract removal and intraocular lens placement with slight variations in preferred technique between both surgeons. In cases of femtosecond laser-assisted cataract surgery (FLACS), a LenSx® Laser System (Alcon, Fort Worth, TX, USA) was used to perform the capsulorrhexis, nucleus softening, and, if appropriate, corneal arcuate incisions for the correction of astigmatism. In addition, the femtosecond laser was used to create the main and accessory corneal wounds by one surgeon (MJB). The surgical portion of the case was completed with hydration of all wounds using BSS to ensure watertight closure, after which additional topical anesthetic was applied to the ocular surface.
Both surgeons employed the same technique for IVAS injection for patients in the treatment group. At the conclusion of the case, a 0.12 mm forceps was used to grasp the superior limbus and a caliper, set at 3.5 mm, was used to mark the conjunctiva posteriorly from the inferotemporal limbus to designate an injection site for a pars plana approach (see Video 1; a short intraoperative video clip that demonstrates a pars plana intravitreal antibiotic-steroid injection). Approximately 0.15 mL of Trimoxivanc® (TMV; 15 mg/mL triamcinolone, 1 mg/mL moxifloxacin, and 10 mg/mL vancomycin; Imprimis Pharmaceuticals, Inc., San Diego, CA, USA) was injected into the vitreous cavity with direct visualization of medication entry. This was followed by assessment of gross intraocular pressure (IOP) by digital palpation of the cornea and assurance of watertight wound closure using cellulose sponges.
All patients were subsequently evaluated in clinic by the operating surgeon on the first day (POD1), first week (POW1), first month (POM1), third month (POM3; if available), and sixth month (POM6; if available) postoperatively.
Patients in the control group received a topical antibiotic drop (either moxifloxacin or trimethoprim/polymyxin B) to be used four times daily for the first week, a topical steroid drop (prednisolone acetate 1%) to be used four times daily and tapered over four weeks, and a topical non-steroidal drop (ketorolac) to be used three times daily for four weeks.
Electronic medical records of all patients were manually reviewed to extract information. Collected data included demography, past ocular history, relevant systemic comorbidities, use of FLACS or placement of a TMS during surgery, and the following information from each postoperative clinic visit: monocular best-corrected visual acuity (BCVA), IOP, presence of anterior chamber inflammation (eg cell, flare) using the Standardization of Uveitis Nomenclature grading schemes,19 complications, and use of topical medications. In addition, the occurrence of iatrogenic “floaters” (POD1) and final postoperative refraction and associated monocular BCVA were obtained.
Postoperative inflammatory events of interest included anterior segment breakthrough inflammation (persistent anterior chamber inflammation [PACI] or rebound anterior chamber inflammation [RACI]) and CME. PACI was defined as 2+ cell and/or flare at the POW1 visit. In contrast, RACI was defined as 1+ cell and/or flare or less at the POW1 visit with subsequent 2+ cell and/or flare detected at any visit thereafter up to, and including, the POM1 visit. All cases of clinically suspected CME, based upon symptoms or signs on indirect ophthalmoscopy, were verified by optical coherence tomography imaging of the macula through subjective interpretation (presence of cysts etc.) or an objective measurement of retinal thickness ≥ 300 microns.
Both descriptive and inferential statistics were performed with the use of Stata version 15.0 (StataCorp LP, College Station, TX). Summative results of continuous and categorical variables are presented as means (± standard deviation [SD]) and percentages, respectively, unless otherwise stated. Visual acuity values are reported in logMAR format.20 A Student’s t-test was used to compare continuous outcomes. A chi-square test (> 5 events per group) or Fisher’s exact test (≤ 5 events in at least one group) was used to compare proportional event rates. A p-value of less than 0.05 was considered statistically significant; however, a Bonferroni correction was applied if appropriate. Confounding was addressed using multivariate logistic regression with postoperative inflammatory events (PACI, RACI, or CME) as the dependent variable. Previously established confounders such as age, gender, cataract grade, diabetes mellitus, epiretinal membrane, uveitis, and pars plana vitrectomy were included in all regression analyses irrespective of statistical significance;21 alternatively, other potential confounders were eliminated in a backwards fashion at the 5% significance level.
Results
In total, 1058 eyes (control group = 487, treatment group = 571) that underwent uncomplicated cataract surgery during the study period were included. Demographic information, ocular and systemic comorbidities, cataract grade, use of FLACS, and TMS placement are reported in Table 1. Statistically significant differences between the control and treatment groups were present with respect to the following variables: glaucoma suspect status, uveitis, epiretinal membrane, pars plana vitrectomy, diabetic retinopathy with or without laser treatment, hypertension, severe cataract grade, use of FLACS, and surgical site.
 |
Table 1 Case Characteristics Including Demographic Information, Ocular and Systemic Comorbidities, and Surgical Variables |
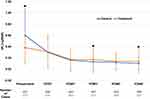
The incidence of subjective “floaters” as reported by patients on POD1 was 10.5% (51/487 cases) in the control group compared to 46.0% (262/570 cases) in the treatment group (p < 0.001). Mean monocular BCVA at the preoperative visit and each postoperative visit is summarized in Figure 1. There were statistically significant differences in the mean BCVA between the groups at the preoperative, POM1, and POM6 visits. In terms of final postoperative refraction, 78.8% (383/486 cases) and 87.4% (381/436 cases) of eyes in the control and treatment groups, respectively, had a monocular BCVA of 20/25 or better (p = 0.001).
Mean IOP at each postoperative visit is summarized in Figure 2. There was a statistically significant difference in the mean IOP between the groups at the POD1 visit; however, this difference was not present at any later visits. The overall incidence of an IOP spike (Δ ≥ 10 mm Hg) was not significantly different between the control and treatment groups (0.4% [2/487] versus 1.9% [11/571], p = 0.027). In addition, there was no statistically significant difference in the incidence of an IOP spike between the groups at any of the non-POD1 postoperative visits. Of the 11 cases of an IOP spike in the treatment group, 5 eyes had a history of either ocular hypertension or mild to moderate POAG, 2 of which had a TMS placed during their cataract surgery. Two of these eyes were treated with topical hypotensive medications, with discontinuation after 1 to 3 weeks, and all cases resolved by the next postoperative visit. No cases required surgical intervention for control of IOP.
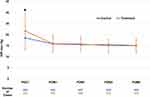 |
Figure 2 A plot of intraocular pressure (mean ± SD) versus time for each group. A star denotes a time point in which there is a statistically significant difference between the two groups. |
Outcomes regarding the unplanned use of anti-inflammatory drops in the postoperative period are reported in Table 2. The overall incidence of unplanned anti-inflammatory drop use was significantly higher in the control group (31.8% [155/487] versus 17.0% [97/571], p < 0.001). The incidence of clinically significant corneal edema (central Descemet folds on POD1 or persistent corneal edema on POW1) and ocular discomfort (pain, foreign body sensation, or discomfort secondary to subconjunctival hemorrhage that occurred on, or prior to, POM1) was significantly different between the two groups. All such non-inflammatory indications were treated with a combination of topical corticosteroid and/or non-steroidal anti-inflammatory drug (NSAID) agents that were successfully tapered and/or discontinued within 1 to 2 weeks. In terms of inflammatory events, the incidence of PACI and RACI were significantly lower in the treatment group; however, these findings were no longer significant after controlling for potential confounders. All cases of PACI and RACI were successfully treated with a topical anti-inflammatory regimen consisting of corticosteroid and/or NSAID agents for up to 4 weeks. The incidence of CME was significantly higher in the treatment group in both uncontrolled and controlled analyses. However, a significantly higher proportion of cases of CME in the control group (11/19 [57.9%] versus 0/27 [0.0%], p < 0.001) required one or more intravitreal injection(s) of steroids to achieve resolution.
 |
Table 2 Outcomes, Uncontrolled, and Controlled Analysis of the Unplanned Use of Anti-Inflammatory Drops in the Postoperative Period |
In the treatment group, a single intraoperative IVAS injection was administered in all cases with no major intraoperative complications including anterior or posterior capsule compromise. No cases of toxic anterior segment syndrome (TASS), hemorrhagic occlusive retinal vasculitis (HORV), or endophthalmitis were detected in the postoperative period. Asymptomatic retinal tears were detected in three control group and one treatment group patient(s) in the postoperative period (p = 0.339). Laser retinopexy was performed in all cases with no further complications noted.
Discussion
Use of an IVAS injection has the potential to improve the cataract surgery experience for both the patient and the provider. A randomized contralateral eye study that compared a transzonular IVAS injection versus topical pharmacotherapy found that patients preferred the former approach.22 In our study, the injection obviated the need for postoperative topical medication in the vast majority of cases. In addition, similar results have been demonstrated in previous studies that reported outcomes after an IVAS approach with a single-use compounded agent.5,18
The incidence of visually significant floaters on POD1 due to the injection is not insignificant and may be higher than reported since patients were not routinely queried about this symptom in a standardized fashion. Education regarding this expected visual disturbance should be provided preoperatively. Nonetheless, both groups achieved satisfactory rates (75% or higher) of a final monocular BCVA of 20/25 or greater during their final postoperative refraction. While the treatment group did demonstrate a significantly higher rate in this regard, this finding is likely explained by the vision-limiting comorbidity profile of the control group. In addition, the observed differences in the BCVA at POM1 and POM6 are likely due to the rate of loss to follow-up in the treatment group, many of whom had an uneventful recovery during our postoperative exams and returned to their referring optometrist for care after the immediate postoperative period.
From a procedural standpoint, we believe that adoption of a pars plana IVAS injection is not characterized by a steep learning curve. Most ophthalmologists, especially those who received training during residency to perform intravitreal injections, are familiar and comfortable with this technique from its application and established safety profile in a variety of posterior segment pathologies. Nonetheless, the risk of a retinal tear or detachment can be higher after cataract surgery or an intravitreal injection, and, as such, this risk may be compounded when both interventions are performed simultaneously. In this study, asymptomatic retinal tears were a rare occurrence (3 in the control group and 1 in the treatment group) and there was no statistically significant difference in the incidence of this complication between the two groups. However, we cannot be certain that the single retinal tear in the treatment group was not related to the injection. In addition, the true incidence of asymptomatic retinal tears may be underestimated since dilated fundus examinations were not routinely performed at all postoperative visits. Furthermore, our study is limited to a six-month follow-up period whereas retinal tears and detachments can occur well beyond this time frame.
In concordance with results from prior work, IOP spikes were rare and resolved with no intervention or a short course of topical hypotensive medication.5,18 A recent study evaluated the safety of a pars plana IVAS injection compared to a standard postoperative topical regimen in patients with POAG who underwent cataract surgery with TMS placement.23 This study found that the postoperative reduction in IOP and incidence of IOP spikes (Δ ≥ 15 mm Hg from baseline) were similar between the two groups. Taken together with our results, these findings suggest that an IVAS injection may potentially be given in patients with a history of ocular hypertension or mild to moderate POAG without a high risk for a significant elevation in IOP. However, we did not perform an IVAS injection in patients with severe POAG due to concerns related to persistent IOP elevation from triamcinolone. Ultimately, we recommend that surgeons should exercise significant caution and best judgement in determining which patients with POAG may be suitable for an IVAS injection approach.
Of cases that required supplementary topical corticosteroid and/or NSAID medication in the postoperative period, a minority were indicated due to predominantly non-inflammatory etiologies. Corneal edema requiring additional pharmacologic treatment in the immediate postoperative setting was much more common in the control group. This observation can be explained by the higher number of severe cataracts (≥ grade 4+) in this group, which likely required more intraoperative ultrasonic phacoemulsification power. The incidence of significant symptoms related to ocular discomfort was low: 0% and 2.5% in the control and treatment groups, respectively. The significantly higher rate in the treatment group may be due to subconjunctival hemorrhage at the injection site and the lack of an NSAID in the TMV formulation. In addition, it is possible that ocular discomfort was experienced by some patients in the control group; however, these symptoms were likely of mild severity and augmentation of the patient’s existing topical regimen was not deemed necessary. The incidence of PACI or RACI was significantly lower in the treatment group compared to the control group. However, the use of an IVAS injection did not confer a statistically significant protective effect when compared to a topical approach with controlled analysis. Compared to a prior report of 1541 cases that received an intraoperative transzonular IVAS injection,18 we found a lower rate of anterior segment breakthrough inflammation in our treatment group. This finding is likely due to the requirement for satisfaction of relatively objective evidence of inflammation (ie cell and/or flare criteria) in all such cases in our study.
The rate of CME was comparable in both groups. However, the use of an IVAS injection conferred a significantly higher risk of CME when compared with a topical approach with controlled analysis. We suspect that this finding may be explained, in part, by the lack of an NSAID component in the TMV formulation. Results from multiple non-dropless cataract surgery studies have demonstrated improvement in CME rates with the use of topical NSAID prophylaxis, particularly in patients with preoperative risk factors.24,25 In addition, the dose of triamcinolone used in this study was 2.25 mg, which is significantly lower than the 4 mg amount that is typically injected into the vitreous cavity of eyes with refractory pseudophakic CME. Ultimately, it is difficult to draw definitive conclusions on the true rates of CME in our study since OCT testing of the macula was not routinely performed in all patients; as such, subclinical CME that is detectable on OCT imaging may have been higher in both groups. Future iterations of this work should employ OCT imaging in all study patients at multiple time points.
There were no cases of major infectious complications, including endophthalmitis, in the studied cohort. This result was not unexpected given our short-term follow-up period, relatively small sample size, and the estimated rate of endophthalmitis in the setting of cataract surgery with or without an IVAS injection.5 Of note, the intraocular use of vancomycin has recently been linked with the development of a rare potentially blinding delayed immune reaction known as HORV.26 This association is the subject of significant debate and is under active investigation by both the American Society of Cataract and Refractive Surgery (ASCRS) and American Society of Retina Specialists (ASRS) through a joint task force and registry. Nonetheless, given the broad-spectrum coverage provided by moxifloxacin, we elected to transition to a non-vancomycin formulation, triamcinolone-moxifloxacin (TriMoxi; Imprimis Pharmaceuticals, Inc., San Diego, CA, USA), since the publication of the ASCRS-ASRS report. While vancomycin provides more effective gram-positive coverage, we share the concerns of the joint task force.
Unique safety concerns exist regarding the use of a compounded agent such as TMV. Multiple clusters of various complications including TASS,27 transient acute macular edema,28 endophthalmitis,29,30 and permanent severe vision loss,31 associated with compounded medication use have been published. However, there are no published reports to date of similar significant adverse events due to a TMV injection from the manufacturer that was used in this study.
As a result of its retrospective design, this study is notably limited by potential selection bias. The control and treatment groups differed significantly with respect to multiple characteristics, some of which are known to play a role in the incidence of postoperative inflammatory events. In particular, the control group had a higher proportion of patients with a severe cataract grade, diabetes mellitus, and other pro-inflammatory risk factors. However, regression analysis was used to address these issues to the best of our ability. Nonetheless, we cannot eliminate the possibility that residual confounding affected our results. Moreover, data regarding iris color and phacoemulsification parameters were not recorded and, as such, were unable to be collected and included in our analyses. In addition, the external validity of our results is limited due to the exclusion of patients who underwent complex cataract surgery.
Conclusion
In summary, an intraoperative IVAS injection after uncomplicated cataract surgery may be as safe and effective as a standard topical regimen in terms of postoperative IOP and anterior chamber inflammatory events, respectively. However, the efficacy of a TMV formulation for CME prophylaxis appears to be unsatisfactory. As such, continued refinement of this technique through ongoing research is critical to optimize clinical outcomes prior to consideration of widespread adoption of this approach. Future studies with a superior design, such as a prospective randomized controlled trial, are needed to more effectively evaluate this technique.
Acknowledgments
The authors would like to thank Ayushi Chandramani, MD, for her assistance with data collection and Kai Ding, PhD, for his assistance with statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Olson RJ, Braga-Mele R, Chen SH, et al. Cataract in the adult eye preferred practice pattern(R). Ophthalmology. 2017;124(2):P1–P119. doi:10.1016/j.ophtha.2016.09.027
2. Packer M, Chang DF, Dewey SH, et al. Prevention, diagnosis, and management of acute postoperative bacterial endophthalmitis. J Cataract Refract Surg. 2011;37(9):1699–1714. doi:10.1016/j.jcrs.2011.06.018
3. Newman-Casey PA, Robin AL, Blachley T, et al. The most common barriers to glaucoma medication adherence: a cross-sectional survey. Ophthalmology. 2015;122(7):1308–1316. doi:10.1016/j.ophtha.2015.03.026
4. An JA, Kasner O, Samek DA, Levesque V. Evaluation of eyedrop administration by inexperienced patients after cataract surgery. J Cataract Refract Surg. 2014;40(11):1857–1861. doi:10.1016/j.jcrs.2014.02.037
5. Lindstrom RL, Galloway MS, Grzybowski A, Liegner JT. Dropless cataract surgery: an overview. Curr Pharm Des. 2017;23(4):558–564. doi:10.2174/1381612822666161129150628
6. Endophthalmitis Study Group ESoC, Refractive S. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007;33(6):978–988. doi:10.1016/j.jcrs.2007.02.032
7. Shorstein NH, Winthrop KL, Herrinton LJ. Decreased postoperative endophthalmitis rate after institution of intracameral antibiotics in a Northern California eye department. J Cataract Refract Surg. 2013;39(1):8–14. doi:10.1016/j.jcrs.2012.07.031
8. Herrinton LJ, Shorstein NH, Paschal JF, et al. Comparative effectiveness of antibiotic prophylaxis in cataract surgery. Ophthalmology. 2016;123(2):287–294. doi:10.1016/j.ophtha.2015.08.039
9. Jabbarvand M, Hashemian H, Khodaparast M, et al. Endophthalmitis occurring after cataract surgery: outcomes of more than 480 000 cataract surgeries, epidemiologic features, and risk factors. Ophthalmology. 2016;123(2):295–301. doi:10.1016/j.ophtha.2015.08.023
10. Haripriya A, Chang DF, Namburar S, et al. Efficacy of intracameral moxifloxacin endophthalmitis prophylaxis at aravind eye hospital. Ophthalmology. 2016;123(2):302–308. doi:10.1016/j.ophtha.2015.09.037
11. Haripriya A, Chang DF, Ravindran RD. Endophthalmitis reduction with intracameral moxifloxacin prophylaxis: analysis of 600 000 surgeries. Ophthalmology. 2017;124(6):768–775. doi:10.1016/j.ophtha.2017.01.026
12. Chang DF, Braga-Mele R, Henderson BA, et al. Antibiotic prophylaxis of postoperative endophthalmitis after cataract surgery: results of the 2014 ASCRS member survey. J Cataract Refract Surg. 2015;41(6):1300–1305. doi:10.1016/j.jcrs.2015.01.014
13. Gills JP, Gills P. Effect of intracameral triamcinolone to control inflammation following cataract surgery. J Cataract Refract Surg. 2005;31(8):1670–1671. doi:10.1016/j.jcrs.2005.07.023
14. Karalezli A, Borazan M, Akova YA. Intracameral triamcinolone acetonide to control postoperative inflammation following cataract surgery with phacoemulsification. Acta Ophthalmol. 2008;86(2):183–187. doi:10.1111/j.1600-0420.2007.01114.x
15. Simaroj P, Sinsawad P, Lekhanont K. Effects of intracameral triamcinolone and gentamicin injections following cataract surgery. J Med Assoc Thai. 2011;94(7):819–825.
16. Chang DT, Herceg MC, Bilonick RA, et al. Intracameral dexamethasone reduces inflammation on the first postoperative day after cataract surgery in eyes with and without glaucoma. Clin Ophthalmol. 2009;3:345–355. doi:10.2147/OPTH.S5730
17. Meredith TA. Antimicrobial pharmacokinetics in endophthalmitis treatment: studies of ceftazidime. Trans Am Ophthalmol Soc. 1993;91:653–699.
18. Tyson SL, Bailey R, Roman JS, et al. Clinical outcomes after injection of a compounded pharmaceutical for prophylaxis after cataract surgery: a large-scale review. Curr Opin Ophthalmol. 2016.
19. Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of Uveitis Nomenclature Working G. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005;140(3):509–516.
20. Holladay JT. Visual acuity measurements. J Cataract Refract Surg. 2004;30(2):287–290. doi:10.1016/j.jcrs.2004.01.014
21. Chu CJ, Johnston RL, Buscombe C, et al. Risk factors and incidence of macular edema after cataract surgery: a database study of 81984 eyes. Ophthalmology. 2016;123(2):316–323. doi:10.1016/j.ophtha.2015.10.001
22. Fisher BL, Potvin R. Transzonular vitreous injection vs a single drop compounded topical pharmaceutical regimen after cataract surgery. Clin Ophthalmol. 2016;10:1297–1303. doi:10.2147/OPTH.S112080
23. Kindle T, Ferguson T, Ibach M, et al. Safety and efficacy of intravitreal injection of steroid and antibiotics in the setting of cataract surgery and trabecular microbypass stent. J Cataract Refract Surg. 2018;44(1):56–62. doi:10.1016/j.jcrs.2017.10.040
24. McCafferty S, Harris A, Kew C, et al. Pseudophakic cystoid macular edema prevention and risk factors; prospective study with adjunctive once daily topical nepafenac 0.3% versus placebo. BMC Ophthalmol. 2017;17(1):16. doi:10.1186/s12886-017-0405-7
25. Shorstein NH, Liu L, Waxman MD, Herrinton LJ. Comparative effectiveness of three prophylactic strategies to prevent clinical macular edema after phacoemulsification surgery. Ophthalmology. 2015;122(12):2450–2456. doi:10.1016/j.ophtha.2015.08.024
26. Witkin AJ, Shah AR, Engstrom RE, et al. Postoperative hemorrhagic occlusive retinal vasculitis: expanding the clinical spectrum and possible association with vancomycin. Ophthalmology. 2015;122(7):1438–1451. doi:10.1016/j.ophtha.2015.03.016
27. Cakir B, Celik E, Aksoy NO, et al. Toxic anterior segment syndrome after uncomplicated cataract surgery possibly associated with intracamaral use of cefuroxime. Clin Ophthalmol. 2015;9:493–497. doi:10.2147/OPTH.S74249
28. Wong DC, Waxman MD, Herrinton LJ, Shorstein NH. Transient macular edema after intracameral injection of a moderately elevated dose of cefuroxime during phacoemulsification surgery. JAMA Ophthalmol. 2015;133(10):1194–1197. doi:10.1001/jamaophthalmol.2015.2421
29. Goldberg RA, Flynn HW
30. Cakir M, Imamoglu S, Cekic O, et al. An outbreak of early-onset endophthalmitis caused by Fusarium species following cataract surgery. Curr Eye Res. 2009;34(11):988–995. doi:10.3109/02713680903254822
31. Olavi P. Ocular toxicity in cataract surgery because of inaccurate preparation and erroneous use of 50mg/mL intracameral cefuroxime. Acta Ophthalmol. 2012;90(2):e153–4. doi:10.1111/j.1755-3768.2010.02103.x
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.