Back to Journals » International Medical Case Reports Journal » Volume 9
Serum total IgG and IgG4 levels in thyroid eye disease
Authors Sy A, Silkiss RZ
Received 3 July 2016
Accepted for publication 22 August 2016
Published 20 October 2016 Volume 2016:9 Pages 325—328
DOI https://doi.org/10.2147/IMCRJ.S116331
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Aileen Sy, Rona Z Silkiss
Department of Ophthalmology, California Pacific Medical Center, San Francisco, CA, USA
Purpose: To investigate the relationship between immunoglobulin G (IgG)4-related disease (IgG4-RD) and thyroid eye disease (TED) with respect to IgG levels.
Patients and methods: A retrospective review of total IgG, IgG subclass, and thyroid stimulating immunoglobulin (TSI) levels in 24 patients with TED.
Results: Five patients (20.8%) demonstrated serum IgG4 levels consistent with IgG4-RD without any additional systemic disease. Total IgG and IgG subclass levels were found to be an inadequate proxy for TSI elevation.
Conclusion: There may be a subtype of TED patients with elevated IgG4 in the absence of IgG4-RD systemic findings.
Keywords: thyroid eye disease, IgG subclass, IgG4, Graves’ disease, Graves’ ophthalmopathy, IgG4-RD
Introduction
Immunoglobulin G (IgG)4-related disease (IgG4-RD) is a relatively recently described systemic, fibro-inflammatory disorder that affects multiple organ systems, including commonly the orbits.1 Reports have identified IgG4-RD as an etiology of previously described cases of orbital inflammatory disease or pseudotumor.1–3 The most common orbital inflammatory disease is thyroid eye disease (TED). Studies of elevated serum IgG4 levels in systemic Graves’ disease and histopathologic analysis of thyroid stroma from Graves’ disease patients have suggested a possible subpopulation of Graves’ patients with elevated IgG4.4,5 However, the study of IgG4 levels in the TED subgroup has not been previously reported nor have IgG subclass levels been evaluated in TED at large. The authors sought to evaluate total IgG and IgG subclass levels, including IgG4, in a TED population to determine if a subset of this population demonstrated latent IgG4-RD. Additionally, the relationship among total IgG, IgG4, and thyroid stimulating immunoglobulin (TSI) levels was investigated.
Methods
TED patients in the practice of one author (RZS) between December 2013 and January 2015 were reviewed. Patients with total and IgG subclass and thyroid function tests were included in the study. None of the patients studied demonstrated systemic signs or symptoms of IgG4-RD. Those patients meeting the serum criteria for IgG4-RD by either serum IgG4 concentration ≥135 mg/dL (Umehara et al.) or ratio of IgG4/IgG ≥8% (Masaki et al.) criteria were identified.6,7 No biopsies for histopathological review were evaluated. The authors present in brief five case reports of patients with TED who also met serum criteria for IgG4-RD, followed by a summary of total IgG, IgG subclass, and TSI levels.
Institutional review board (IRB) approval was obtained from the Sutter Health IRB for this retrospective review that waived the need for individual informed consent. The study adhered to the Declaration of Helsinki and the Health and Portability and Accountability Act regulations.
Results
A total of 24 patients with available subclass IgG levels and thyroid function tests were identified. Twenty of these patients had total IgG levels available. Of 24 patients, two (8.3%) were found to meet IgG4-RD criteria by serum level ≥135 mg/dL and three (12.5%) by IgG4/IgG ratio ≥8%.
Case 1
A 55-year-old woman presented with an insidious onset of left ocular proptosis of uncertain duration. She did not have any other systemic issues or medical diagnoses. Her visual acuity was 20/20 in both eyes. Examination demonstrated eyelid retraction with proptosis of the left eye (clinical activity score (CAS) 3). Magnetic resonance imaging (MRI) showed enhanced, thickened extraocular muscles, particularly the inferior and superior recti. Her TSI was 753%, total IgG 1,496 mg/dL, and IgG4 167 mg/dL with an IgG4/IgG ratio of 11.1%.
Case 2
A 39-year-old man presented with a 6-week history of proptosis and diplopia. He had no other systemic symptoms. Medical history was remarkable for the diagnosis of hyperthyroidism 1 year prior, for which he was taking methimazole. Visual acuity was 20/30 right eye and 20/20 left eye. Examination was significant for left upper lid retraction, and proptosis and chemosis in both eyes (CAS 4). MRI showed bilateral inferior and medial rectus muscle enlargement. TSI was 353%, total IgG 1,202 mg/dL, and IgG4 106.3 mg/dL with IgG4/IgG ratio of 8.8%.
Case 3
A 53-year-old woman presented with an insidious onset of diplopia and headaches. She had been recently diagnosed with hyperthyroidism and started on methimazole. Her medical history was notable for hypertension. She was otherwise symptomatically well. Her vision was 20/30 in the right eye and 20/25 in the left eye, with examination demonstrating left upper lid retraction, restriction of left supraduction, and left proptosis (CAS 5). MRI showed enhancement of the inferior and lateral left extraocular muscles. Her TSI was 323%, total IgG 1,294 mg/dL, IgG4 123 mg/dL, and IgG4/IgG ratio was 9.5%.
Case 4
A 57-year-old woman presented with a 3-month history of bilateral proptosis and diplopia. She reported systemic symptoms of fatigue, weight gain, and dry skin consistent with hypothyroidism. Her history was significant for a thyroidectomy 20 years prior. She was being treated with levothyroxine. Her medical history was otherwise unremarkable. Visual acuity was 20/25 in both eyes and exam was significant for eyelid retraction and proptosis of both eyes (CAS 3). Her TSI was 354%, total IgG 987 mg/dL, and IgG4 97 mg/dL with an IgG4/IgG ratio of 9.8%. No MRI was available at the time of review.
Case 5
A 32-year-old woman presented with bilateral upper lid retraction and a prior diagnosis of hyperthyroidism treated with methimazole. She did not have any other systemic issues or medical diagnoses. Her visual acuity was 20/20 in both eyes and exam showed lid retraction of both eyelids (CAS 2). TSI was 539%, total IgG 1,335 mg/dL, and IgG4 153 mg/dL with IgG4/IgG ratio of 11.5%. An MRI was not available at the time of review.
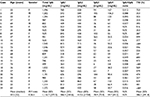
Serum total IgG, IgG subclass, and TSI in TED patients
Data for total IgG, IgG subclass, and TSI are detailed in Table 1. Summary data were performed in STATA. There were 19 women and five men (M:F ratio 0.26:1), and the average age was 50.2 years (median age of 52 years, range 32 to 74 years). Serum total IgG in TED patients was 1,116.7±277.0 mg/dL (range 499–1,546), IgG1 subclass 586.4±184.6 mg/dL (range 318–974), IgG2 subclass 410.6±170.8 mg/dL (range 102–863), and IgG3 subclass 78.9±70.0 mg/dL (range 6–362). Serum IgG4 subclass was 59.7±44.2 mg/dL (range 3.8–167) and TSI 386.2±191.8% (range 24–753). All total IgG levels were within normal range, regardless of TSI elevation, and no particular IgG subclass correlated with TSI elevation. Additionally, there was no correlation found between CAS and total IgG or IgG4 subclass levels.
Discussion
The results of this study identify a small subset of TED patients with elevated serum IgG4 levels meeting serum IgG4-RD criteria but without findings of systemic IgG4-RD by symptomology and medical history. This study also reveals that total IgG levels were not an adequate proxy for either IgG4 or TSI elevation. Among TED patients, there did not appear to be a dominance of any one subclass of IgG, nor were high levels of TSI associated with elevation in total IgG or a specific IgG subclass.
Patients included in the study had clinical exam findings, imaging, and/or lab values consistent with TED but did not have other systemic symptoms or medical issues to indicate multi-system organ involvement characteristic of IgG4-RD. A case of concurrent IgG4-RD and TED has been described in the literature, but how commonly IgG4-RD or IgG4 elevation occurs in TED patients has not been reported.8 Serum IgG4 levels in Graves’ thyroidopathy patients with systemic manifestations have been reported. In 1990, before the first descriptions of IgG4-RD, Weetman et al. investigated the levels of each IgG subtype in 10 Graves’ disease patients and found two patients with IgG4 levels greater than the 95th percentile of normal; however, only one of these patients had an IgG4 level ≥135 mg/dL.9 In 2014, Takeshima et al. studied 109 Graves’ thyroidopathy patients and found seven (6.4%) had elevated serum IgG4 levels ≥135 mg/dL and three (2.8%) additional cases had IgG4/IgG ratios ≥8%.4 These patients were found to be older, with more hypoechoic areas on thyroid ultrasound. Three patients with elevated IgG4 levels also had CAS suggestive of ocular involvement (2.8%); however, there was no statistical difference in the incidence of ophthalmopathy by CAS or orbital imaging between the non-elevated and elevated IgG4 groups. Histopathologic study of stromal thyroid tissue from Graves’ disease patients found 0.74% (11/1484) to have diffuse lymphoplasmacytic infiltration characteristic of IgG4-RD.5 Of these 11 cases, the investigators found only a portion had IgG4-positive plasma cells (45.5%; 0.33% overall).5 Further investigation into patients with ophthalmopathy was not available. In our current study specific to Graves’ ophthalmopathy patients, our results suggest a higher (8.3% by IgG4 level ≥135 mg/dL criteria or 20.8% by combined criteria) prevalence of serum IgG4 elevation among TED patients. In another study, orbital biopsies of patients with varying orbital diseases were studied for immunostaining with IgG4. None of the biopsies from TED patients had significant IgG4 staining.3 Biopsies for histopathological analysis were not available for our study.
Conclusion
The identification of a possible subgroup of TED patients with elevated IgG4 may aid in the further development of a treatment protocol for TED. While the use of IgG levels may not be an adequate proxy for TSI or TED, IgG4 levels may help to identify patients selectively more responsive to rituximab or other biologics, allowing for earlier and more effective treatment. It remains unclear whether the presence of IgG4 elevation in this subpopulation of TED patients indicates a more severe inflammatory disease course or predates latent IgG4-RD. Further immunologic evaluation of TED patients could provide insight into the pathogenesis of the disease and aid in the selection of biologic immune therapy.
Acknowledgment
The authors thank the Pacific Vision Foundation for their support of this research.
The abstract of this paper was presented at the ARVO Annual Meeting, May 3–7 2015 in Denver, CO, USA.
Disclosure
The authors report no conflicts of interest in this work.
References
McNab AA, McKelvie P. IgG4-related ophthalmic disease. Part I: background and pathology. Ophthal Plast Reconstr Surg. 2015;31(2):83–88. | ||
Andrew NH, Sladden N, Kearney DJ, Selva D. An analysis of IgG4-related disease (IgG4-RD) among idiopathic orbital inflammations and benign lymphoid hyperplasias using two consensus-based diagnostic criteria for IgG4-RD. Br J Ophthalmol. 2015;99(3):376–381. | ||
Wong AJ, Planck SR, Choi D, et al. IgG4 immunostaining and its implications in orbital inflammatory disease. PLoS One. 2014;9(10):e109847. | ||
Takeshima K, Inaba H, Furukawa Y, et al. Elevated serum immunoglobulin G4 levels in patients with Graves’ disease and their clinical implications. Thyroid. 2014;24(4):736–743. | ||
Nishihara E, Hirokawa M, Ito M, Fukata S, Nakamura H, Amino N, Miyauchi A. Graves’ disease patients with persistent hyperthyroidism and diffuse lymphoplasmacytic infiltration in the thyroid show no histopathological compatibility with IgG4-related disease. PLoS One. 2015;10(7):e0134143. | ||
Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol. 2012;22(1):21–30. | ||
Masaki Y, Kurose N, Yamamoto M, et al. Cutoff values of serum IgG4 and histopathological IgG4+ plasma cells for diagnosis of patients with IgG4-related disease. Int J Rheumatol. 2012;2012:580814. | ||
Kubota T, Moritani S, Terasaki H. Ocular adnexal IgG4-related lymphoplasmacytic infiltrative disorder and Graves ophthalmopathy. Arch Ophthalmol. 2011;129(6):818–819. | ||
Weetman AP, Byfield PG, Black C, Reimer CB. IgG heavy-chain subclass restriction of thyrotropin-binding inhibitory immunoglobulins in Graves’ disease. Eur J Clin Invest. 1990;20(4):406–410. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.