Back to Journals » Clinical Ophthalmology » Volume 14
Secondary Posterior Chamber Intraocular Lens Fixation Using Flanged Prolene Sutures as an Alternative to an Anterior Chamber Intraocular Lens Implantation
Authors Hostovsky A , Mandelcorn M, Mandelcorn ED
Received 12 August 2020
Accepted for publication 28 September 2020
Published 23 October 2020 Volume 2020:14 Pages 3481—3486
DOI https://doi.org/10.2147/OPTH.S276707
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Video abstract of "Four point IOL fixation is a good alternative to ACIOL implantation" [ID 276707].
Views: 581
Avner Hostovsky,1,2 Mark Mandelcorn,1,2 Efrem D Mandelcorn1,2
1Department of Ophthalmology and Vision Sciences, University of Toronto, Toronto, Ontario, Canada; 2Department of Ophthalmology, Toronto Western Hospital, The University Health Network, Toronto, Ontario, Canada
Correspondence: Avner Hostovsky
Department of Ophthalmology and Vision Sciences, University of Toronto, Toronto, Ontario, Canada
Email [email protected]
Purpose: To describe and evaluate the clinical outcomes of the Flanged Prolene Suture intraocular lens fixation (PIF) technique and compare it to anterior chamber IOL (ACIOL) implantation.
Design: A retrospective comparative review.
Methods: A retrospective comparative review of consecutive patients undergoing secondary IOL implantation was performed. A comparison between patients that had ACIOL and PIF technique was conducted. The main outcome measures were changes in best-corrected visual acuity (VA), IOL position and complications.
Results: In the study period, fourteen eyes had ACIOL implantation and ten eyes had PIF surgery. VA acuity for both groups combined improved from 1.27 ± 0.65 logMAR preoperatively to 0.84 ± 0.65 logMAR (P< 0.0001). Seventeen patients had VA measurements in the year before the IOL dislocation. In those seventeen patients, VA changed from a baseline of 0.90 ± 0.68 to 0.97 ± 0.61 logMAR in the PIF group (p=0.334) and from 0.54 ± 0.27 to 0.85 ± 0.65 logMAR in the ACIOL group (p=0.145). No intraoperative or early postoperative complications were documented in either group. Two (20%) patients in the PIF group developed CME and one patient developed corneal edema. In the ACIOL group, one patient developed significant CME and two patients developed visual significant corneal edema.
Conclusion: The PIF technique seems to offer a simple, fast and safe way to fixate an IOL posteriorly. In our experience, the learning curve of the technique is short with a low complication rate and good visual outcomes.
Keywords: four-point, flange, IOL fixation
Introduction
There are a myriad of surgical techniques described for secondary intraocular lens (IOL) implantation in the absence of capsular support. These included anterior chamber IOL (ACIOL), iris-fixated IOL, transscleral sutured posterior chamber IOL, and Flanged Intrascleral Intraocular Lens Fixation with Double-Needle Technique (FIF).1–4
Because FIF has advantages over the other techniques with reduced rates of corneal endothelial cell loss, glaucoma, and peripheral anterior synechiae,5–7 it has become a common technique for IOL fixation.8,9 Haptic breakage during surgery, postoperative IOL dislocation, and IOL tilt remain a significant concern with this technique. In an attempt to avoid those complications, some authors have recommended using a specific three-piece IOL such as CT-Lucia (Zeiss) IOL or Aaris EC-3 PAL IOL which are not always readily available.10,11
The relatively long learning curve of performing FIF and the uncertain access to the specific lenses needed for this type of fixation may limit its use. Recent publications show that ACIOL, with its large corneal or scleral incision, is still a widely used technique for secondary IOL in 23% to 50% cases.12–14
Since November 2017, FIF has been our preferred IOL fixation technique. Anterior chamber IOLs are currently being used in our surgical practice only in cases in which a large corneal or a scleral tunnel is needed (dislocated PMMA lens, mature cataract requiring extracapsular surgery), in cases of repeat IOL dislocations, or in cases that are deemed high risk in which a short surgical duration is desired. Since January 2019, instead of ACIOL implantation, we have been using a variant of FIF in which there is no need for tissue glue or tying sutures as described by Canabrava et al.15 The purpose of this study is to describe the preliminary results of this IOL fixation technique and to compare the results and complication rates to ACIOL implantation.
Methods
This study is a retrospective comparative review of consecutive cases of secondary intraocular lens implantation following dislocated IOL or subluxated crystalline that had either ACIOL implantation before the introduction of Flanged Prolene Suture intraocular lens fixation (PIF) (November 2017 to December 2018) or PIF (January 2018 to July 2019).
All cases were performed by a single vitreoretinal surgeon (EDM) at the Toronto Western Hospital, University of Toronto.
Two groups were compared, namely, those undergoing ACIOL implantation before the introduction of PIF (November 2017 to December 2018) and those undergoing PIF (January 2018 to July 2019).
Approval of the research ethics board of the Toronto Western Hospital was obtained, and the research was conducted with the adherence to the guidelines of the Declaration of Helsinki. As this is a retrospective study and no patient identification data was collected, informed consent was not required.
Patient demographics, preoperative and postoperative data including patients’ age, sex, operative eye, best-corrected visual acuity, lens status, IOL calculation data, postoperative refractive data and complications such as cystoid macular edema, hypotony (IOP <6 mmHg), choroidal detachment, vitreous hemorrhage, and endophthalmitis were reviewed and collected. Intraoperative data obtained included surgical procedure details, number of IOL fixation attempts and intraoperative complications. All eyes with a minimum follow-up of three months were included in the analysis.
Technique
After removal of the dislocated IOL or crystalline lens through a 5–7mm corneal incision or scleral tunnel, a 27-gauge thin-wall TSK needle is inserted 2.5mm posterior to the limbus, at the 3-o’clock position. Similar to Baskaran et al X-NIT technique,16 the needle enters the conjunctiva and sclera in a perpendicular direction, without the creation of a beveled tunnel, and is introduced into the open corneal incision from behind the iris. A 5–0 polypropylene mono-filament (Surgipro, CV-15 taper needle) is docked into the lumen of the needle and removed from the scleral opening. The same manoeuvre is performed 180 degrees from the initial site, resulting in two 5–0 polypropylene monofilaments externalized 2.5 mm from the limbus. The Single Piece PMMA CZ70BD9® IOL is then placed upside down on the cornea to make the suture pass easier, and the two sutures are passed through the haptic eyelet and heated by thermocautery to create one flange at each islet. After each flange is tested for stability, the IOL is inverted and introduced to the eye through the corneal or scleral tunnel incision. The two polypropylene sutures are then gently pulled to centre the IOL behind the iris. Once the IOL is in good position, the sutures are cut 2 mm from their base and heated to create the third and fourth flanges, which are tucked into the scleral wound and buried under the conjunctiva (Figure 1).
Statistical Analysis
Descriptive statistics were used to report patient demographics and operative details. Comparisons between groups of best-corrected visual acuity and the incidence of postoperative complications were made between the techniques using the chi-square test. Other variables, including postoperative IOP and change in best-corrected visual acuity, were described as mean with SD and compared using the paired samples t-test. Descriptive statistics were used to report patient demographics and operative details. All statistical analyses were performed using SPSS 22.0.
Results
In the study period (November 2017 to July 2019), 139 eyes underwent surgery for dislocated IOL or subluxated crystalline lens. 103 eyes (74%) of 101 patients had FIF, 12 eyes (8%) of 12 patients had three-piece IOL implantation in the sulcus.
Of the remaining 24 eyes, 14 (10%) had ACIOL implantation (Group 1) and ten eyes (7%) of 10 patients had PIF (Group 2). These 24 cases comprise the study population.
Demographics and Indications
The mean age of subjects was 86.1 ± 7.2 years in the PIF group and 81.43 ± 9.3 years in the ACIOL group. All patients had at least three months of follow-up with an average follow-up time of 125 ± 45 days. In both groups, the most common indication for surgery was IOL exchange due to subluxated/dislocated 1-piece IOL in the bag, six eyes (60%) in the PIF group and eight eyes (57%) in the ACIOL group. Other indications included aphakia, PMMA IOL dislocation, uveitic hyphema glaucoma syndrome (UGH), ACIOL removal due to subluxation and chronic CME, dislocated flanged fixated IOL and mature cataract that was preplanned for extracapsular cataract extraction surgery. The clinical characteristics are summarized in Table 1.
 |
Table 1 Clinical Characteristics of Patients That Had ACIOL Implantation and PIF |
Outcomes
The visual acuity, for all patients, improved from a mean of 1.27 ± 0.65 logMAR preoperatively to 0.84 ± 0.65 logMAR (P<0.0001). In the PIF group, the logMAR VA improved from preoperative 1.42 ± 0.66 to postoperative 0.88 ± 0.53 (p<0.001). In the AC IOL group, the logMAR improved from preoperative 1.17 ± 0.64 to post operative 0.82 ± 0.64 (p<0.001) at last follow up (Table 2).
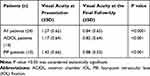 |
Table 2 Change in Visual Acuity results from Presentation to the Last Follow-Up |
Following a special effort made to obtain the visual acuity of the patients in the year before the original IOL had become dislocated, data were obtained in 17 patients, 7 patients in the PIF group and 10 patients in the ACIOL group. In this group of 17 patients, the logMAR visual acuity before the IOL dislocation was found to be 0.69 ± 0.50. It decreased to 0.90 ± 0.61 logMAR after the IOL exchange in the last follow-up (p=0.094). In the PIF group, the VA changed from a baseline of 0.90 ± 0.68 to 0.97 ± 0.61 logMAR following PIF (p=0.334). In the ACIOL group the logMAR decreased from 0.54 ± 0.27 to 0.85 ± 0.65 logMAR following ACIOL implantation (p=0.145). In other words, the visual acuity was not significantly different after the secondary IOL from the way it had been 1 year prior with the original IOL in place for each group (Table 3).
 |
Table 3 Change in Visual Acuity Results from Baseline to the Last Follow-Up |
Complications
No intraoperative complications were documented in either group. In particular, there was no case of IOP elevation, hyphema, vitreous hemorrhage, IOL tilt, or decentralization in the early postoperative period. Also, in the PIF group, there were no suture-related complications, such as exposure, scleral atrophy, discomfort, foreign body sensation or conjunctival scar formation.
In the PIF group, two (20%) patients had post-surgery cystoid macular edema (CME). The CME resolved with a single anterior subtenon’s injection of triamcinolone acetate 1% (Bristol-Myers Squibb ®) in both patients. One patient that was preplanned to DMEK surgery due to pre-existing corneal decompensation developed significant corneal edema after the PIF procedure.
In the ACIOL group, one patient developed significant CME with minimal response to steroid treatment (subtenon or intraocular), and two patients developed visual significant corneal edema.
When compared to the baseline visual acuity, one patient (12%) in the PIF group and three patients (21%) in the ACIOL group lost more than three lines of vision. The difference between groups was not statistically significant (p=0.45) (Table 4).
 |
Table 4 Intraoperative and Postoperative Complication |
Discussion
Since FIF was first described by Yamane et al in 2018,4 many surgeons have made it their preferred treatment for secondary IOL implantation. To a large extent, it has replaced iris IOL fixation and sutured scleral fixation techniques.
The open loops model of the ACIOL, first introduced almost twenty years ago,17 offers stable fixation in the angle and a relatively simple and fast surgical technique and is currently used, as a secondary IOL in 23% to 50% cases.12–14 Nevertheless, since ACIOL implantation is associated with a higher risk for producing postoperative transient corneal edema, bullous keratopathy, and uveitis and hyphema,18–20 we sought to develop a different approach for posterior IOL fixation in patients requiring a larger corneal incision that might make the risk of such complications lower.
In our study, patients in the PIF group had visual acuity outcomes and complication rates that were comparable to ACIOL implantation. No intraoperative IOL or suture-related complications were encountered. Only one patient had a visually significant complication that was caused by preexisting corneal edema. Two patients developed mild CME that responded to treatment.
Although longer followed-up is needed to assess the late-term complication rate, the advantage of the posterior location of the IOL should theoretically reduce the risk of long-term damage to corneal endothelial cell and to the risk of long-term iris irritation, persistent CME, uveitis and hyphema.
The PIF technique offers a simple and fast way to fixate an IOL posterior to the iris without the need for tissue glue, complex suturing maneuvers or scleral tunnels. In our experience, the learning curve for the technique is short with a low complication rate and good visual outcomes, especially in cases requiring a large corneal or scleral incision to deal with a dislocated PMMA IOL or a large dislocated crystalline lens that might otherwise be handled using an ACIOL.
Summary Statement
Four-point IOL fixation is a good alternative to ACIOL implantation.
Funding
No funding received for this work from any of the following organizations: National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI).
Disclosure
No conflicting relationship exists for any of the authors.
References
1. Por YM, Lavin MJ. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Surv Ophthalmol. 2005;50(5):429–462. doi:10.1016/j.survophthal.2005.06.010
2. Koh HJ, Kim CY, Lim SJ, Kwon OW. Scleral fixation technique using 2 corneal tunnels for a dislocated intraocular lens. J Cataract Refract Surg. 2000;26(10):1439–1441. doi:10.1016/s0886-3350(00)00477-6
3. Zeh WG, Price FW. Iris fixation of posterior chamber intraocular lenses. J Cataract Refract Surg. 2000;26(7):1028–1034. doi:10.1016/S0886-3350(00)00322-9
4. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136–1142. doi:10.1016/j.ophtha.2017.03.036
5. Drolsum L. Long-term follow-up of secondary flexible, open-loop, anterior chamber intraocular lenses. J Cataract Refract Surg. 2003;29(3):498–503. doi:10.1016/s0886-3350(02)01614-0
6. Evereklioglu C, Er H, Bekir NA, Borazan M, Zorlu F. Comparison of secondary implantation of flexible open-loop anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 2003;29(2):301–308. doi:10.1016/S0886-3350(02)01526-2
7. Kokame GT, Yanagihara RT, Shantha JG, Kaneko KN. Long-term outcome of pars plana vitrectomy and sutured scleral-fixated posterior chamber intraocular lens implantation or repositioning. Am J Ophthalmol. 2018;189:10–16. doi:10.1016/j.ajo.2018.01.034
8. Kelkar A, Kelkar J, Kothari A, et al. Comparison of two modified sutureless techniques of scleral fixation of intraocular lens. Ophthalmic Surg Lasers Imaging Retin. 2018;49(10):e129–e134. doi:10.3928/23258160-20181002-15
9. Czajka MP, Frajdenberg A, Stopa M, Pabin T, Johansson B, Jakobsson G. Sutureless intrascleral fixation using different three-piece posterior chamber intraocular lenses: a literature review of surgical techniques in cases of insufficient capsular support and a retrospective multicentre study. Acta Ophthalmol. 2019. doi:10.1111/aos.14307
10. Stem MS, Wa CA, Todorich B, Woodward MA, Walsh MK, Wolfe JD. 27-gauge sutureless intrascleral fixation of intraocular lenses with haptic flanging: short-term clinical outcomes and a disinsertion force study. Retina. 2018:1. doi:10.1097/IAE.0000000000002268
11. Yoshida N, Kojima T, Yokoyama S, Horai R, Ichikawa K. New surgical approach for intrascleral fixation using an intraocular lens with hook-shaped haptics. J Cataract Refract Surg. 2018;44(2):129–133. doi:10.1016/j.jcrs.2017.12.011
12. Vounotrypidis E, Schuster I, Mackert MJ, Kook D, Priglinger S, Wolf A. Secondary intraocular lens implantation: a large retrospective analysis. Graefes Arch Clin Exp Ophthalmol. 2019;257(1):125–134. doi:10.1007/s00417-018-4178-3
13. Lorente R, De Rojas V, Vazquez De Parga P, et al. Management of late spontaneous in-the-bag intraocular lens dislocation: retrospective analysis of 45 cases. J Cataract Refract Surg. 2010;36(8):1270–1282. doi:10.1016/j.jcrs.2010.01.035
14. Østern AE, Sandvik GF, Drolsum L. Late in-the-bag intraocular lens dislocation in eyes with pseudoexfoliation syndrome. Acta Ophthalmol. 2014;92(2):184–191. doi:10.1111/aos.12024
15. Canabrava S, Canêdo Domingos Lima AC, Ribeiro G. Four-flanged intrascleral intraocular lens fixation technique. Cornea. 2020;39(4):527–528. doi:10.1097/ico.0000000000002185
16. Baskaran P, Ganne P, Bhandari S, Ramakrishnan S, Venkatesh R, Gireesh P. Extraocular needle-guided haptic insertion technique of scleral fixation intraocular lens surgeries (X-NIT). Indian J Ophthalmol. 2017;65(8):747. doi:10.4103/ijo.IJO_296_17
17. Weene LE. Flexible open-loop anterior chamber intraocular lens implants. Ophthalmology. 1993;100(11):1636–1639. doi:10.1016/S0161-6420(13)31445-6
18. Chan TCY, Lam JKM, Jhanji V, Li EYM. Comparison of outcomes of primary anterior chamber versus secondary scleral-fixated intraocular lens implantation in complicated cataract surgeries. Am J Ophthalmol. 2015;159(2):221–226.e2. doi:10.1016/j.ajo.2014.10.016
19. Khan MA, Gupta OP, Pendi K, et al. Pars plana vitrectomy with anterior chamber versus gore-tex sutured posterior chamber intraocular lens placement: long-term outcomes. Retina. 2019;39(5):860–866. doi:10.1097/IAE.0000000000002042
20. Melamud A, Topilow JS, Cai L, He X. Pars plana vitrectomy combined with either secondary scleral-fixated or anterior chamber intraocular lens implantation. Am J Ophthalmol. 2016;168:177–182. doi:10.1016/j.ajo.2016.05.006
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

