Back to Journals » Research and Reports in Urology » Volume 11
Same-day angiography and embolization in delayed hematuria following percutaneous nephrolithotomy: an effective, safe, and time-saving approach
Authors Chakraborty JN , Hatimota P
Received 26 October 2018
Accepted for publication 27 January 2019
Published 21 March 2019 Volume 2019:11 Pages 83—89
DOI https://doi.org/10.2147/RRU.S192175
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Joy Narayan Chakraborty, Pradeep Hatimota
Depart of Urology and Radiology, Apollo Hospitals, Guwahati 781005, India
Purpose: To evaluate the results of prompt, same-day selective angiography and transcatheter angioembolization (TAE) on delayed post-percutaneous nephrolithotomy (PCNL) hematuria.
Materials and methods: Between 2011 and 2017, 21 patients with a mean age of 37 years (range, 21–60 years; males, 18) underwent digital subtraction angiography (DSA) and TAE to control delayed gross hematuria following PCNL. Discharged patients who following an uneventful PCNL presented to the emergency room with gross, brisk hematuria were included in the study and taken up for prompt, same-day DSA and same-session TAE with N-butyl-2-cyanoacrylate glue, without resorting to any initial conservative measures. All patient data were retrieved from medical records.
Results: Angiography revealed vascular lesions in all the cases (pseudoaneurysms, 14 cases; arteriovenous fistula, 2; mixed lesions, 5). The mean time of onset of delayed hemorrhage was 10.10±2.67 days. The average time from onset of bleeding to TAE was 4.31±0.64 hours (range 3.5–5.5 hours). Bleeding was controlled in all the cases without any recurrence or the need for further embolization. There were no procedural complications except for transient elevation of serum creatinine in four cases.
Conclusion: Primary DSA and TAE is a safe, effective, and time-saving alternative to conservative management for post-PCNL, delayed, gross hematuria.
Keywords: angiography, transcatheter angioembolization, PCNL, hematuria, delayed bleeding, percutaneous nephrostomy
Introduction
Percutaneous nephrolithotomy (PCNL) is a safe and effective surgical procedure for the management of kidney stones, especially for large volume (>2 cm in size) and complex stones. Some amount of bleeding, secondary to internal manipulation, is expected while accessing the pelvicalyceal system. This is usually related to disruption of the high-flow arteriovenous network closely surrounding the collecting system, which receives about 20% of the total cardiac output. Often, this bleeding is self-limiting and is spontaneously controlled. The incidence of major bleeding requiring transfusion following PCNL is 2%–23%.1–4 Delayed and massive bleeding usually results from traumatic arteriovenous malformations, which require transcatheter angioembolization (TAE), and constitute 0.4%–2% of all cases undergoing PCNL.5 Pseudoaneurysms (PA) are the most common cause of delayed hemorrhage, followed by arteriovenous fistulae (AVF), mixed lesions, and lumbar artery aneurysms. Interlobar and arcuate arteries are the most common offenders developing PA, followed by the posterior segmental artery.4,6–8
Cases with massive post-PCNL hematuria, whether early or delayed, warrant an early or urgent digital subtraction angiography (DSA) and TAE to control bleeding. Delayed hematuria often presents as brisk and intermittent bleeding, and is managed initially by conservative measures (close monitoring for recurrent bleeding or fall in hematocrit, imaging tests, blood transfusions). The standard indications for DSA are recurrent or continuous bleeding with a drop in corrected hemoglobin of >30 g/L or hemodynamic instability.9–11 The timing of intervention is based on clinical judgment and is subjective.
Herein, we report on the diagnosis, effectiveness, morbidity, complications, and hospitalization time with primary same-day DSA and TAE in cases with post-PCNL, delayed, and brisk gross hematuria based on our experience. A secondary analysis was performed to identify the demographic factors, stone characteristics, and primary surgical factors in the included patients.
Materials and methods
A total of 1,326 PCNL procedures were performed at our tertiary care center between April 2011 and January 2017. The PCNL technique followed at our center is as follows: an initial percutaneous puncture is made under C-arm fluoroscopy guidance followed by tract dilatation with sequential teflon dilators (Cook) up to 26 F and an Amplatz sheath. Larger tracts (28 or 30 F) are usually reserved for grossly hydronephrotic kidneys with large stone burden. Smaller stones were removed by forceps, while larger or staghorn stones were broken by pneumatic lithoclast prior to their extraction. After complete clearance, a nephrostomy tube was placed. None of our patents required a second-look procedure. Complete blood count, serum creatinine, and X-ray were performed on the first postoperative day. Patients were discharged following nephrostomy tube removal after 24 hours. All patients were confirmed to have a normal coagulation profile preoperatively.
Out of 1,326 patients who underwent PCNL, 21 patients who presented to the emergency room with delayed gross hematuria were included in this study. All included patients were discharged from the hospital following an uneventful PCNL surgery. We defined delayed hematuria as readmission of the patient owing to gross hematuria and previous history of uneventful PCNL and hospital stay. Patients with intra- or perioperative hemorrhage following PCNL during the index admission were excluded. Patients were shifted to the angiography suite on the same day of readmission. Initial stabilization and blood transfusions were restricted only to patients who were hemodynamically unstable. DSA followed by selective TAE, with N-butyl-2-cyanoacrylate (NBCA) glue as the embolizing agent, was performed in a single session. Angiography was performed by an experienced interventional radiologist.
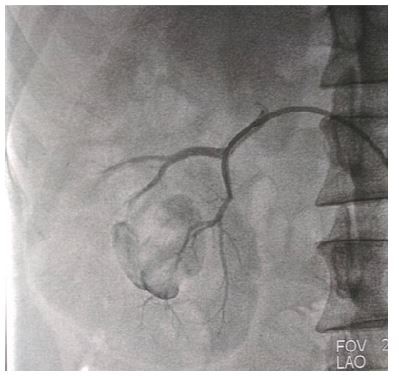
For the DSA procedure, the right main femoral artery was punctured under local anesthesia by using Seldinger technique. A 6 F vascular sheath was inserted as an introducer (Cordis; Johnson & Johnson, Miami, FL, USA). A 5 F Cobra catheter (Cordis; Johnson & Johnson) was introduced over a 0.035-inch diameter guidewire (Terumo, Tokyo, Japan), and an abdominal aortography was obtained by injecting 8–10 mL of contrast media, to demonstrate bilateral main or accessory renal arteries. Subsequently, selective renal DSA was performed by advancing the catheter into the injured branch of the renal artery feeding the lesion. Rapid filming of sequences and careful examination of all phases of the arteriogram were performed to assess the site of bleeding, feeding pedicle, flow pattern, and venous drainage of the vascular lesion. Superselective angiogram was performed by using a 2.8 F microcatheter (Progreat; Terumo). The catheter was inserted as close as possible to the lesion, and was flushed with 10% dextrose before injecting NBCA (Gesika; Reevax Pharma Pvt Ltd, Hyderabad, India) mixed with lipiodol (Guerbet) in 1:2 dilution. The microcatheter was removed immediately after the injection and a check angiogram was performed. Average volume of glue used was 0.5–1.5 mL. The procedure was deemed complete when total occlusion of the lesion and cessation of the hemorrhage was confirmed on the control angiogram. An example of a large PA being embolized by cyanoacrylate glue is shown in Figures 1 and 2.
  | Figure 1 Post-PCNL, large pseudoaneurysm developed in the lower pole with the feeder artery seen during angiography. Abbreviation: PCNL, percutaneous nephrolithotomy. |
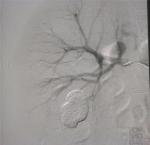  | Figure 2 Successful obliteration of the feeder segmental artery following TAE. Abbreviation: TAE, transcatheter angioembolization. |
“Technical success” of TAE was defined as complete occlusion of the offending vascular lesion as documented by immediate post-procedural angiography. “Clinical success” was defined as cessation of hematuria and the return of hemoglobin and serum creatinine to normal levels, with no recurrence of hemorrhage within 4 weeks following the procedure.
The primary operative and demographic data of the patients were obtained from their hospital medical records. Stone characteristics, number and location of kidney punctures, timing and nature of delayed bleeding, blood transfusion requirements, presence of comorbid diseases such as diabetes mellitus, intraoperative complications, nature of vascular lesions on angiography, and the response to TAE were analyzed. Statistical tests performed included Student’s t-test. All analyses were performed by using a statistical software (R version 3.4.1).
The study was carried out following approval by the institutional ethical board. Written and informed consent was obtained from all patients or their guardians.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Apollo Hospital Ethical Committee (Approval No Uro/2/2017) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Results
A total of 21 patients (males, 18 [85.71%]) with a mean age of 37.05±11.96 years (range, 21–60 years) were included. The right and left kidneys were affected in 9 (42.86%) and 12 (57.14%) patients, respectively. Nineteen (90.48%) patients had staghorn calculi, and one patient each (4.76%) had multiple and single calculus, respectively. In 12 cases (57.14%), multiple punctures were required in addition to upper calyceal entry, as part of PCNL. The average operative time was 84.29±17.92 minutes. Two patients had diabetes mellitus, while four had mildly elevated creatinine levels (Tables S1 and S2).
The mean time of onset of hemorrhage was 10.10±2.67 days post-PCNL. The average time gap between the onset of bleeding and TAE was 4.31±0.64 hours (range, 3.5–5.5 hours) (Table 1). Sixteen patients presented with “sudden-onset” hematuria (urine suddenly turned bright red, with cloturia and clot colic), three with history of “continuous” mild hematuria for a few days followed by an episode of brisk bleeding, and two presented with “hemodynamic instability”.
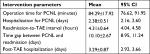  | Table 1 Operating time and duration of hospitalization (n=21) Notes: Data are presented as mean±SD. Abbreviations: PCNL, percutaneous nephrolithotomy; TAE, transcatheter angioembolization. |
The mean fall in the corrected hemoglobin between the pre-PCNL period and the first post-PCNL day was significant (1.71±0.98 g/dL; P-value <0.05). The mean fall in the corrected hemoglobin between the first post-PCNL day and the readmission was also significant (1.67±0.92 g/dL; P-value <0.05). Similarly, there was a significant fall in the post-PCNL to TAE period (–0.55±0.70 g/dL; P-value 0.0013<0.05). There was a significant gain in the hemoglobin values from readmission to 3-month follow-up period (2.17±1.08 g/dL; P-value <0.05), readmission to 24 hours post-TAE period (1.12±1.03; P-value <0.05), and 24 hours post-TAE to 3-month follow-up period (1.05±0.62; P-value <0.05) (Table 2).
  | Table 2 Changes in hemoglobin and creatinine levels Notes: **P-value <0.01, *P-value <0.05. Abbreviations: PCNL, percutaneous nephrolithotomy; TAE, transcatheter angioembolization. |
The number of patients who required blood transfusions during PCNL was seven (33.33%). The mean transfusion volume was 300 mL. The number of patients who received blood transfusions during TAE was six (28.57%), and the mean transfusion volume was 600±509 mL (95% CI: 193, 1007)
DSA was used as the first imaging modality and revealed vascular lesions in all 21 patients. The vascular lesions included PA in 14 (66.66%) cases, AVF in 2 (9.52%), and mixed lesions in 5 (23.81%) (Table S3). Complete cessation of bleeding with source control was achieved in all patients. Two patients required cystoscopy and clot evacuation on the post-TAE day to clear residual clots. However, there was no evidence of fresh bleeding following embolization.
In four patients, creatinine level increased beyond the usually expected elevation following TAE. The elevated levels in these patients were in the range of 2.8–4.1 mg/dL, probably owing to acute renal insufficiency. These values normalized by the time of their discharge from the hospital. The increase in the creatinine level (mg/dL) between the pre-PCNL and post-PCNL period was mild but significant (0.17±0.16; P-value <0.05). There was no significant change in the post-PCNL to readmission period (0.01±0.19; P-value, 0.826>0.05). There was a significant increase in the post-PCNL to TAE period (0.72±0.53; P-value <0.05) and in readmission to 24 hours post-TAE period (0.71±0.53; P-value <0.05). There was a significant reduction in the readmission to 3-month follow-up period (–0.13±0.21; P-value <0.05), and in the 24 hours post-TAE to 3-month follow-up period (–0.84±0.60; P-value <0.05) (Table 2). The changing pattern of hemoglobin and creatinine values from the pre-PCNL time up to 3 months post-TAE is depicted in Table S2. Overall, at the end of 3 months of follow-up, there was no significant change in the creatinine values of our patients.
Discussion
PCNL is the most common modality of removal for renal stones >2 cm size, especially complete staghorn and complex stones. Hemorrhage is a natural accompaniment of PCNL surgery, which is self-limiting in most cases. However, in 2%–23% of cases, “acute massive hemorrhage” necessitating blood transfusion can occur in the intra- or perioperative period.1–4 “Delayed hemorrhage” is relatively uncommon following PCNL (1%–1.8% of all PCNL cases) and is mainly due to traumatic vascular lesions such as PA, AVF, or mixed lesions.6,11–13 This usually starts around 1 week following surgery and presents as an intermittent, continuous, or sudden form of bleeding. Patients often require readmission, blood transfusions, and interventional measures such as DSA and TAE. Selective renal angiography remains the gold standard procedure because of the added advantage of endovascular treatment during the same session, which is the most appropriate treatment modality for arterial lesions.14–17
“Delayed post-PCNL hematuria” most commonly presents as “intermittent bleeding”. According to previous studies, post-PCNL bleeding in stable patients can be managed successfully by conservative measures, and only few (4%–5%) patients require embolization, implying that the majority of patients do not need DSA or TAE.1,3 It is well known that during this period of monitoring, patients may experience clot colic, clot retention, and recurrent bleeding episodes requiring multiple transfusions. All these complications potentially increase the morbidity and hospitalization time.
Abrupt, brisk, and intermittent bleeding is the hallmark of PA and AVF. In the presence of a high suspicion of vascular injury, early renal angiography is a key factor in patient management. Shortening the time gap between the bleeding episode and endovascular treatment may result in reducing the number of hospitalization days.17 According to Jinga et al, the mean interval between debut hematuria and the decision to transfer the patient to the interventional radiology suite is often prolonged (156.72±41.76 hours) in most cases that present with intermittent bleeding.2 Li et al, in a multicenter retrospective study, identified the average time from the onset of bleeding to TAE as 2 days.17
According to literature, despite the 5% negative angiography rate, the presence of a demonstrable and treatable etiology in the remaining 95% strongly supports the use of renal angiography as the first-line imaging modality.18 Thus, the benefits of early DSA far outweigh its disadvantages. In our study, all 21 (100%) cases had demonstrable vascular lesions that were successfully managed by TAE. Also, our interval between debut hematuria and embolization was short (mean, 4.31±0.64 hours), resulting in early diagnosis and timely management of the offending bleeding source. This figure of TAE (1.4% of all PCNL cases) is consistent with the literature review. However, in our study, the proportion of patients presenting with delayed bleeding and the fact that all of them required TAE needs an explanation. It is possible that the majority of patients with mild post-PCNL bleeding may have ignored the initial intermittent bleeding episodes and attended the emergency room only when there was bright red, brisk bleeding. Also, patients may be living at places distant from the hospital restricting their visit only on serious bleeding. Our observations strongly support the need for prompt selective angiography as a first-line measure in all discharged patients presenting as delayed, gross hematuria, without the need to spend time on conservative measures.
TAE is a lifesaving as well as a kidney-sparing procedure. The success rates of TAE ranges from 85% to 100% in different series of patients.1,2,6,7,9,19,20 Our success rate of 100% is consistent with the literature. The choice of embolization material is important in achieving good results, and depends on the accessibility, size, and flow pattern of the vessels to be occluded.2 Ideally, embolization should occlude both the upstream and downstream vessels of the PA. Metallic or microcoils are considered as agents of first choice, followed by gelfoam, autologous blood clot, or glue.13,18
The complications of embolization are rare and include renal artery dissection, coil migration, post-embolization syndrome, non-target embolization, and loss of renal function. In about 5% of cases, TAE fails to stop hemorrhage.4 Renal function can be affected by contrast media-induced nephropathy or collateral loss of functional renal tissue. TAE causes an immediate parenchymal perfusion deficit of 0%–20% (mean deficit, 9%), and a permanent perfusion deficit of 0%–10% (mean deficit, 5%). However, in most cases there is a transient rise in serum creatinine that returns to normal pre-injury levels within 10 days of the procedure.6 Short-term deleterious effects are more pronounced in patients with solitary kidneys. Extremely superselective techniques and the use of platinum microcoils can preserve functional renal parenchyma.13,15,17,18 In our study, no significant post-embolization complications were identified. However, in a few cases, we identified a significant increase in the creatinine level 24 hours post-TAE, which stabilized within the 3-month follow-up period.
Our study is limited by its retrospective nature and small sample size. Moreover, we did not perform follow-up diethylene triamine pentaacetic acid nuclear renogram or contrast-enhanced computed tomography in our cases. Thus, the exact loss of differential renal function or an assessment of the post-embolization infarct area could not be performed. A prospective, multicenter, randomized study comparing primary DSA and initial conservative monitoring is required to confirm their respective roles in the management of patients presenting with delayed hematuria following PCNL.
Conclusion
Delayed post-PCNL bleeding is a rare but severe complication of PCNL. DSA as first-line imaging modality with same-session TAE appears to be a safe, effective, and time-saving alternative to the conventional initial conservative management in patients presenting with this complication. A high index of suspicion for vascular lesions and radiologic acumen is fundamental to their management.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Nouralizadeh A, Ziaee SA, Hosseini Sharifi SH, et al. Delayed postpercutaneous nephrolithotomy hemorrhage: prevalence, predictive factors and management. Scand J Urol. 2014;48(1):110–115. | ||
Jinga V, Dorobat B, Youssef S, et al. Transarterial embolization of renal vascular lesions after percutaneous nephrolithotomy. Chirurgia (Bucur). 2013;108:521–529. | ||
El-Nahas AR, Shokeir AA, El-Assmy AM, et al. Post-percutaneous nephrolithotomy extensive hemorrhage: a study of risk factors. J Urol. 2007;177(2):576–579. | ||
Aminsharifi A, Irani D, Eslahi A. Massive hemorrhage after percutaneous nephrolithotomy: saving the kidney when angioembolization has failed or is unavailable. Int J Surg. 2014;12(8):872–876. | ||
Srivastava A, Singh KJ, Suri A, et al. Vascular complications after percutaneous nephrolithotomy: are there any predictive factors? Urology. 2005;66(1):38–40. | ||
Poulakis V, Ferakis N, Becht E, Deliveliotis C, Duex M. Treatment of renal-vascular injury by transcatheter embolization: immediate and long-term effects on renal function. J Endourol. 2006;20(6):405–409. | ||
Martin X, Murat FJ, Feitosa LC, et al. Severe bleeding after nephrolithotomy: results of hyperselective embolization. Eur Urol. 2000;37(2):136–139. | ||
Akman T, Binbay M, Sari E, et al. Factors affecting bleeding during percutaneous nephrolithotomy: single surgeon experience. J Endourol. 2011;25(2):327–333. | ||
Kessaris DN, Bellman GC, Pardalidis NP, Smith AG. Management of hemorrhage after percutaneous renal surgery. J Urol. 1995;153(3 Pt 1):604–608. | ||
Turna B, Nazli O, Demiryoguran S, Mammadov R, Cal C. Percutaneous nephrolithotomy: variables that influence hemorrhage. Urology. 2007;69(4):603–607. | ||
Lam HS, Lingeman JE, Mosbaugh PG, et al. Evolution of the technique of combination therapy for staghorn calculi: a decreasing role for extracorporeal shock wave lithotripsy. J Urol. 1992;148(3 Pt 2):1058–1062. | ||
Tefekli A, Kurtoglu H, Tepeler K, et al. Does the metabolic syndrome or its components affect the outcome of percutaneous nephrolithotomy? J Endourol. 2008;22(1):35–40. | ||
Richstone L, Reggio E, Ost MC, et al. First prize (tie): hemorrhage following percutaneous renal surgery: characterization of angiographic findings. J Endourol. 2008;22(6):1129–1136. | ||
Sutherland DE, Williams SB, Rice D, Jarrett TW, Engel JD. Vascular pseudoaneurysms in urology: clinical characteristics and management. J Endourol. 2010;24(6):915–921. | ||
Cantasdemir M, Adaletli İ, Cebi D, Kantarci F, Selcuk ND, Numan F. Emergency endovascular embolization of traumatic intrarenal arterial pseudoaneurysms with n-butyl cyanoacrylate. Clin Radiol. 2003;58(7):560–565. | ||
Inci K, Cil B, Yazici S, et al. Renal artery pseudoaneurysm: complication of minimally invasive kidney surgery. J Endourol. 2010;24(1):149–154. | ||
Li L, Zhang Y, Chen Y, et al. A multicentre retrospective study of transcatheter angiographic embolization in the treatment of delayed haemorrhage after percutaneous nephrolithotomy. Eur Radiol. 2015;25(4):1140–1147. | ||
Vignali C, Lonzi S, Bargellini I, et al. Vascular injuries after percutaneous renal procedures: treatment by transcatheter embolization. Eur Radiol. 2004;14(4):723–729. | ||
Ganpule AP, Shah DH, Desai MR. Postpercutaneous nephrolithotomy bleeding: aetiology and management. Curr Opin Urol. 2014;24(2):189–194. | ||
Patterson DE, Segura JW, Leroy AJ, Benson RC, May G. The etiology and treatment of delayed bleeding following percutaneous lithotripsy. J Urol. 1985;133(3):447–451. |
Supplementary materials
  | Table S1 Demographic and primary treatment (PCNL) and TAE characteristics (n=21) Abbreviations: PCNL, percutaneous nephrolithotomy; TAE, transcatheter angioembolization. |
  | Table S2 Hemoglobin and creatinine levels (mean±SD, 95% CI) (n=21) Abbreviations: PCNL, percutaneous nephrolithotomy; TAE, transcatheter angioembolization. |
  | Table S3 Incidence of vascular lesions on angiography (n=21) |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
