Back to Journals » Clinical Interventions in Aging » Volume 15
Relation Between the Incidence of Carotid Artery Calcification and Systemic Diseases
Authors Agacayak KS , Guler R , Sezgin Karatas P
Received 2 April 2020
Accepted for publication 19 May 2020
Published 3 June 2020 Volume 2020:15 Pages 821—826
DOI https://doi.org/10.2147/CIA.S256588
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Kamil Serkan Agacayak,1 Rıdvan Guler,1 Pınar Sezgin Karatas2
1Department of Oral and Maxillofacial Surgery, Dicle University School of Dentistry, Diyarbakır, Turkey; 2Department of Radiology, Diyarbakir Pediatrics Hospital, Diyarbakır, Turkey
Correspondence: Kamil Serkan Agacayak
Dicle University School of Dentistry, Department of Oral and Maxillofacial Surgery, Diyarbakır 21280, Turkey
Tel +90 412 2411017/3364
Email [email protected]
Background: The aim of this study is to investigate the relationship of carotid artery calcifications detected in panoramic radiographs of patients aged 60 or older with isolated systemic diseases.
Patients and Methods: From October 2018 to December 2019, 867 panoramic radiographs of patients, who applied to Dicle University Faculty of Dentistry for various dental reasons, were collected for examination. Of these 867 panoramic radiographs, 444 panoramic radiographs were included in this study. Medical data were collected from the archival records of the dental school.
Results: The study population consisted of 240 female (54.1%) and 204 male (45.9%) patients. Their mean age was 66 ± 7.3 (range: 60– 92) years. Only 39 (8.8%) of the 444 patients had atherosclerotic plaques. Of the 39 patients with carotid artery calcification, 13 (33.3%) were male and 26 (66.7%) were female. As a result of statistical analysis, carotid artery calcification compared to other systemic diseases was found to be significantly more common in patients with hypertension (p = 0.009).
Conclusion: Carotid artery calcifications detected coincidentally in standard panoramic radiographs of dental patients may be important markers for preventing serious risks such as coronary artery disease, stroke, and death. The relationship between carotid artery calcifications found on dental panoramic radiographs and hypertension was significant. Therefore, it seems that detection of carotid artery calcifications on panoramic images of hypertension patients must be considered by dentists.
Keywords: panoramic radiograph, carotid artery calcification, systemic diseases
Introduction
Atherosclerosis is a progressive inflammatory disease that can cause coronary artery disease, peripheral vascular disease, and ischemic cerebrovascular diseases.1 The prevalence of atherosclerosis is very high in many countries and a cause of high mortality rates.2,3 Vascular calcification caused by atherosclerosis is especially common in large and elastic aortic and carotid arteries. Early detection of calcification in these arteries may help to reduce the clinical pathologies caused by atherosclerosis.4 Thromboembolic material developing due to carotid artery calcification (CAC), whether asymptomatic or symptomatic, may lead to a stroke with a blocking effect on the cerebrovascular system.
The main risk factors for atherosclerosis are considered age, gender, endothelial function, genetic predisposition, smoking, alcohol abuse, diabetes mellitus, hypertension, hyperlipidemia, coronary artery disease, obesity and lack of physical activity. Other risk factors include stress, hyperhomocysteinemia, head and neck radiotherapy, obstructive sleep apnea syndrome, and aging.5
Although strokes can be avoided, a major challenge is to develop efficient methods to identify stroke-prone patients. Most non-cardiogenic strokes result from atheroma plaques on panoramic radiographs (PR), in which calcification can be detected in the internal carotid artery.6
Radiographically, calcified atheroma plaques are manifested as irregular, circular, or heterogeneous radiopaque masses, unilateral or bilateral. These plates are generally circular and linear when small; when thin and large, it is rectangular.7 PR is not as useful as Doppler ultrasonography and three-dimensional computed tomography for detecting atherosclerotic plaques in the carotid arteries, especially stenosis of the vessels, but it is less expensive and invasive than other imaging methods. PRs may help in the early diagnosis and evaluation of CACs in patients with or without associated risk factors, thus contributing to reducing the morbidity and mortality rates due to diseases caused by atherosclerosis.8 Dentists play an important role in their early diagnosis by identifying calcified carotid artery atheroma in PRs. CACs are usually located posterosuperiorly to the angle of the mandible, approximately at the inferior margin of the third cervical vertebra (between C3 and C4) near the hyoid bone; however, their location is not limited to the hyoid bone or the thyroid cartilage.9 Carotid atherosclerosis is not the only cause of cervical calcification seen anterior to the cervical vertebrae in PRs. Dentists should be able to distinguish CACs from natural anatomical structures and pathological structures. As anatomical structures similar to CACs, calcified tritic or thyroid cartilage, hyoid bone, calcified stylohyoid ligaments, epiglottis might be counted. As pathological structures similar to CACs, calcified lymph nodes, phlebolites, submandibular salivary gland inflammation and tonsil infection might be said.10
The aim of this study was to determine the presence of CAC on PRs of patients aged 60 years or older with isolated systemic diseases and to investigate the relationship between its incidence and systemic diseases.
Patients and Methods
The study included patients admitted to the Department of Oral and Maxillofacial Surgery. Study was planned on PRs which had received for various dental reasons between October 2018-December 2019. Data regarding their age, sex, previous systemic diseases, drugs used, and chronic diseases and their courses were collected. Informed consent forms were obtained from all the patients for using their data. The study was approved by the Ethics Committee of the Faculty of Dentistry of Dicle University (Protocol No: 53/November 22, 2018). The number of PRs obtained was 844.
The inclusion criteria of the study are written below:
- Male and female patients 60 years and older
- With isolated systemic disease diagnosed at least 5 years ago (Hypertension, diabetes, coronary artery disease, hyperlipidemia, atherosclerosis)
- Radiographs where the image resolution allows the examination of the regions in the working grab
- Patients who do not have regular smoking and alcohol use habits
A number of patients were excluded from the study according to the following criteria
- Patients with two or more systemic diseases, ie multiple systemic diseases
- Diagnosis of systemic disease less than five years prior to the study
- Systemic or physical disability due to obvious inherited causes
- Lack of image clarity due to misuse of the panoramic X-ray system
- Smoking and alcohol use (Patients who are addicted and use regularly)
- Body mass index (BMI) > 30
A total of 444 PRs were finally included according to these criteria. All PRs included in the study were examined by a radiologist with 17 years of experience and using the same monitor, considering differential diagnosis. The research procedure extended over four sessions, spaced by a fi fteen day period. The patient’s data were analyzed according to age, sex, systemic disease, and presence of atheroma plaque. The relationship between the frequency of atheroma plaques and systemic diseases was analyzed.
Panoramic Radiography
All PRs were taken at the Faculty of Dentistry, Dicle University, Diyarbakır, Turkey, using Planmeca ProMax (Helsinki, Finland) panoramic X-ray systems. The exposure value ranges were 1–7.5 mA and 60–70 kV, depending on each patient’s size. According to the differential diagnosis of CAC described by Friedlander and Lande,10 radiopaque nodular masses independent of the hyoid bone adjacent to the cervical vertebrae at or below the C3–C4 intervertebral disc level or the retromandibular area, generally at an angle of about 45° from the mandibular angle, were regarded as CAC. To minimize observation discrepancies, all PRs were evaluated by the same radiologist (Figures 1 and 2).
Statistical Analysis
Statistical analysis was performed using SPSS Statistics 21.0 (Statistical Package for Social Science Inc., Chicago, USA). Numerical variables were expressed as means±standard deviations. The Kolmogorov–Smirnov test was used to determine whether the cases fit the normal distribution. The Mann–Whitney U-test was used for those that did not comply with the normal distribution. The independent-test was performed for the normal distribution. The chi-square test was used for categorical variables. The effect of the independent variables was evaluated by multivariate linear regression analysis. A value of P<0.05 was considered statistically significant.
Results
The study population consisted of 240 female (54.1%) and 204 male (45.9%) patients. Their mean age was 66 ± 7.3 (range: 60–92) years (Table 1). Regarding the distribution of systemic diseases, the most common was hypertension, followed by diabetes, coronary artery disease, atherosclerosis, and hyperlipidemia (Table 2).
 |
Table 1 Distribution of Demographic Features |
 |
Table 2 Distribution of Systemic Diseases in Patients That Included in This Study |
On PRs, CACs were round, irregular, or heterogeneous radiopaque between or just below the vertebrae C3 and C4 (Figure 1). Only 39 (8.8%) of the 444 patients had atherosclerotic plaques. The remaining 405 patients (91.2%) had no observed of atheroma plaques.
Of the 39 patients with CAC, 13 (33.3%) were male and 26 (66.7%) were female. Their medical records were examined and analyzed for possible systemic risk factors. CAC was found to be significantly more common in patients with hypertension compared to other systemic diseases (p = 0.009; Table 3). Twenty-two of these patients (56.4%) had hypertension, 6 (10.5%) had diabetes, 6 (4.4%) had atherosclerosis, 3 (6.1%) had coronary artery disease, and 2 (3.3%) had hyperlipidemia (Table 4).
 |
Table 3 Atheroma Plaque Distribution on the Panoramic X-Ray in the Patients That Included in This Study |
 |
Table 4 Atheroma Plaque Percentages That Seen in Systemic Diseases |
As a result of multivariate analysis of the effects of age, gender and systemic diseases on atheroma plaque, it was observed that age and gender had no effect, but those with systemic disease had a significant effect on the development of atheroma plaque (Table 5).
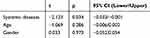 |
Table 5 Multivariate Analysis Results Evaluating the Effect of Age, Gender and Systemic Diseases on Parameters |
Discussion
The objective of this study was to determine the relationship of CACs detected in a PRs of patients aged 60 or older with isolated systemic diseases. We found that CAC was significantly higher in patients with hypertension, which is a systemic disease.
Friedlander and Lande11 were the first to describe the presence of calcification in the common carotid artery region using PR for routine dental diagnoses. Friedlander and Baker12 reported that asymptomatic patients at risk of a stroke could be identified by PRs. Almost 5% of PRs of patients over the age of 30 show detectable CAC.12 In our study, 8.8% CAC was detected.13 However, the higher CAC rate in our study compared to the literature may be due to the group of patients included in the study over 60 years of age. CAC may appear in the form of a nodular or verticolinear radiopacity inferior to the angulus mandible, adjacent to the cervical 3–cervical 4(C3–C4) intervertebral junction.14 Cohen et al15 pointed out that PR is an important marker for detecting atheroma plaque formation in the carotid artery and suggested that patients with CAC should be evaluated for cerebrovascular and cardiovascular risks. Sisman et al reported hyperlipidemia in 31.58% of their patient population with CAC.8 In this study, although more atheroma plaques were found in patients with hypertension than in those with other systemic diseases, this did not reach the level of statistical significance. Nevertheless, hypertension was significantly higher than the other systemic diseases among patients with atheroma plaques. Therefore, we should be alerted in terms of atheroma plaque in patients with hypertension and vice versa for hypertension in patients with atheroma plaques.
CAC may cause ischemic cerebrovascular attacks due to severe stenosis and obstructions.16 In Western societies, this is the underlying reason for approximately 50% of all deaths. Cerebrovascular accidents, or strokes, are the third most common etiology of death in the United States today, preceded only by cardiovascular disease and cancer.17–19 Over 750,000 new or recurrent strokes occur in the United States annually. Atherosclerosis and its more dramatic consequences are stroke and heart attack; are important health problems in other countries as well. In Turkey, too, strokes are the third etiology of death, after cardiovascular disease and cancer.20 Carotid artery disease may not show symptoms until severe contraction or complete obstruction of the carotid arteries occurs. In some people, stroke is the first sign of the disease.19 Therefore, the diagnosis of CAC is very important. Friedlander and Cohen21 reported that 26% of men (mean age 66 years) with CAC diagnosed by PR experienced an adverse vascular event (myocardial infarction, stroke, revascularization, transient ischemic attack, or angina).
Studies on the frequency of CAC have reported varying rates, ranging from 3% to 20%.22–24 In our study, the rate was 8.8%. This result was found to be compatible with the literature. Bayram et al25 evaluated the PRs of 4106 patients and reported the presence of CAC in 88 (2.1%). If we compare our results with the two studies, the reason for the higher rate in our study; The presence of an isolated systemic disease can be explained by regional differences, diet, lifestyle and the average age of our patients. Pornprasertsuk-Damrongsri and Thanakun found CAC in 2.5% of the PRs in a Thai dental patient population.10 In that study, the patients were aged 50 or older. We believe that the higher rate in our study is due to the fact that our patients were 60 or older. Carter et al7 evaluated the prevalence of CAC in PRs from 1175 dental patients at the University of New York and reported a prevalence of 3.6%. Tamura et al26 retrospectively investigated the prevalence of CAC in 2568 PRs from a Japanese population and reported a rate of 4.13%.
The most important risk factors for CAC are hypertension, age, sex, diabetes mellitus, hyperlipidemia, atherosclerosis, and smoking.27 The differences in these factors between populations explain the different rates of CAC from society to society. Ethnicity, diet, and lifestyle are among other factors. In this study, we analyzed hypertension, hyperlipidemia, coronary artery disease, diabetes mellitus, and atherosclerosis as risk factors.28
In our study, the incidence of CAC was twice as high in female (26) than in male (13) patients. Bayram et al25 reported that its incidence in women was approximately three times higher than in men. In Pornprasertsuk-Damrongsri and Thanakun’s10 study, the male-to-female ratio was 1:0.8, which is consistent with that in our study.
Regarding diseases and lifestyle factors associated with CAC, hyperlipidemia, hypertension, cardiovascular diseases, smoking, obesity, renal disease, diabetes mellitus, obstructive sleep apnea syndrome, and periodontitis have been reported.8 In our study, hypertension was observed in 56.4% of the 39 patients who had atherosclerotic plaque, diabetes in 15.3%, atherosclerosis in 15.3%, coronary artery disease in 7.7%, and hyperlipidemia in 5.1%. The high prevalence of hypertension and diabetes among patients with CAC is in line with other studies’ findings. Pornprasertsuk-Damrongsri and Thanakun10 reported hypertension in 52.9% of their patient population with CAC, diabetes mellitus in 29.4%, hyperlipidemia in 14.7%, and smoking in 2.9%. Lewis and Brooks29 reported hypertension 77.8% and diabetes mellitus 22.2% as risk factors. Cohen et al15 examined the PRs of 1879 male patients over 55 years of age and reported that only 3.8% had CAC. In that study, 53.5% of the patients with CAC had hypertension, 36.6% had hyperlipidemia, 22.5% had diabetes mellitus, and 54.9% were smokers. Constantine et al evaluated the PRs of 5780 patients and reported the presence of CAC in 623 (10.8 %).30 In our study, the rate was 8.8%. The reason for the high prevalence of CAC compared to our study may be due to the differences in nutritional habits socially.
Conclusion
CACs detected coincidentally in standard PRs of dental patients may be important markers for preventing serious risks such as coronary artery disease, stroke, and death. Therefore, it seems that detection of CAC on panoramic images of hypertension patients must be considered by dentists. It is necessary to be alerted in terms of atheroma plaque in patients with hypertension and vice versa, in terms of hypertension in patients with atheroma plaques. We believe that more extensive studies are needed in this regard. We think that the patient should be warned in terms of hypertension in patients with CAC on dental PRs.
 |
Figure 1 Diagrammatic illustration of a panoramic radiograph indicating the carotid artery atheromas disposed bilaterally (arrows). |
 |
Figure 2 Panoramic radiography image suggesting the presence of common carotid artery calcifications (arrows). |
Disclosure
The authors report no conflicts of interest in this work.
References
1. Akkemik O, Kazaz H, Tamsel S, Dündar N, Sahinalp Ş, Ellidokuz H. A 5 years follow-up for ischemic cardiac outcomes in patients with carotid artery calcification on panoramic radiographs confirmed by doppler ultrasonography in Turkish population. Dentomaxillofac Radiol. 2020;49:20190440. doi:10.1259/dmfr.20190440
2. Gunen Yilmaz S, Yilmaz F, Bayrakdar IS, Harorli A. The relationship between carotid artery calcification and pulp stone among hemodialysis patients: a retrospective study. Saudi J Kidney Dis Transpl. 2019;30(4):755–763. doi:10.4103/1319-2442.265449
3. Diehm C, Kareem S, Lawall H. Epidemiology of peripheral arterial disease. Vasa. 2004;33(4):183–189. doi:10.1024/0301-1526.33.4.183
4. Santos JM, Soares GC, Alves AP, Kurita LM, Silva PG, Costa FW. Prevalence of carotid artery calcifications among 2500 digital panoramic radiographs of an adult Brazilian population. Med Oral Patol Oral Cir Bucal. 2018;23(3):e256–e261. doi:10.4317/medoral.22350
5. Panico MDB. Hiper-homocisteinemia e doença vascular [Hyperhomocysteinemia and vascular disease]. J Vasc Bras. 2004;3:3–4. Portuguese.
6. Gonçalves JR, Yamada JL, Berrocal C, Westphalen FH, Franco A, Fernandes Â. Prevalence of pathologic findings in panoramic radiographs: calcified carotid artery atheroma. Acta Stomatol Croat. 2016;50(3):230–234. doi:10.15644/asc50/3/5
7. Carter LC, Haller AD, Nadarajah V, Calamel AD, Aguirre A. Use of panoramic radiography among an ambulatory dental population to detect patients at risk of stroke. J Am Dent Assoc. 1997;128:977–984. doi:10.14219/jada.archive.1997.0338
8. Sisman Y, Ertaş ET, Gokce C, Menku A, Ulker M, Akgunlu F. The prevalence of carotid artery calcification on the panoramic radiographs in Cappadocia region population. Eur J Dent. 2007;1(3):132–138. doi:10.1055/s-0039-1698328
9. Nasseh I, Aoun G. Carotid artery calcification: a digital panoramic-based study. Diseases. 2018;6:15. doi:10.3390/diseases6010015
10. Pornprasertsuk-Damrongsri S, Thanakun S. Carotid artery calcification detected on panoramic radiographs in a group of Thai population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(1):110–115. doi:10.1016/j.tripleo.2005.04.002
11. Friedlander AH, Lande A. Panoramic radiographic identification of carotid arterial plaques. Oral Surg Oral Med Oral Pathol. 1981;52(1):102–104. doi:10.1016/0030-4220(81)90181-X
12. Friedlander AH, Baker JD. Panoramic radiography: an aid in detecting patients at risk of cerebrovascular accident. J Am Dent Assoc. 1994;125:1598–1603. doi:10.14219/jada.archive.1994.0237
13. Bayer S, Helfgen EH, Bös C, Kraus D, Enkling N, Mues S. Prevalence of findings compatible with carotid artery calcifications on dental panoramic radiographs. Clin Oral Investig. 2011;15:563–569. doi:10.1007/s00784-010-0418-6
14. Kumagai M, Yamagishi T, Fukui N, Chiba M. Carotid artery calcification seen on panoramic dental radiographs in the Asian population in Japan. Dentomaxillofac Radiol. 2007;36:92–96. doi:10.1259/dmfr/79378783
15. Cohen SN, Friedlander AH, Jolly DA, Date L. Carotid calcification on panoramic radiographs: an important marker for vascular risk. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(4):510–514. doi:10.1067/moe.2002.125580
16. Chen XY, Lam WW, Ng HK, Fan YH, Wong KS. Intracranial artery calcification: a newly identified risk factor of ischemic stroke. J Neuroimaging. 2007;17(4):300–303. doi:10.1111/j.1552-6569.2007.00158.x
17. Hertzer NR, O’Hara PJ, Mascha EJ, Krajewski LP, Sullivan TM, Beven EG. Early outcome assessment for 2228 consecutive carotid endarterectomy procedures: the Cleveland clinic experience from 1989 to 1992. J Vasc Surg. 1997;26:1–10. doi:10.1016/S0741-5214(97)70139-3
18. Friedlander AH. Identification of stroke-prone patients by panoramic and cervical spine radiography. Dentomaxillofac Radiol. 1995;24:160–164. doi:10.1259/dmfr.24.3.8617388
19. Lee WC, Joshi AV, Wang Q, Pashos CL, Christensen MC. Morbidity and mortality among elderly Americans with different stroke subtypes. Adv Ther. 2007;24(2):258–268. doi:10.1007/BF02849893
20. Prime Ministry Republic of Turkey: turkish Statistical Institute (Turkstat) Report. Statistics/social security & health/health statistics/reason of disease; 2005. Available from: http://www.turkstat.gov.tr.
21. Friedlander AH, Cohen SN. Panoramic radiographic atheromas portend adverse vascular events. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(6):830–835. doi:10.1016/j.tripleo.2006.07.016
22. Deahl ST. Panoramic radiography does not reliably detect carotid artery calcification nor stenosis. J Evid Based Dent Pract. 2007;7(4):172–173. doi:10.1016/j.jebdp.2007.09.009
23. Johnsen SH, Mathiesen EB, Joakimsen O, et al. Carotid atherosclerosis is a stronger predictor of myocardial infarction in women than in men: a 6-year follow-up study of 6226 persons: the Tromsø Study. Stroke. 2007;38(11):2873–2880. doi:10.1161/STROKEAHA.107.487264
24. Nemcsik J, Farkas K, Kolossváry E, et al. Intracardiac calcification is a marker of generalized atherosclerosis. Angiology. 2007;58(4):413–419. doi:10.1177/0003319706291112
25. Bayram B, Uckan S, Acikgoz A, Muderrisoglu H, Aydinalp A. Digital panoramic radiography: a reliable method to diagnose carotid artery atheromas? Dentomaxillofac Radiol. 2006;35:266–270. doi:10.1259/dmfr/50195822
26. Tamura T, Inui M, Nakase M, Nakamura S, Okumura K, Tagawa T. Clinicostatistical study of carotid calcification on panoramic radiographs. Oral Dis. 2005;11:314–317. doi:10.1111/j.1601-0825.2005.01125
27. Garcia JH, Khang-Loon H.Carotid atherosclerosis. Definition, pathogenesis, and clinical significance. Neuroimaging Clin N Am. 1996;6(4):801–810.
28. Allison MA, Criqui MH, Wright CM. Patterns and risk factors for systemic calcified atherosclerosis. Arterioscler Thromb Vasc Biol. 2004;24(2):331–336. doi:10.1161/01.ATV.0000110786.02097.0c
29. Lewis DA, Brooks SL. Cartoid artery calcification in a general dental population: a retrospective study of panoramic radiographs. Gen Dent. 1999;47:98–103.
30. Constantine S, Roach D, Liberali S, et al. Carotid artery calcification on orthopantomograms (CACO Study) - is it indicative of carotid stenosis? Aust Dent J. 2019;64(1):4–10. doi:10.1111/adj.12651
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
