Back to Journals » Therapeutics and Clinical Risk Management » Volume 12
Reduction in total recurrent cardiovascular events in acute coronary syndrome patients with low-density lipoprotein cholesterol goal <70 mg/dL: a real-life cohort in a developing country
Authors Chinwong S, Patumanond J , Chinwong D, Joseph Hall J, Arintaya Phrommintikul A
Received 9 September 2015
Accepted for publication 15 December 2015
Published 3 March 2016 Volume 2016:12 Pages 353—360
DOI https://doi.org/10.2147/TCRM.S96016
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Garry Walsh
Surarong Chinwong,1 Jayanton Patumanond,2 Dujrudee Chinwong,1 John Joseph Hall,3 Arintaya Phrommintikul4
1Department of Pharmaceutical Care, Faculty of Pharmacy, Chiang Mai University, Chiang Mai, Thailand; 2Center of Excellence in Applied Epidemiology, Faculty of Medicine, Thammasat University, Pathum Thani, Thailand; 3Centre for Clinical Epidemiology and Biostatistics, School of Medicine and Public Health, Faculty of Health, University of Newcastle, Callaghan, NSW, Australia; 4Department of Internal Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand
Background: For investigations into cardiovascular disease, the first problematic event (ie, nonfatal acute coronary syndrome (ACS), nonfatal stroke, or all-cause mortality) generally was considered as the primary end point; however, ACS patients often experience subsequent events, which are rarely considered. This study reports an investigation into whether achieving a low-density lipoprotein cholesterol (LDL-C) goal of <70 mg/dL (1.8 mmol/L) is associated with a reduction in total recurrent cardiovascular events in a cohort of ACS patients hospitalized in northern Thailand.
Methods: The medical charts and the electronic hospital database of ACS patients treated with statins at a tertiary hospital in Thailand between 2009 and 2012 were reviewed. Patients were checked for their LDL-C goal attainment, and then were followed for subsequent events until the last follow-up date, or to December 31, 2012. The Wei–Lin–Weissfeld method was used for multiple time-to-events data to investigate the association between achieving an LDL-C goal of <70 mg/dL and total recurrent cardiovascular events.
Results: Of 405 eligible patients, 110 patients attained an LDL-C goal of <70 mg/dL. During a median follow-up of 1.94 years, the majority of patients (88.6%) had no subsequent cardiovascular events, while 46 patients experienced at least one recurrent cardiovascular event: 36 with one event, six with two events, two with three events, one with four events, and one with seven events. Compared to patients with an LDL-C ≥100 mg/dL, patients achieving an LDL-C of <70 mg/dL were significantly less likely to experience total cardiovascular events (adjusted hazard ratio =0.29; 95% confidence interval =0.09–0.87; P-value =0.028); the result was similar to patients with an LDL-C of 70–100 mg/dL, but it was not significant (adjusted hazard ratio =0.53; 95% confidence interval =0.23–1.26; P-value =0.154).
Conclusion: ACS patients receiving statins who attained an LDL-C <70 mg/dL experienced a reduction in total recurrent cardiovascular events compared to those with LDL-C ≥100 mg/dL.
Keywords: LDL-C goal, statins, recurrent events, multiple events, subsequent events, WLW method, multiple time-to-events
Introduction
Patients with acute coronary syndrome (ACS) usually experience additional cardiovascular events.1,2 However, the first event was normally considered as primary end point in the analysis, both in randomized controlled trials and observational studies,3–5 resulting in the loss of evaluation of recurrent events. This does not reflect the real-world situation in which patients often experience multiple cardiovascular events. However, the occurrence of subsequent events in addition to the first event is important to both the physicians and patients and should therefore be considered in outcome analysis.1,2,6
Well-established research has shown that patients who achieved low-density lipoprotein cholesterol (LDL-C) levels below 70 mg/dL had an associated decrease in cardiovascular events or mortality.5,7–11 In our setting in Thailand, we found that for ACS patients treated with statins who achieved LDL-C goal <70 mg/dL, the likelihood of experiencing a first cardiovascular event was reduced compared with patients with LDL-C ≥100 mg/dL (adjusted hazard ratio [HR] =0.42; 95% confidence interval (CI) =0.18–0.95; P-value =0.037).5 Recently, the new 2013 ACC/AHA guidelines on cholesterol management12 as well as NICE guidelines on lipid modification13 have abandoned LDL-C goal as a target for therapy in patients treated with statins due to the lack of evidence from randomized controlled trials supporting that achieving LDL-C goal was associated with a reduction in cardiovascular events. The discontinuation of treating to LDL-C target has been debated among experts and some physicians.14–16 On the contrary, some guidelines such as the 2011 ESC/EAS guidelines for the management of dyslipidemias17 and the 2014 National Lipid Association18 still use the LDL-C goal as target for therapy. In our previous study, some ACS patients suffered multiple recurrent cardiovascular events following the first event,5 which led us to investigate if ACS patients who reach LDL-C levels of <70 mg/dL will reduce their likelihood of experiencing the total subsequent events. If this is the case, treating to LDL-C levels of <70 mg/dL (<1.8 mmol/L) is further supported as a target. In that case, it would be desirable to use the LDL-C goal of <70 mg/dL to prevent both the first and recurrent cardiovascular events.
Methods
Ethical approval
The Research Ethics Committee, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand, approved this study protocol prior to the commencement of the study. Since this study is a retrospective study where patients’ information were retrieved from medical records and database of hospital, the Ethics Committee did not need informed consent from the patients.
Setting and study population
The study design and results of the first cardiovascular event in relation to reaching the LDL-C goal of <70 mg/dL have been published previously.5 In brief, the study was carried out at a university-affiliated hospital in the north of Thailand, the Maharaj Nakorn Chiang Mai Hospital, which has 1,400 patient beds and serves 1,300,000 outpatients and 48,000 inpatients from the northern part of the country each year.19 We reviewed the medical charts and electronic hospital database to find patients with a diagnosis of ACS according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision, code of I20 (angina pectoris) or I21 (acute myocardial infarction), between 2009 and 2012. Information collected for these patients included demographic data, comorbidities, risk factors for coronary artery disease, current medication, and laboratory results including lipid profiles: total cholesterol, LDL-C, high-density lipoprotein cholesterol, and triglycerides. Patient data were included into the analysis if records indicated that patients were aged ≥18 years, diagnosed with ACS (unstable angina [UA], non–ST-elevation myocardial infarction [NSTEMI], or ST-elevation myocardial infarction [STEMI]) on discharge date; treated with statins; had LDL-C levels measured at baseline (during admission) and at the first follow-up between 2 weeks to 1 year to determine achieving LDL-C goal; followed from the date of LDL-C goal assessment until the occurrence of the last recurrent cardiovascular events or until December 31, 2012, whichever came first, or the last entry on the medical record of a patient.
Measurement of LDL-C goal and total recurrent cardiovascular outcome
Patients had their LDL-C levels assessed on their first follow-up and were subsequently classified into three groups based on their LDL-C levels: <70 mg/dL (<1.8 mmol/L), 70–99 mg/dL, and ≥100 mg/dL (reference group). An LDL-C <70 mg/dL was considered as achieving the LDL-C goal based on the 2011 ESC/EAS guidelines for the management of dyslipidemias.17
The outcome in this study was the occurrence of any recurrent cardiovascular event experienced by a patient, namely nonfatal ACS (myocardial infarction [MI] or UA), nonfatal stroke, or all-cause mortality. Occurrences of the events included the first cardiovascular event and all subsequent events for each patient; the total recurrent cardiovascular events were considered as the outcome in the analysis. The occurrences of the events must happen following the LDL-C goal assessment for each patient. We considered all cardiovascular events equally (ie, we weighted death and recurrent MI or stroke equally). For example, if a patient had only a nonfatal stroke, this was classified as having only the first recurrent event; if a patient had a nonfatal MI, and then subsequently had a stroke, this patient was characterized as having two recurrent events.
Statistical analysis
We categorized patients based on their LDL-C levels at the first follow-up visit into one of three groups: <70, 70–99, and ≥100 mg/dL. We reported baseline characteristics of patients in numbers, and percentage for categorical variables, and means with standard deviations for continuous variables. We carried out one-way analysis of variance or the Fisher’s exact test, as appropriate, to compare the differences among these three groups. Whereas the analysis from the previous study used the first cardiovascular events as the outcome variable,5 the present study used the total recurrent events as the outcome, and was carried out using multiple time-to-events analysis. We used the Wei–Lin–Weissfeld (WLW) method for our analysis, which uses multiple time-to-event data with a marginal approach based on the Cox proportional hazards model.20 The WLW method regards a total-time approach, which is the time from LDL-C goal assessment to the occurrence of each recurrent cardiovascular event. With this method, all subjects are considered at risk for all recurrent cardiovascular events.20,21 The hazards ratios adjusted for the potential confounders (ie, sex, age, diabetes mellitus, hypertension, serum creatinine, angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, revascularization, and baseline LDL-C level) are presented to show the association between LDL-C goal attainment and total recurrent cardiovascular events. All analyses were carried out with STATA software, version 12 (StataCorp LP, College Station, TX, USA); and two-tailed tests were used for all analyses with a P-value of <0.05 considered to be statistically significant.
Results
Of 1,089 patients hospitalized with ACS at the study hospital between 2009 and 2012, 684 patients were excluded from the analysis due to the lack of LDL-C levels at baseline or follow-up (Figure 1). Baseline characteristics between the two groups were similar except age; included patients were younger than excluded patients (64.9±11.5 vs 67.2±12.9 years; P-value =0.003).
  | Figure 1 Flowchart of patient selection and study timeline. |
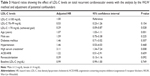
Median follow-up time from the date of measurement of LDL-C goal to the last follow-up date or until December 31, 2012, was 1.94 years (interquartile range of 0.92–2.64). The three groups of patients, categorized according to their LDL-C levels (<70, 70–99, and ≥100 mg/dL), were similar in most other baseline characteristics except that patients with LDL-C <70 mg/dL were older and had lower baseline LDL-C levels compared with the other two groups (Table 1). Twenty-seven percent of patients (110/405) achieved an LDL-C goal of <70 mg/dL. Of 405 ACS patients who were included in the analysis, 46 patients experienced at least one recurrent cardiovascular event; a single event occurred in 36 patients, two events in six patients, three events in two patients, four events in one patient, and seven events in one patient (Table 2). The most common recurrent cardiovascular event was nonfatal ACS (MI or UA): ten events in patients with LDL-C <70 mg/dL, 20 events in patients with LDL-C 70–99 mg/dL, and 23 events in patients with LDL-C ≥100 mg/dL. All ten deaths were considered as a single event because all ten patients died without having prior cardiovascular events.
The results from the analysis using the WLW method show that ACS patients treated with statins who achieved LDL-C levels <70 mg/dL had a lower incidence in total recurrent cardiovascular events compared to patients with an LDL-C ≥100 mg/dL (adjusted HR =0.29; 95% CI =0.09–0.87; P-value =0.028). Similarly, patients with LDL-C levels between 70 and 99 mg/dL were less likely to experience total recurrent cardiovascular events compared with patients with LDL-C levels ≥100 mg/dL, but this was not statistically significant (adjusted HR =0.53; 95% CI =0.23–1.26; P-value =0.154) (Table 3).
Discussion
Our study investigated the impact of achieving LDL-C levels <70 mg/dL on total recurrent cardiovascular events, using the WLW analysis for multiple time-to-events data. Results show that those ACS patients treated with statins who achieved the LDL-C goal had a reduced risk to suffer recurrent cardiovascular events, compared with those patients with LDL-C ≥100 mg/dL.
Multiple time-to-events analysis has been developed and applied to many studies, including investigations into cardiovascular diseases.1,2,6,22–24 The PROVE IT-TIMI 22 trial,2 the IDEAL trial,6 and the TNT trial,24 for instance, showed a reduction in not only the first cardiovascular event but also the recurrent cardiovascular events in patients who received intensive statin therapy compared to those on usual dose statin therapy. The PROVE IT-TIMI 22 trial in patients with ACS2 showed that more potent statin therapy with atorvastatin 80 mg daily was shown to reduce first cardiovascular event by 16%, P-value =0.005, and subsequent event by 19%, P-value =0.009, as compared with moderate potent statin therapy with pravastatin 40 mg daily.2 The IDEAL trial in patients with a history of confirmed acute MI demonstrated that intensive statin therapy (atorvastatin 80 mg daily) was more effective than standard statin therapy (simvastatin 20–40 mg daily) in the prevention of repeated occurrences of cardiovascular events, even beyond the first cardiovascular event. Compared with standard therapy, the relative risk reduction in patients with intensive therapy was reduced by 17% for the first cardiovascular event (P-value <0.0001), by 24% for the second event (P-value <0.0001), by 19% for the third event (P-value =0.035), by 24% for the fourth event (P-value =0.058), and by 28% for the fifth event (P-value =0.117).6
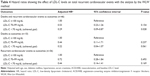
This study, to the best of our knowledge, is the first to investigate the impact of achieving the LDL-C target of <70 mg/dL on total recurrent cardiovascular events, using the WLW method, in the real-world practice. Our findings show that ACS patients treated with statins who achieved LDL-C levels of <70 mg/dL were at reduced risk for total recurrent cardiovascular events. This adds to the knowledge that showed the impact of reaching the LDL-C goal reduced the first cardiovascular event, as reported in our previous study (HR =0.42; 95% CI =0.18–0.95; P-value =0.037).5 When considering only the first recurrent cardiovascular event, the risk was reduced by about 58% for patients who achieved the LDL-C goal; further, the risk was reduced by about 70% when the total recurrent cardiovascular events were taken into account; adjusted HR =0.29; 95% CI =0.09–0.87; P-value =0.028. However, all recurrent events are considered in this type of analysis to reflect the real-life situation, and death may preclude the development of multiple recurrent events. Therefore, we did further analyses by separating the outcomes as only deaths or only recurrent cardiovascular events (Table 4). The analysis that included only ten deaths as the outcomes (excluded 36 patients with recurrent events) with adjustment of potential confounders showed that patients who achieved LDL-C goal of <70 mg/dL were less likely to die as compared to patients with LDL-C ≥100 mg/dL, but it was not significant (HR =0.22; 95% CI =0.04–1.07; P-value =0.061). The further analysis, excluding ten deaths, that included only 36 patients with recurrent events as the outcomes revealed that patients who achieved LDL-C goal of <70 mg/dL were less likely to experience total recurrent events as compared to patients with LDL-C ≥100 mg/dL, but it was not significant (HR =0.44; 95% CI =0.14–1.41; P-value =0.169). Although the results of the additional analyses were not statistically significant, partly due to a small sample size, the results provided a hint that patients achieving LDL-C <70 mg/dL were less likely to experience total recurrent cardiovascular events.
Our study suggests that the total recurrent events should be considered in the analysis to reflect the real-life situation. Our findings highlight the importance of treating to an LDL-C target of <70 mg/dL, suggesting that attention should be paid to ACS patients who cannot achieve the desired LDL-C target to prevent not only the first event but also subsequent cardiovascular events. Importantly, this study supports the use of the LDL-C goal of <70 mg/dL as a target therapy in dyslipidemia management according to the recommendation by the 2011 ESC/EAS guidelines for the management of dyslipidemias17 and the 2014 National Lipid Association18 and as a means of communication between physicians and patients on patients’ progress to prevent subsequent cardiovascular events.
The WLW method has been widely used for analysis of chronic disease with multiple events,6,23,25 including multiple cardiovascular events.6,23 The WLW method was chosen for our analysis based on our research question of whether attaining the LDL-C goal results in reduced total recurrent cardiovascular events after the LDL-C goal is reached. This method uses the time from LDL-C goal assessment to the last recurrent cardiovascular events or the last follow-up date; therefore, each patient is considered to be at risk for all occurrences of recurrent cardiovascular events from the beginning of the observation point, which is from the date of LDL-C goal measurement.6,20,26
Limitations
Some limitations should be noted when interpreting the results. The first limitation is the retrospective study design; hence many patients needed to be excluded due to missing data. Even though potential confounders were controlled through statistical analysis, residual confounders may remain. Second, the number of all ACS patients included in our study is quite small, especially patients who experienced more than one recurrent cardiovascular event; however, it is still reasonable to hypothesize that achieving an LDL-C goal <70 mg/dL is associated with a reduction in total recurrent cardiovascular events in real-world practice. A larger study with a bigger study population and/or a longer period of follow-up is warranted. Third, our analyses are based on the LDL-C goal assessment at the first follow-up visit, which happened between 2 weeks to 1 year, so that changes in the LDL-C levels of patients during the follow-up period were not taken into account. Fourth, other confounders that we did not control for – such as comorbidities (apart from hypertension and diabetes mellitus), adherence to drug therapy, eating behaviors, and daily lifestyle – may be better in those patients with LDL-C <70 mg/dL, and these can affect the results.
Finally, our analysis is based on the WLW method that considers all patients to be at risk for all events; however, some authors suggest that this type of analysis may lead to overestimation of the effect.6,21,27
Despite its limitations, our study reflects real-world practice where patients can experience multiple recurrent events. Our analysis considered total recurrent events, not only the first event to reflect this.
Conclusion
Based on the multiple time-to-event analysis with the WLW method, ACS patients treated with statins who achieved an LDL-C goal of <70 mg/dL were less likely to experience total subsequent cardiovascular events compared to patients with LDL-C ≥100 mg/dL. Our finding supports the “treat to LDL-C target” approach. The LDL-C goal of <70 mg/dL should be used as a target for ACS patients in routine clinical practice to prevent both the first and total recurrent cardiovascular events.
Acknowledgments
We thank the authorities of the Maharaj Nakorn Chiang Mai Hospital for their permission to use the data for the study. We are grateful to Claudia Koller for her assistance with editing this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Murphy SA, Antman EM, Wiviott SD, et al. Reduction in recurrent cardiovascular events with prasugrel compared with clopidogrel in patients with acute coronary syndromes from the TRITON-TIMI 38 trial. Eur Heart J. 2008;29(20):2473–2479. | ||
Murphy SA, Cannon CP, Wiviott SD, McCabe CH, Braunwald E. Reduction in recurrent cardiovascular events with intensive lipid-lowering statin therapy compared with moderate lipid-lowering statin therapy after acute coronary syndromes from the PROVE IT-TIMI 22 (Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis In Myocardial Infarction 22) trial. J Am Coll Cardiol. 2009;54(25):2358–2362. | ||
Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350(15):1495–1504. | ||
de Lemos JA, Blazing MA, Wiviott SD, et al. Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. JAMA. 2004;292(11):1307–1316. | ||
Chinwong D, Patumanond J, Chinwong S, et al. Low-density lipoprotein cholesterol of less than 70 mg/dL is associated with fewer cardiovascular events in acute coronary syndrome patients: a real-life cohort in Thailand. Ther Clin Risk Manag. 2015;11:659–667. | ||
Tikkanen MJ, Szarek M, Fayyad R, et al. Total cardiovascular disease burden: comparing intensive with moderate statin therapy insights from the IDEAL (Incremental Decrease in End Points Through Aggressive Lipid Lowering) trial. J Am Coll Cardiol. 2009;54(25):2353–2357. | ||
LaRosa JC, Grundy SM, Kastelein JJ, Kostis JB, Greten H. Safety and efficacy of atorvastatin-induced very low-density lipoprotein cholesterol levels in patients with coronary heart disease (a post hoc analysis of the treating to new targets [TNT] study). Am J Cardiol. 2007;100(5):747–752. | ||
Wiviott SD, Cannon CP, Morrow DA, Ray KK, Pfeffer MA, Braunwald E. Can low-density lipoprotein be too low? The safety and efficacy of achieving very low low-density lipoprotein with intensive statin therapy: a PROVE IT-TIMI 22 substudy. J Am Coll Cardiol. 2005;46(8):1411–1416. | ||
Ray KK, Bach RG, Cannon CP, et al. Benefits of achieving the NCEP optional LDL-C goal among elderly patients with ACS. Eur Heart J. 2006;27(19):2310–2316. | ||
Blazing MA, Giugliano RP, Cannon CP, et al. Evaluating cardiovascular event reduction with ezetimibe as an adjunct to simvastatin in 18,144 patients after acute coronary syndromes: final baseline characteristics of the IMPROVE-IT study population. Am Heart J. 2014;168(2):205–212.e1. | ||
Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015; 372(25):2387–2397. | ||
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–2934. | ||
National Institute for Health and Care Excellence. Lipid Modification: Cardiovascular Risk Assessment and the Modification of Blood Lipids for the Primary and Secondary Prevention of Cardiovascular Disease. London, UK: National Clinical Guideline Centre; 2014. | ||
Ray KK, Kastelein JJ, Boekholdt SM, et al. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: the good the bad and the uncertain: a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011. Eur Heart J. 2014;35(15):960–968. | ||
Martin SS, Abd TT, Jones SR, Michos ED, Blumenthal RS, Blaha MJ. 2013 ACC/AHA cholesterol treatment guideline: what was done well and what could be done better. J Am Coll Cardiol. 2014;63(24): 2674–2678. | ||
Lopez-Jimenez F, Simha V, Thomas RJ, et al. A summary and critical assessment of the 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: filling the gaps. Mayo Clin Proc. 2014;89(9):1257–1278. | ||
Reiner Z, Catapano AL, De Backer G, et al. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011;32(14):1769–1818. | ||
Jacobson TA, Ito MK, Maki KC, et al. National Lipid Association recommendations for patient-centered management of dyslipidemia: part 1 – executive summary. J Clin Lipidol. 2014;8(5):473–488. | ||
Faculty of Medicine Chiang Mai University [homepage on the Internet]. Chiang Mai, Thailand: Maharaj Nakorn Chiang Mai Hospital. Available from: http://www.med.cmu.ac.th/2013/academic-departments-2/maharaj-nakorn-chiang-mai-hospital.html. Accessed May 15, 2015. | ||
Wei LJ, Lin DY, Weissfeld L. Regression analysis of multivariate incomplete failure time data by modeling marginal distributions. J Am Stat Assoc. 1989;84(408):1065–1073. | ||
Villegas R, Julia O, Ocana J. Empirical study of correlated survival times for recurrent events with proportional hazards margins and the effect of correlation and censoring. BMC Med Res Methodol. 2013;13:95. | ||
Rogers JK, Pocock SJ, McMurray JJ, et al. Analysing recurrent hospitalizations in heart failure: a review of statistical methodology, with application to CHARM-Preserved. Eur J Heart Fail. 2014;16(1):33–40. | ||
Kohli P, Wallentin L, Reyes E, et al. Reduction in first and recurrent cardiovascular events with ticagrelor compared with clopidogrel in the PLATO Study. Circulation. 2013;127(6):673–680. | ||
LaRosa JC, Deedwania PC, Shepherd J, et al. Comparison of 80 versus 10 mg of atorvastatin on occurrence of cardiovascular events after the first event (from the Treating to New Targets [TNT] trial). Am J Cardiol. 2010;105(3):283–287. | ||
Pandeya N, Purdie DM, Green A, Williams G. Repeated occurrence of basal cell carcinoma of the skin and multifailure survival analysis: follow-up data from the Nambour Skin Cancer Prevention Trial. Am J Epidemiol. 2005;161(8):748–754. | ||
Cui J, Forbes A, Kirby A, et al. Semi-parametric risk prediction models for recurrent cardiovascular events in the LIPID study. BMC Med Res Methodol. 2010;10:27. | ||
Kelly PJ, Lim LL. Survival analysis for recurrent event data: an application to childhood infectious diseases. Stat Med. 2000;19(1):13–33. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.