Back to Journals » Research and Reports in Urology » Volume 10
Redo hypospadias surgery: current and novel techniques
Authors Kulkarni SB, Joglekar O, Alkandari MH, Joshi PM
Received 16 March 2018
Accepted for publication 1 June 2018
Published 28 September 2018 Volume 2018:10 Pages 117—126
DOI https://doi.org/10.2147/RRU.S142989
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jan Colli
Video abstract presented by Kulkarni et al.
Views: 332030
Sanjay B Kulkarni, Omkar Joglekar, Mohammad H Alkandari, Pankaj M Joshi
Kulkarni Reconstructive Urology Center, Pune, India
Abstract: Failed hypospadias includes patients with multiple attempts at hypospadias surgery. These present as recurrent stricture, urethrocutaneous fistula glans dehiscence, urethral dehiscence, chordee, and glans deformity. Failed hypospadias is a complex and challenging issue. Various surgeries and techniques have been described for hypospadias. We need uniform guidelines for management of failed hypospadias. In this paper, we highlight the current and feasible options in the management of failed hypospadias which would deliver best long-term cosmetic and functional outcomes for the patients.
Keywords: failed hypospadias, hypospadias cripple, penile stricture, glans dehiscence, urethrocutaneous fistula, chordee
Introduction
Hypospadias has varying presentations in children.
Anthony Mundy in his editorial review said that it is almost impossible to write a satisfactory journal article on failed hypospadias repair.1
Hypospadias encompasses a wide range of abnormalities. This includes the abnormal location of meatus, degree of chordee, the width of urethral plate, and the tilt of glans. This makes the management of hypospadias a complex issue. There has been controversy on many issues ranging from the age at which to operate to the technique to be used as well as the type of procedure to be performed. There are more than 200 mentioned surgeries for hypospadias. The term failed hypospadias was coined for individuals with remaining functional complications after multiple failed attempts at hypospadias.
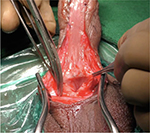
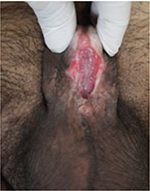
These include recurrent stricture (Figure 1), urethrocutaneous fistula (Figure 2), glans dehiscence, urethral dehiscence, chordee, and glans deformity. Repeated surgery increases the likelihood of recurrent fistulation and restructure formation, mainly because the ventral penile shaft skin is less well vascularized and in turn because of deficient ventral Dartos tissue.
  | Figure 1 Complex penile stricture inpatient with multiple hypospadias repair. |
  | Figure 2 Multiple urethrocutaneous fistula. |
By and large, a majority of hypospadias cripples would have had more than 3 failed prior attempts at urethroplasty.2
Failed hypospadias is an important topic for discussion. This is because the best practices for management of these complications are yet not established. For a young urologist, we need to lay down guidelines and simplify the management of hypospadias cripple.
Thus, in this paper, we review the management of hypospadias cripple.
Materials and methods
Ours is a tertiary referral center for management of urethral stricture. We get referrals from all over the country and the globe.
From 1995–2018 we have performed 4,368 urethroplasties including 1,171 cases of pelvic fracture urethral injuries. We have experience in management of hypospadias cripple. We have performed urethroplasty on more than 200 cases of hypospadias, including primary and failed. Among the failed hypospadias, the minimum number of prior surgeries was 2 and maximum was 17 prior attempts in management of hypospadias.
We will describe the management of hypospadias cripple in our center.
Detailed history of all patients is noted. Previous surgical notes and type of repair performed are thoroughly studied. On examination, we evaluate the length of penis, shape of glans, diameter of glans, width of urethral plate, presence of urethrocutaneous fistula, chordee, and previous scars. The patient or his parents are specifically asked for details on penile curvature. Any photographs taken by the patient of chordee is evaluated. Uroflowmetry is performed. We examine the patient at voiding to look for the stream of urine and presence of urethrocutaneous fistula. The cosmetic appearance of the penis is noted. Many patients have been found to have uncorrected penoscrotal transposition.
Residual urine is evaluated, and ultrasonography is performed to look for upper tract dilation like hydroureteronephrosis.
A surgical plan is made and discussed with the patient and relatives.
We have standardized the management of failed hypospadias in our unit.
Postoperatively, patient is discharged on day 1. Dressing is changed on day 5. Per-urethral Foley’s catheter is kept for 7 days in case of Staged repair and 3 weeks in case of single-stage urethroplasty. Patients receive low-dose antibiotics till catheter removal. On catheter removal, the patient is examined at voiding. Any dehiscence or urethrocutaneous fistula is noted. We maintain a prospective database of all patients operated in our center. Patients are asked to follow-up at 3 monthly intervals for 1 year and 6 monthly thereafter for a period of 5 years and then once a year indefinitely.
Many patients are from outside our city. They visit the referring local urologist who is requested to update us. We routinely use the internet-based applications like WhatsApp and e-mail for collecting patient data, flow rates, symptoms, and the as-required postoperative photographs. Patient confidentially is maintained.
We would like to describe our experience of success rate under the respective individual headings.
Several factors need to be considered before deciding on the type of repair to be performed. However, we will simplify the management of hypospadias cripple.
The main factors determining the type of urethroplasty to be performed depends on the following:
- Scarring of urethral plate
- Width of urethral plate
- Width of glans
- Degree of chordee
- Ventral skin
We will discuss the above factor in specific urethroplasty.
Surgical techniques
Single-stage dorsal inlay urethroplasty
In patients with urethral stricture, we incise the urethra ventrally (Figure 3).3,4 This incision is extended proximally till the normal urethra with good healthy spongiosum. We then measure the width of urethral plate. If the urethral plate is more than 8 mm in width, then decision to perform a single-stage dorsal inlay augmentation urethroplasty is made (Figures 4 and 5). We make a midline incision into the dorsal urethral plate, about 1.5 cm in width. These are multiple parallel incisions and not a single deep midline incision. A buccal graft is harvested by a second team. The graft is inserted as dorsal inlay and quilted to the underlying corpora with 3 rows of continuous quilting sutures. Occasionally, multiple interrupted quilting sutures are made (Figure 6). Periurethral incisions are made and the urethra tubularized using subcuticular sutures over a silicone catheter. Wide glans wings are essential for creating a vertically slit meatus. Glansplasty is done. The second layer of Dartos fascia is sutured to cover. Skin is closed with subcuticular sutures. A suprapubic catheter is inserted.
  | Figure 3 Ventral urethrostomy inpatient with complex penile stricture after failed hypospadias. |
  | Figure 4 Width of urethral plate more than 8 mm – single-stage dorsal inlay augmentation. |
  | Figure 5 Incision till wide proximal good caliber urethra. |
  | Figure 6 Dorsal inlay augmentation. |
In case the urethral plate is narrow, we perform our novel 2-stage urethroplasty which is also described here.
We have performed this repair in 59 patients with a success rate of 94.91%. Two patients had glans dehiscence and 1 had urethrocutaneous fistula. Both were repaired subsequently after a 6 months interval.
Staged buccal graft urethroplasty
We classify patients into 2 main categories, patients with salvageable urethral plate and patients with scarred penis with no urethral plate.
We usually see patients with penile stricture and fistulas.
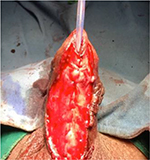
When the urethral plate is scarred, we tend to excise all the scarred tissue (Figure 7). We check the chordee and correct it with multiple ventral transverse corporotomies. In case the curvature still remains, we perform corporal plication on the dorsal side or lateral side as the situation demands.
  | Figure 7 Scarred urethral plate after multiple failed hypospadias urethroplasty. |
We prefer using buccal graft for urethroplasty.5,6–9 Buccal mucosal graft is harvested by a separate team simultaneously. We use cheek grafts and do not prefer using lip grafts. Lip grafts, though mentioned in the literature as being supple, leave behind scarring of the donor site which can be a cosmetic issue. Dartos is mobilized and sutured in the midline. The graft is then placed above the Dartos and quilted with multiple stitches usually as wide as the native urethra (Figures 8 and 9). Placement of the graft on the Dartos helps in tubularization at second stage. It also improves the blood supply to the graft. Literature has mentioned the use of tunica vaginalis flap on the graft bed. We give a tie over dressing on the graft. Parents are taught to keep wetting the dressing by Normal Saline irrigation, which is removed on day 2.
  | Figure 8 Bracka urethroplasty – insertion of buccal graft. |
  | Figure 9 Quilting the graft in Bracka urethroplasty. |
The catheter is removed on day 7. Patient/parents are instructed to keep the graft moist by pouring water at regular intervals in the day time and by application of moisturizer. No medications are given to suppress erections.
Usually, the graft contracts by 15%–20%; hence the reason behind a wide 3 cm graft being inserted in an adult.
There remains a controversy regarding the excision of existing urethral plate. We do not believe in excising any existent plate unless it is extremely scarred. Each and every millimeter of native urethra is helpful for reconstructing a wide urethra.
A buccal graft can be split and inserted around the urethral plate if necessary rather than excision of the plate. One important step of staged urethroplasty is to quilt the graft adequately to the underlying tissue with absorbable sutures.
The patient is evaluated at intervals of 3 months. There is usually some amount of graft contraction that takes place. At 6 months, the graft is supple, and so the second stage of the procedure is performed.
In the second stage, periurethral incisions are made and the neourethra is constructed. This incision is made as lateral as possible. The edges of the graft should be mobilized to the minimum. In case there is scarring of urethral plate, another small graft can be inserted as dorsal inlay augmentation. Dartos is used to cover the urethral repair. Wide glans wings are created. This is essential to avoid meatal stenosis. All the suture lines lie ventrally in hypospadias surgery. A per-urethral Foley’s catheter can put a strain on the suture line and cause dehiscence. Therefore, we usually prefer inserting a suprapubic catheter for all our patients.
The aim is to create a vertical slit meatus which is wide.
All this works provided the graft remains supple and has no contracture.
In our unit, this type of urethroplasty was performed from 1995 until 2010 when we changed our protocol. This has been highlighted in the next section. We have performed this staged urethroplasty in 29 patients. Whenever we have done a staged buccal graft repair, our graft contraction rate was 33%, needing graft revision and redo surgery. Similarly in various high-volume units, the graft contraction (Figure 10) after a Bracka repair is as high as 39%. Mundy1 published interesting work at the American Urology Association. When the Bracka procedure was assessed in the UK, the graft contraction rate was 3%, but when the same procedure was done in Middle East, a graft contraction rate of 39% was observed.10–12
  | Figure 10 Graft contraction. |
This proves the effect of climacteric and ethnic factors in the healing process. We have faced a graft contraction rate of 34%. In such patients, our initial approach was to insert another graft and wait for 6 months. This has also failed in some attempts. We now insert a graft and tubularize the urethra at the same time (Figure 11).
  | Figure 11 Dorsal inlay augmentation in a contracted graft. |
Since necessity is the mother of invention, this graft contracture made us review our technique.
We recently published a novel composite 2-stage urethroplasty for penile urethral strictures, mainly failed hypospadias.
Two stage surgery – novel approach
First stage: Johanson’s
Having assessed the patient clinically in the outpatient department, patients were admitted a day before surgery.12 Patients were requested to apply Betadine scrub solution to genitalia a day before surgery. A single dose of intravenous antibiotic was administered. The patient is placed in supine position. Urethroscopy was performed with a narrow endoscope such as 6 or 4.5 Fr ureteroscope and length of stricture assessed. The urethra was longitudinally opened along its ventral surface and the spongiosum tissue is sutured (Figure 12). The penile skin margins are sutured to the margins of the urethral plate, and the new urinary meatus was located in the healthy urethral mucosa 2 cm proximally to the stricture, leaving a wide open meatus proximally to void through. A 14-Fr Foley silicone catheter is left in place for 7 days. A soft dressing is applied. The dressing is removed on day 2, and patient was discharged from the hospital. Catheter was removed on day 7, and uroflowmetry is performed.
  | Figure 12 Stage I Johanson’s urethroplasty. |
Second-stage urethroplasty using oral mucosal graft inlay: Asopa dorsal inlay Buccal mucosal graft (BMG)
Six months after the first stage, the patients are evaluated clinically for closure of the urethra by second-stage urethroplasty. Uroflowmetry and urine culture were assessed. Three days before surgery patients were requested to apply Betadine scrub to genitalia twice a day and do Chlorhexidine gargles twice a day. On the day of surgery, intravenous broad-spectrum antibiotics are administered. The patients are intubated through the nose, allowing the mouth to be completely free. The patients are operated by 2 surgical teams who work simultaneously, each having its own set of surgical instruments. The oral mucosa graft is harvested from the cheek according to our standard technique used on more than 553 patients. The graft is tailored as per individual case. The patient is placed in supine position. A stay suture is taken at glans and penis stretched. The new meatus after 1 stage is calibrated with the progressive insertion of 10, 12, 14, 16 Fr Nelaton catheters. This gave us the size of proximal normal urethra. The lateral skin incisions of the urethral plate are outlined depicting the narrow urethral plate. The lateral margins of the urethral plate are dissected from the penile skin. A midline dorsal longitudinal mucosal incision of the urethral plate is outlined from the existing meatus to where the neomeatus at glans would be. The urethral plate is incised longitudinally and opened. This is deepened until corpora. Any scarred tissue from previously failed surgeries is excised. A wide bed for the graft is created. The buccal graft harvested is then applied as dorsal inlay (Figure 13). Multiple quilting sutures are done with 6-0 polyglactin. The concept is to make a wide urethral plate using a dorsal inlay buccal graft. This should be as wide as the native proximal urethra. A suprapubic catheter is inserted. A 8-Fr soft tube was used as urethral stent. Urethra is tubularized with subcuticular sutures of polydioxanone (Figures 14 and 15). Glansplasty is performed to create wide vertical slit-like meatus. Meatal reconstruction is most important technically as meatal stenosis will lead to fistula formation.
  | Figure 13 Dorsal inlay buccal graft augmentation. |
  | Figure 14 Periurethral incision. |
  | Figure 15 Urethral tubularization. |
Local Dartos is mobilized and used to cover the suture line. A narrow strip of Dartos may be inserted in between the urethra and glans. The penile skin is meticulously closed. A soft dressing is applied. The soft tube used as a urethral stent is kept just across the constructed urethra. Dressing is removed on day 4, and the patients were discharged. They are requested to follow-up on day 21. After clinical assessment, the urethral stent is removed, and suprapubic tube is clamped. After successful voiding per urethra, the suprapubic tube is removed. Uroflowmetry is recorded. Patients are asked to regularly follow-up every 3 months for 1 year and then annually.
The advantage of this technique is that the buccal graft is not inserted in Stage I. So, graft contraction may be less, and if it happens, it is hidden. Once the graft is inserted in Stage II, the urethra is tubularized. This keeps the graft moist and reduces the risk of graft contraction.
We started performing this technique in 2010. Since then, we have moved away from inserting buccal graft in Stage I (Bracka) unless there are no options. We have performed this type of staged urethroplasty in 53 patients since 2010. Three patients had partial glans dehiscence, 2 developed urinary tract infection (UTI), and 2 had urethrocutaneous fistula. The 2 patients with UTI needed intravenous antibiotics. In 1 patient, the UTI kept recurring, and this was probably due to the presence of previous skin-lined urethra. He has been maintained on low-dose antibiotics. In patients with glans dehiscence and urethrocutaneous fistula, redo surgery was done after an interval of 6 months.
Pedicled preputial flap/tube
Usually, hypospadias cripple has deficient local ventral skin, and circumcision already been done in previous surgeries. In case the prepuce is intact, it can be used as a flap to make the ventral wall of the urethra or it can be tubularized like a preputial tube.13 However, compared to grafts, this is used as last resort. Use of penile/preputial flaps/tubes has high risk of diverticulum formation and should be avoided. The technique of pedicled penile or preputial flap is standard, and it has been described by Asopa et al.13
In multiple failed cases, we use the dorsal penile skin as a pedicled flap and transpose it to the ventral side, using as a onlay cover over the native plate. Two incisions are made on the dorsum of penis, 1.5 cm apart. The incisions are deepened till the level of Buck’s fascia. The skin island is then mobilized on the Dartos pedicle. The mobilization is done till the root of the penis. A button hole is made, and the skin island is transposed ventrally in such a way that the skin overlies as ventral cover for the native urethral plate. An all-silicone catheter is then inserted, and the edges of penile flap are sutured to the native urethral plate. Overlying Dartos acts as a second layer of cover. We have performed this in 5 patients.
It may be challenging to cover the skin on the neourethra. The incision on the dorsal aspect of penis may not be sutured, leaving it to heal by epithelization. This is similar to the concept of penile relaxing incisions which were used for Stage II closure in Johanson’s urethroplasty.
Closure of urethrocutaneous fistula
There may be 1 or many fistulas which are connected between the ventral skin and the urethra. This is as a result of distal meatal stenosis or ischemia of the ventral skin. The management depends on the size of meatus and concomitant stricture. In case meatus is narrow, there is urethral stricture, the urethra is incised ventrally till a good caliber urethra is seen. If the width of urethra is more than 8 mm, then Asopa single-stage dorsal inlay buccal graft augmentation urethroplasty is performed. If the width is <8 mm, then the urethra is kept open and our novel 2-stage approach is used to close the urethra.
If the urethra is normal caliber, then urethrocutaneous fistula can be closed locally.
We use 3 approaches here:
- If the fistula is more than 5 mm in width, peri-fistula incision is made (Figure 16). We use an ophthalmic scalpel as it helps in fine dissection. The fistula tract is cored down till the level of the underlying urethra. Excess fistula tract is excised, and polydioxanone is used to close the fistula (Figure 17). Second-layer closure is done with Dartos tissue. The overlying ventral skin is closed (Figure 18). We usually keep the catheter for 2 weeks. We have done this in 31 patients, which include 5 of our own fistulas. All except 1 were successful.
- If the fistula is narrow, after dissection a suture is passed through the fistula. A small Mosquito forceps is passed through the glans and brought out through the fistula. It grabs the suture and pulls it inside the urethra. This helps in inverting the fistula tract. The direction of the fistula tract is now toward the meatus, and catheter can be removed early. We have used this technique in 14 patients and none required revision.
- Occasionally, when fistula is large and meatus normal we insert a small graft as dorsal inlay through the fistula tract and tubularize the urethra. We have done this in 7 patients, and this has worked well.
  | Figure 16 Peri-fistula incision in a case of urethrocutaneous fistula after hypospadias repair. |
  | Figure 17 Coring the fistula tract till the underlying urethra. |
  | Figure 18 Closure of urethrocutaneous fistula. |
Chordee correction
Chordee in hypospadias is usually due to scarred tissue, short ventral urethra, and disproportionate length of the corporal tissues.
Occasionally, the chordee is corrected by skin dissection or transecting the urethral plate. Majority of the times, there is corporal disproportion which needs to be addressed.
There are 2 options possible: to make the long side short, to make the short side long.
Penile length in hypospadias is precious. Hence, we defer from using penile plication technique for chordee correction. However, if needed, it can be done using the Lue multiple dot technique.
For lengthening the short side, we prefer making several transverse corporotomies, which usually lead to correction. If grafting is needed for chordee correction,then single stage urethroplasty is not recommended. Chordee assessment and correction is done in each individual case.
Discussion
Hypospadias cripple should be managed in specialized high-volume centers. Having multiple surgeries makes each further surgical procedure challenging. Usually, hypospadias cripple merit 2-staged urethroplasty.
Traditionally 2-staged urethroplasty involves the application of buccal mucosa in the first stage for subsequent tubularization after 6 months. In our previous study, involving data of 2 high-volume centers, we found that the use of oral mucosa in the first stage showed a high incidence of scarring and retraction, requiring multiple revisions, with high surgeon and patient disappointment.11 Andrich and Mundy10 presented similar results of staged BMG. The contraction rate of BMG in first stage was 4% in the UK as compared to 33% in Saudi Arabia. Overall, the contraction rate of BMG when placed in the first stage varies between 20% and 38% across all high-volume centers. This contraction rate leads often to revision surgeries.
Oral mucosa is normally in a moist environment in the oral cavity. Application as a staged graft exposes it to dry air and friction with clothes. In our experience, marsupialization of the urethra at the first stage without using any substitution of oral graft appears to be more suitable for an anatomical reconstruction at the second stage using an oral graft as dorsal inlay.4 The oral mucosa is deeply closed inside the urethra, which is a humid canal like the oral cavity, thus reinstating the original environment of the oral mucosa. Based on these reasons, we believed that our composite 2-stage urethroplasty might improve the success rate of complex penile urethroplasty, avoiding the traps of scarring and retraction of the transplanted oral graft.
Conclusion
Hypospadias complication is a challenging reconstructive urology issue. There are no clear guidelines for the management of these types of patients. Traditionally, 2-stage urethroplasty has been used with grafting in first stage leading to revision and graft contraction. Our novel technique of using a graft in the second stage avoids the issue of revision and graft contraction. Patients should be warned of the need for additionally surgery. Mundy1 observed that it takes a surgical lifetime to learn how to deal with all these various problems of hypospadias, and even still it is difficult to categorize satisfactorily the treatment plan for such patients.
In this review, we have simplified the approach and advocate dorsal inlay augmentation for successful management of hypospadias cripple. The idea is still to individualize each case, take down the previous repair, correct the abnormalities and the urethral plate, and reconstruct the urethra and penis to its normal shape and function.
Disclosure
The authors report no conflicts of interest in this work.
References
Mundy AR. Failed hypospadias repair presenting in adults. Eur Urol. 2006;49(5):774–776. | ||
Craig JR, Wallis C, Brant WO, Hotaling JM, Myers JB. Management of adults with prior failed hypospadias surgery. Transl Androl Urol. 2014;3(2):196–204 | ||
Hayes MC, Malone PS. The use of a dorsal buccal mucosal graft with urethral plate incision (Snodgrass) for hypospadias salvage. BJU Int. 1999;83(4):508–509. | ||
Asopa HS, Garg M, Singhal GG, Singh L, Asopa J, Nischal A. Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach. Urology. 2001;58(5):657–659. | ||
Bracka A. The role of two-stage repair in modern hypospadiology. Indian J Urol. 2008;24(2):210–218. | ||
Myers JB, McAninch JW, Erickson BA, Breyer BN. Treatment of adults with complications from previous hypospadias surgery. J Urol. 2012;188(2):459–463. | ||
Barbagli G, Perovic S, Djinovic R, Sansalone S, Lazzeri M. Retrospective descriptive analysis of 1,176 patients with failed hypospadias repair. J Urol. 2010;183(1):207–211. | ||
Leslie B, Lorenzo AJ, Figueroa V, et al. Critical outcome analysis of staged buccal mucosa graft urethroplasty for prior failed hypospadias repair in children. J Urol. 2011;185(3):1077–1082. | ||
Kozinn SI, Harty NJ, Zinman L, Buckley JC. Management of complex anterior urethral strictures with multistage buccal mucosa graft reconstruction. Urology. 2013;82(3):718–722. | ||
Andrich DE, Mundy AR. Climate – a potential cause of primary graft failure in buccal mucosal graft urethroplasty. J Urol. 2009;181(Suppl 4):15. | ||
Barbagli G, De Angelis M, Palminteri E, Lazzeri M. Failed hypospadias repair presenting in adults. Eur Urol. 2006;49(5):887–894 | ||
Joshi PM, Barbagli G, Batra V, et al. A novel composite two-stage urethroplasty for complex penile strictures: a multicenter experience. Indian J Urol. 2017;33(2):155–158. | ||
Asopa HS, Elhence IP, Atri SP, Bansal NK. One stage correction of penile hypospadias using a foreskin tube. A preliminary report. Int Surg. 1971;55(6):435–40. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
