Back to Journals » Psychology Research and Behavior Management » Volume 12
Psychological impact of fibromyalgia: current perspectives
Authors Galvez-Sánchez CM , Duschek S, Reyes del Paso GA
Received 19 November 2018
Accepted for publication 7 January 2019
Published 13 February 2019 Volume 2019:12 Pages 117—127
DOI https://doi.org/10.2147/PRBM.S178240
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Video abstract presented by Carmen M Galvez-Sánchez
Views: 1386
Carmen M Galvez-Sánchez,1 Stefan Duschek,2 Gustavo A Reyes del Paso1
1Department of Psychology, University of Jaén, Jaén, Spain; 2Department of Psychology, University for Health Sciences, Medical Informatics and Technology, Hall in Tirol, Austria
Abstract: Fibromyalgia syndrome (FMS) is a chronic disorder characterized by widespread and persistent musculoskeletal pain and other frequent symptoms such as fatigue, insomnia, morning stiffness, cognitive impairment, depression, and anxiety. FMS is also accompanied by different comorbidities like irritable bowel syndrome and chronic fatigue syndrome. Although some factors like negative events, stressful environments, or physical/emotional traumas may act as predisposing conditions, the etiology of FMS remains unknown. There is evidence of a high prevalence of psychiatric comorbidities in FMS (especially depression, anxiety, borderline personality, obsessive-compulsive personality, and post-traumatic stress disorder), which are associated with a worse clinical profile. There is also evidence of high levels of negative affect, neuroticism, perfectionism, stress, anger, and alexithymia in FMS patients. High harm avoidance together with high self-transcendence, low cooperativeness, and low self-directedness have been reported as temperament and character features in FMS patients, respectively. Additionally, FMS patients tend to have a negative self-image and body image perception, as well as low self-esteem and perceived self-efficacy. FMS reduces functioning in physical, psychological, and social spheres, and also has a negative impact on cognitive performance, personal relationships (including sexuality and parenting), work, and activities of daily life. In some cases, FMS patients show suicidal ideation, suicide attempts, and consummated suicide. FMS patients perceive the illness as a stigmatized and invisible disorder, and this negative perception hinders their ability to adapt to the disease. Psychological interventions may constitute a beneficial complement to pharmacological treatments in order to improve clinical symptoms and reduce the impact of FMS on health-related quality of life.
Keywords: fibromyalgia, background, psychological impact, patients’ experiences, personality, mood
Introduction
Fibromyalgia syndrome (FMS) is a chronic disorder characterized by widespread and persistent musculoskeletal pain that predominantly affects women (between 61% and 90%)1 and has an estimated prevalence of 2%–4% in the general population.2 Other associated symptoms are fatigue, insomnia, morning stiffness, depression, and anxiety.
FMS is frequently accompanied by other conditions such as irritable bowel syndrome, headache, fever, diarrhea, oral ulcers, dry eyes, vomit, constipation, skin rash, hearing difficulties, hair loss, painful and frequent urination, etc.2 FMS is associated with high socioeconomic costs for the health system (medical visits, specialized consultations, diagnostic tests, drugs, and others therapies) and the workforce (sick leave, high rate of absenteeism, and decreased work-related productivity).3,4
FMS was recognized as an illness by the WHO in 1992, being included in the ICD-10 under code number M79.5 The etiology of FMS remains unknown. Current pathophysiological models assume a central sensitization to pain and impairments in endogenous pain inhibitory mechanisms4,6–8 (Figure 1). This idea is supported by the existence of hyperalgesia and allodynia, low thresholds and tolerance to pain, development of pain sensitization in the dorsal horns of the spinal cord in response to repeated pain, and greater brain responses to pain evocation observed in areas of the pain neuromatrix.6–8,10,11 However, other authors have considered neurological origin of FMS, based on the discovery of small fiber12,13 and large fiber14 neuropathy in the affected patients.12 Moreover, the involvement of idiopathic cerebrospinal pressure dysregulation in FMS pathology is discussed.15 In 1990, the American Colleague of Rheumatology (ACR) established the first diagnostic criteria for FMS, wherein pain pressure up to 4 kg/cm2 was evaluated at 18 body points; pain elicited in at least eleven of them was required for a diagnosis.16 However, these criteria were widely criticized due to the difficulties in using pressure algometry in primary health care and the limited predictive validity with respect to clinical pain.17 Thus, in 2010, a new proposal was presented by the ACR exclusively based on the use of two scales: the Widespread Pain Index (WPI) and the Severity Scale (SS). The WPI includes a list of 19 painful areas and the SS involves an evaluation of the severity of certain clinical symptoms. For an FMS diagnosis, a WPI score ≥7 and SS score ≥5 or a WPI score between 3 and 6 and SS score ≥9 is needed. As with 1990 criteria, the symptoms must be present continuously over the period of at least 3 months.2
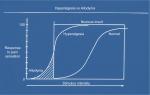  | Figure 1 Hyperalgesia and allodynia. Note: Reprinted from Current Biology, 8(15), Martin WJ, Malmberg AB, Basbaum AI, Pain: nocistatin spells relief, R525–R527, Copyright (1998), with permission from Elsevier.9 |
Vulnerability factors in fibromyalgia
Some factors seem to predispose individuals to FMS, such as accidents (traffic and work injuries, fractures, polytraumatisms), medical interventions and complications (such as from surgeries and infections), and emotional traumas (sexual and physical abuse and neglect).18–20 Environmental factors like stressful life events may be associated with FMS onset.21,22 FMS patients who report sexual or physical abuse tend to experience poorer psychological adjustment, greater psychological distress, and more severe clinical symptoms, and use more health care services.23–25 In general, studies have found an association between traumas during childhood and adolescence (not only abuse or violence, but also negligence and other negative life events) and level of disability in FMS.26 Dysregulation of stress response mechanisms may antecede the development of FMS and other chronic conditions like chronic fatigue syndrome. Early stress in human development could alter stress mechanisms, leading to increased vulnerability to stress-related disorders. As such, lengthy trauma or life stress in childhood and adulthood seems to negatively affect brain modulatory systems, of both pain and emotions.27 Though life experiences may partially explain the high prevalence of emotional disorders and alterations in pain modulation in FMS, the corresponding state of research does not allow definite conclusions.
FMS patients show blunted HPA (hypothalamus–pituitary–adrenal) reactivity (particularly at the pituitary level), which leads to an inappropriate cortisol response to stress or activities of daily living.28,29 FMS patients also displayed aberrant autonomic regulation17 with lower activity of both the sympathetic and parasympathetic branches (such as higher heart rate and lower heart rate variability, blood pressure, stroke volume, etc) and reduced reactivity to physical and psychological stressors.30,31 This leads to a reduced capacity to face and cope successfully with environmental and daily life demands. Furthermore, the activity of the baroreflex, the main mechanism mediating the antinociceptive effect of blood pressure, is decreased.26,27 Moreover, the negative effect of negative life events seems to be enhanced and maintained due to the patients’ tendency toward catastrophizing,10 avoidance, or inhibition of their emotions.32
Physical inactivity and sedentary lifestyles, and the associated increase in body mass index (BMI), have been suggested as factors associated with FMS.33,34 Activity avoidance is associated with poorer function in individuals with chronic pain, and predicted poorer physical and psychological functioning and higher pain-related interference with daily life.35 Overactive patterns can also contribute in the long term to increased risk of pain exacerbation, and patients with an overactive coping style when engaging in daily life activities usually report poorer physical and psychological function.35 In contrast, patients who pace themselves (such as by slowing down and taking breaks to facilitate goal attainment) in their daily activities report lower pain interference and greater psychological function and pain control.35
Family aggregation in FMS, suggesting genetic influences, has been observed.36–38 There is a greater prevalence of mood disorders (especially major depressive and bipolar disorders) and reduced pressure pain thresholds in the relatives of FMS patients. However, the specific genes and mechanisms of transmission are unknown, although they are probably polygenic, for instance, HLA antigen class I and II, DR4, 5-HTT, 5-HTTLPR, D2 receptor, catechol-O-methyltransferase polymorphism, etc.36,37
In spite of the evidence regarding the abovementioned predisposing factors (which cannot be considered causal), more research is needed to comprehensively understand their contribution to FMS origin and maintenance.39
Impact on health-related quality of life
FMS negatively affects functioning at the physical, psychological, and social levels, impairing social relationships, ability to fulfill family and work responsibilities, daily life activities, and mental health, not only due to pain but also because of fatigue, cognitive deficits, and other associated symptoms.40–42 The quality of life of relatives can also be affected. Work is especially affected due to the tension between health problems (pain, fatigue, muscle weakness, limited physical capacity, increased stress, and increased need of rest) and work-related demands.43,44 It is important to provide familial and general social support to FMS workers, taking into account the fact that working patients show better health status and adaptation than non-working patients.45,46 FMS patients should have the opportunity to adjust their work situation and workload according to their reduced physical capacity for fulltime work, or decide definitively if they can or cannot work.47,48 In this vein, the WHO recommends workplace adjustments for health reasons.49
FMS negatively affects sexual health50 and is related to reproduction problems51 and female sexual dysfunctions,52,53 such as hypoactive sexual desire,54 sexual aversion, orgasm disorder, vaginismus, and dyspareunia.55 Characteristic FMS symptoms (particularly widespread pain, fatigue, sleep disorders, and hypersensitivity and intolerability to tactile and pressure stimuli)56 together with psychiatric comorbidities57 (especially anxiety and depression),58,59 body image problems,60 decreased lubrication,61 pelvic floor muscle problems,62 and medication side effects,63 are some of the main causes of sexual problems (Table 1). With a multidisciplinary approach, it is necessary to treat sexual problems in FMS, as they are not only a cause of discomfort, which worsens symptoms and quality of life, but also lead to interpersonal problems and the breakup of couples.64
  | Table 1 Biological and psychosocial aspects of FMS sexual dysfunctions Abbreviation: FMS, fibromyalgia syndrome. |
Cognitive impact of fibromyalgia
Lower cognitive performance has been found in FMS patients compared to healthy people.33,65,66 FMS patients usually report cognitive impairments, especially problems in planning, attention, memory (in the working, semantic, and episodic domains), executive functions, and processing speed.33,67,68 These findings accord with self-reported cognitive deficits, which usually include concentration difficulties, forgetfulness, decreased vocabulary, poor verbal fluency, and mental slowness.69,70 Nevertheless, the cognitive deficit does not seem to be global.71 Additionally, higher levels of fatigue have been found during cognitive tasks in FMS patients compared to healthy people.72
The main mediating factor of these cognitive deficits is the severity of clinical pain.73–75 Secondary explanatory factors are emotional-affective problems (particularly anxiety, depression, and negative emotional states),76,77 fatigue, and insomnia.78–80
Emotional and affective impact of fibromyalgia
FMS is linked to greater negative affect,74–76 which involves a general state of distress composed of aversive emotions like sadness, fear, anger, and guilt.77 In addition, FMS patients tend to experience high levels of stress,78,79 anger (including anger-in or anger suppression, anger-out or anger expression, and angry rumination),80–82 and pain catastrophizing (conceptualized as an exaggerated negative orientation to pain, which provokes fear and discomfort and increases pain perception),83 which are frequently associated with a worsening of symptoms,84 including cognitive ones.66
Psychiatric disorders can accompany rheumatic diseases and may increase disability and mortality, as well as reduce quality of life in these patients.85,86 FMS patients display a high rate of anxiety (20%–80%)87 and depressive disorders (13%–63.8%).88 Specifically, a higher prevalence in FMS patients than in the general population was observed for generalized anxiety disorder, panic attack, phobias,89 obsessive compulsive disorder,90 post-traumatic stress disorder,90,91 major depressive disorder,92 dysthymia,93 and bipolar disorders.94,95
The intensity of negative affective states is positively associated with increased pain intensity, irritability, physical and mental strain, functional limitations, the number of tender points, non-restorative sleep, cognitive deficits, fatigue, and the impact of the illness on quality of life.90,96,97 FMS patients usually feel isolated, misunderstood, or rejected by relatives, friends, health workers, and society in general. This may contribute to the high prevalence of depression, along with the constant and intense pain.90 There is also evidence of high levels of anxiety related to FMS patients’ heightened perception of pain and somatization of symptoms.88
Chronic pain is a risk factor for suicidal behaviors.98 In the case of FMS, the estimated prevalence of suicidal attempts has been reported as 16.7%,99 rising to 58.3% in the case of FMS with comorbid migraine.100 Thus, FMS patients have a higher rate of suicide attempts than the general population, where their risk of suicide is similar to that observed in other chronic diseases.101 Suicidal behaviors in FMS include suicidal ideation,102,103 suicide attempts,104 and death by suicide.105,106 The risk of suicide in FMS is increased due to the presence of a constellation of factors that are usually related to suicide, such as being female,107 psychological distress, poor sleep quality,108,109 enhanced fatigue,110 psychiatric comorbidities (especially depression, bipolar disorders, and borderline personality),101,108,111 and physical comorbidities (like headache and gastric diseases).101 Suicidal ideation is more common than suicide attempts112 and the latter occurs ten times more frequently than suicide.113 Suicidal ideation in FMS is related to comorbid depression, anxiety, and a high negative impact on daily life activities.103 The inclusion of FMS patients in suicide risk assessments in clinical practice, to prevent suicide, is an important consideration in clinical practice.
Personality, temperament, character, and fibromyalgia
Personality characteristics modulate an individual’s response to psychological stressors27 and adjustment to chronic illness.27 An “FMS personality” is a topic that remains under debate. While some authors have found characteristic FMS traits,27 others have failed to find any particular personality features.114
Some personality disorders appear to be more prevalent in FMS patients than in the general population, including obsessive-compulsive personality disorder,115,116 borderline personality,94 avoidant personality disorder,117,118 and histrionic personality disorder.115 Some studies have observed a predominance of certain personality traits in FMS, such as perfectionism,119,120 alexithymia,84,121 neuroticism,27,122,123 psychocitism,123 avoidant personality traits,115,117,118 and type D personality124 (which combine high negative affect with social inhibition).125
Some studies have focused on the Big Five Model of Personality, which includes five dimensions: extraversion vs introversion, agreeableness vs antagonism, conscientiousness vs impulsivity, neuroticism vs emotional stability, and openness vs closed-mindedness.126 In FMS, high neuroticism and low conscientiousness (high impulsivity) have been found, which seem to be related to high levels of chronic pain.126 Furthermore, in some FMS patients, the high level of neuroticism is usually accompanied by low extraversion, contributing to more severe psychosocial problems.127 Extraversion in FMS is associated with lower levels of pain, anxiety, and depression, and better mental health, thereby constituting a protective influence against FMS.45 In general, the presence of personality disorders and negative personality traits in FMS is associated with poorer results after pain treatment,128,129 a worsening of the functional status, higher health care demands (particularly in terms of increased number of medical visits), and greater occupational and medical costs.118,130
Some studies have focused on the temperament and character of FMS patients, mainly based on Cloninger’s Personality Model, using the Temperament and Character Inventory.131 High harm avoidance, high self-transcendence, low cooperativeness, and self-directedness have been found in FMS patients.132–134 Harm avoidance is related to pessimism, concerns about the future, fear of the unknown, and shyness. Self-transcendence can be conceptualized as spiritual ideas that involve a state of unified consciousness in which everything is an integral part of a totality, favoring a spiritual union with the universe. Self-transcendence has been associated with post-traumatic stress and psychotic symptoms, such as borderline, narcissistic, schizotypal, and paranoid symptoms.135 Low levels of cooperativeness include social intolerance, lack of social interest, and a tendency to further their own interests. People with low self-directedness usually have difficulties in accepting responsibility and being independent, and show a lack of long-term goals, low motivation, and low self-esteem.131
Impact of FMS on self-concept
The few studies available in this field have found lower self-esteem66,136,137 levels in FMS patients. Lower self-esteem is related to a reduction of cognitive performance in FMS, especially in terms of attention, memory, and planning abilities.66 FMS patients tend to experience a higher need to earn self-esteem through competence and others’ approval. It is known that self-esteem is related to self-confidence and self-efficacy expectations.136,137 Self-efficacy (the confidence one has in one’s ability to perform or resolve a specific behavior or problem)138 or perceived self-efficacy (individuals’ beliefs in their capacities to achieve certain goals)139 is usually low in FMS patients.140,141 Pain-related self-efficacy, conceptualized as beliefs about the ability to perform activities despite pain,142 is also damaged in FMS.140,143 A high positive association has been found between self-efficacy and treatment adherence and improvements in FMS, with better self-efficacy being associated with more positive outcomes.140,141 Thus, interventions aimed at increasing self-esteem may be useful to improve expectations of self-efficacy and the patient’s own ability to manage their illness, thus promoting better adaptation to the disease.144
Several studies have shown a precarious or negative self-image in FMS patients.116,145 Self-image problems are associated with the notion of an ill person, which radically alters FMS patients’ self-identity. Moreover, FMS patients’ self-image seems to be modified during the development and course of the illness146 and therapeutic interventions,147 affecting their self-identity.148 In spite of the relevance of the self-image concept, few studies to date have addressed this issue.
Body image is part of the overall self-image and is defined as the subjective perceptions, feelings, and thoughts about the physical body. It includes perceptual and affective components,149 which are usually affected in pain-related illnesses.150 Indeed, there is evidence of a negative body image in FMS patients,151,152 further exacerbated by the high prevalence of overweight and obesity.153,154 FMS body image also seems to be influenced by the illness-affected body parts (especially painful and stiff areas), problems in cognitive function, negative health care experiences, activity limitations, and decreased quality of life.151
Patient beliefs about fibromyalgia
The unknown etiology of FMS and the lack of objective diagnostic markers of the disease have led to a debate about its legitimacy and controversies regarding its true nature.114 The negative experience of FMS patients is exacerbated due to the occasional perception that it is not a genuine disease.155 Additionally, FMS patients cite the lack of physical markers of the illness as a reason for the delay in diagnosis and the source of doubts about the authenticity of the illness.151 Many FMS patients report that their family and friends do not understand their disease;156–158 this lack of support could affect their functioning and recovery. Some studies have confirmed the relevance of support from family, friends, and health care staff for managing daily life with chronic illnesses, including FMS.159,160
In this way, FMS patients feel a double burden because their life is dominated by pain but it is not adequately acknowledged.161 In fact, the process of FMS diagnosis is stressful for patients due to the lack of objective clinical markers and physician doubts, together with the general uncertainty of the process.162 The majority of FMS patients feel relieved when they finally receive their FMS diagnosis. However, this relief tends to evaporate when they realize the ineffectiveness of treatments and the illness prognosis.163,164
Patients with FMS experience a sense of invisibility because of debates regarding the authenticity of the diagnosis, treatment, and health care in general.155,165 Moreover, FMS patients usually feel embarrassed because they are no longer able to perform daily tasks as before.156 In fact, they have problems in planning daily life activities and interactions with family and their social circles due to the severity of their symptoms, such that they become more isolated.157,161,166 Dissatisfaction with the patient–doctor relationship is another recurring problem, together with frustration due to uncertainty regarding the etiology and treatment of FMS.164
FMS seems to undermine patients’ self-confidence and sense of self155 and disrupts their identity.167 In this sense, FMS patients experience a transition or change in identity due to the illness, which is apparently invisible to the people who saw them when healthy due on the basis of their external or physical appearance.168
Clearly, FMS patients can be perceived negatively, which worsens their symptoms and functioning. In their own words, they experience “illness intrusiveness” characterized as disruptions of valued activities, lifestyle, and interests, leading to compromised global quality of life. Evidence also suggests that feelings of vulnerability and apprehension about having a chronic illness of unknown origin may contribute to limiting patients’ activities, inability to sustain work, and somatic distress.169,170
Conclusion
FMS is associated with a high prevalence of emotional and affective disorders (particularly depression, anxiety, borderline personality, obsessive-compulsive personality, and post-traumatic stress disorder), and main symptoms and comorbidities may mutually reinforce each other. FMS reduces functioning in the physical, psychological, and social spheres, and has a negative impact on personal relationships (including sexuality and parenting), work, daily activities, and mental health. FMS patients also show problems in cognitive performance, especially in planning, attention, memory, executive functions, and processing speed. There is also evidence of high levels of negative affect, neuroticism, perfectionism, stress, anger, and alexithymia in FMS patients. High harm avoidance together with high self-transcendence, low cooperativeness, and low self-directedness have been found as temperament and character features of FMS patients. Furthermore, FMS patients tend to have a negative self-image and body image perception, as well as low self-esteem and perceived self-efficacy. In some cases, FMS patients show suicidal ideation, suicide attempts, and consummated suicide. FMS patients perceived the illness as a stigmatized and invisible disorder that is difficult to understand. The negative illness perception and lack of social support worsen their symptoms and functioning.
Due to the scarce etiological knowledge about FMS, there is currently no agreement about its appropriate therapy, and treatment effects have been claimed to be unsatisfactory.171 However, various interventions, especially combinations of pharmacological with other types of treatments, may be helpful in reducing FMS symptoms and their impact on quality of life. Some evidence is available for positive effects of moderate aerobic exercise, cognitive-behavioral therapy, self-management programs, mindfulness training, and acceptance and commitment therapy.3,172 Furthermore, educative programs may help in increasing self-confidence, self-esteem, and pain self-efficacy.173 Finally, FMS patients should stay active at the physical and social levels, and avoid sedentary lifestyles in order to control BMI and improve functioning and health-related quality of life.174 However, further research is clearly warranted in order to establish a platform from which to develop guidelines regarding psychological interventions in FMS.
Disclosure
The authors report no conflicts of interest in this work.
References
Wolfe F, Walitt B, Perrot S, Rasker JJ, Häuser W. Fibromyalgia diagnosis and biased assessment: sex, prevalence and bias. PLoS One. 2018;13(9):e0203755. | ||
Wolfe F, Clauw DJ, Fitzcharles MA, et al. The American College of rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). 2010;62(5):600–610. | ||
Arnold LM, Gebke KB, Choy EH. Fibromyalgia: management strategies for primary care providers. Int J Clin Pract. 2016;70:99–112. | ||
Galvez-Sánchez CM. Depression and trait-anxiety mediate the influence of clinical pain on health related quality of life in fibromyalgia. J Affect Disord. 2019. | ||
World Health Organization. International Statistical Classification of Diseases and Related Problems. ICD-10. Geneva: WHO; 1992. | ||
de la Coba P, Bruehl S, Moreno-Padilla M, Reyes Del Paso GA. Responses to slowly repeated evoked pain stimuli in fibromyalgia patients: evidence of enhanced pain sensitization. Pain Med. 2017;18(9):1778–1786. | ||
de la Coba P, Bruehl S, Galvez-Sánchez CM, Reyes Del Paso GA. Slowly repeated evoked pain as a marker of central sensitization in fibromyalgia: diagnostic accuracy and reliability in comparison with temporal summation of pain. Psychosom Med. 2018;80(6):573–580. | ||
Montoro CI, Duschek S, de Guevara CM, Reyes Del Paso GA. Patterns of cerebral blood flow modulation during painful stimulation in fibromyalgia: a transcranial Doppler sonography study. Pain Med. 2016;17(12):2256–2267. | ||
Martin WJ, Malmberg AB, Basbaum AI. Pain: nocistatin spells relief. Curr Biol. 1998;8(15):R525–R527. | ||
Gracely RH, Geisser ME, Giesecke T, et al. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain. 2004;127(Pt 4):835–843. | ||
De La Coba P, Bruehl S, Galvez-Sánchez CM, Reyes del Paso GA. Specificity of slowly repeated evoked pain in comparison with traditional pain threshold and tolerance measures in fibromyalgia patients. Psychosom Med. 2018;80(6):573–580. | ||
Farhad K, Oaklander AL. Fibromyalgia and small-fiber polyneuropathy: what’s in a name? Muscle Nerve. 2018;58(5):611–613. | ||
Martínez-Lavín M. Fibromyalgia and small fiber neuropathy: the plot thickens! Clin Rheumatol. 2018;37(12):3167–3171. | ||
Caro XJ, Galbraith RG, Winter EF. Evidence of peripheral large nerve involvement in fibromyalgia: a retrospective review of EMG and nerve conduction findings in 55 FM subjects. Eur J Rheumatol. 2018;5(2):104–110. | ||
Hulens M, Dankaerts W, Stalmans I, et al. Fibromyalgia and unexplained widespread pain: the idiopathic cerebrospinal pressure dysregulation hypothesis. Med Hypotheses. 2018;110:150–154. | ||
Wolfe F, Smythe HA, Yunus MB, et al. The American College of rheumatology 1990 criteria for the classification of fibromyalgia. Arthritis Rheum. 1990;33(2):160–172. | ||
Gracely RH, Petzke F, Wolf JM, Clauw DJ. Functional magnetic resonance imaging evidence of augmented pain processing in fibromyalgia. Arthritis Rheum. 2002;46(5):1333–1343. | ||
Raphael KG, Janal MN, Nayak S, Schwartz JE, Gallagher RM. Psychiatric comorbidities in a community sample of women with fibromyalgia. Pain. 2006;124(1–2):117–125. | ||
Nicolson NA, Davis MC, Kruszewski D, Zautra AJ. Childhood maltreatment and diurnal cortisol patterns in women with chronic pain. Psychosom Med. 2010;72(5):471–480. | ||
Low LA, Schweinhardt P. Early life adversity as a risk factor for fibromyalgia in later life. Pain Res Treat. 2012;2012:140832. | ||
Albrecht PJ, Rice FL. Fibromyalgia syndrome pathology and environmental influences on afflictions with medically unexplained symptoms. Rev Environ Health. 2016;31(2):281–294. | ||
Gupta A, Silman AJ. Psychological stress and fibromyalgia: a review of the evidence suggesting a neuroendocrine link. Arthritis Res Ther. 2004;6(3):98–106. | ||
Theoharides TC, Tsilioni I, Arbetman L, Panagiotidou S. Fibromyalgia, a syndrome in search of pathogenesis and therapy. J Pharmacol Exp Ther. 2015;355:255–263. | ||
Häuser W, Galek A, Erbslöh-Möller B, et al. Posttraumatic stress disorder in fibromyalgia syndrome: prevalence, temporal relationship between posttraumatic stress and fibromyalgia symptoms, and impact on clinical outcome. Pain. 2013;154(8):1216–1223. | ||
Williams DA, Clauw DJ. Understanding fibromyalgia: lessons from the broader pain research community. J Pain. 2009;10(8):777–791. | ||
Gonzalez B, Baptista TM, Branco JC, Ferreira AS. Fibromyalgia: antecedent life events, disability, and causal attribution. Psychol Health Med. 2013;18(4):461–470. | ||
Malin K, Littlejohn GO. Personality and fibromyalgia syndrome. Open Rheumatol J. 2012;6(1):273–285. | ||
Van Houdenhove B. Premorbid “overactive” lifestyle and stress-related pain/fatigue syndromes. J Psychosom Res. 2005;58(4):389–390. | ||
Van Houdenhove B, Egle UT. Fibromyalgia: a stress disorder? piecing the biopsychosocial puzzle together. Psychother Psychosom. 2004;73(5):267–275. | ||
Reyes Del Paso GA, Garrido S, Pulgar A, Martín-Vázquez M, Duschek S. Aberrances in autonomic cardiovascular regulation in fibromyalgia syndrome and their relevance for clinical pain reports. Psychosom Med. 2010;72(5):462–470. | ||
Reyes del Paso GA, Garrido S, Pulgar Á, Duschek S, Pulgar A. Autonomic cardiovascular control and responses to experimental pain stimulation in fibromyalgia syndrome. J Psychosom Res. 2011;70(2):125–134. | ||
Horowitz MJ. Stress-response syndromes: a review of posttraumatic and adjustment disorders. Hosp Community Psychiatry. 1986;37(3):241–249. | ||
Mork PJ, Vasseljen O, Nilsen TIL. Association between physical exercise, body mass index, and risk of fibromyalgia: longitudinal data from the Norwegian Nord-Trøndelag health study. Arthritis Care Res (Hoboken). 2010;62(5):611–617. | ||
Muñoz Ladrón de Guevara C, Fernández-Serrano MJ, Reyes del Paso GA, Duschek S. Executive function impairments in fibromyalgia syndrome: relevance of clinical variables and body mass index. PLoS One. 2018;13(4):e0196329. | ||
Racine M, Galán S, de la Vega R, et al. Pain-related activity management patterns and function in patients with fibromyalgia syndrome. Clin J Pain. 2018;34(2):122–129. | ||
Arnold LM, Hudson JI, Hess EV, et al. Family study of fibromyalgia. Arthritis Rheum. 2004;50(3):944–952. | ||
Buskila D, Sarzi-Puttini P. Biology and therapy of fibromyalgia genetic aspects of fibromyalgia syndrome. Arthritis Res Ther. 2006;8(5):218. | ||
Arnold LM, Fan J, Russell IJ, et al. The fibromyalgia family study: a genome-wide linkage scan study. Arthritis Rheum. 2013;65(4):1122–1128. | ||
Wolfe F, Häuser W, Walitt BT, Katz RS, Rasker JJ, Russell AS. Fibromyalgia and physical trauma: the concepts we invent. J Rheumatol. 2014;41(9):1737–1745. | ||
Freitas RPA, Andrade SC, Spyrides MHC, Albuquerque Barbosa MT, Sousa MBC. Impacts of social support on symptoms in Brazilian women with fibromyalgia. Rev Bras Rheumatol. 2017;57(3):197–203. | ||
Karper WB. Effects of exercise, patient education, and resource support on women with fibromyalgia: an extended long-term study. J Women Aging. 2016;28(6):555–562. | ||
Neuprez A, Crielaard JM. Fibromyalgie: état de la question en 2017 [Fibromyalgia: state of the issue in 2017]. Rev Med Liege. 2017;72(6):288–294. French. | ||
Mannerkorpi K, Gard G. Hinders for continued work among persons with fibromyalgia. BMC Musculoskelet Disord. 2012;13(1):96. | ||
Henriksson CM, Liedberg GM, Gerdle B. Women with fibromyalgia: work and rehabilitation. Disabil Rehabil. 2005;27(12):685–694. | ||
Ilmarinen J. Work ability – a comprehensive concept for occupational health research and prevention. Scand J Work Environ Health. 2009;35(1):1–5. | ||
Juuso P, Skär L, Sundin K, Söderberg S. The workplace experiences of women with fibromyalgia. Musculoskeletal Care. 2016;14(2):69–76. | ||
Palstam A, Bjersing JL, Mannerkorpi K. Which aspects of health differ between working and nonworking women with fibromyalgia? A cross-sectional study of work status and health. BMC Public Health. 2012;12(1):1076. | ||
Reisine S, Fifield J, Walsh S, Forrest DD. Employment and health status changes among women with fibromyalgia: a five-year study. Arthritis Rheum. 2008;59(12):1735–1741. | ||
World Health Organization. Healthy workplace. Framework and Model. Background and supporting literature and practice 2010. Available from: http://www.who.int/occupational health/evelyn hwpspanish.pdf. Accessed September 20, 2018. | ||
Zielinski RE. Assessment of women’s sexual health using a holistic, patient-centered approach. J Midwifery Womens Health. 2013;58(3):321–327. | ||
Shaver JL, Wilbur J, Robinson FP, Wang E, Buntin MS. Women’s health issues with fibromyalgia syndrome. J Womens Health (Larchmt). 2006;15(9):1035–1045. | ||
Kalichman L. Association between fibromyalgia and sexual dysfunction in women. Clin Rheumatol. 2009;28(4):365–369. | ||
Rico-Villademoros F, Calandre EP, Rodríguez-López CM, et al. Sexual functioning in women and men with fibromyalgia. J Sex Med. 2012;9(2):542–549. | ||
Burri A, Greven C, Leupin M, Spector T, Rahman Q. A multivariate twin study of female sexual dysfunction. J Sex Med. 2012;9(10):2671–2681. | ||
Incesu C. Sexual function and dysfunctions. Klinik Psikiyatri. 2004;Ek3:3–13. | ||
Rosenbaum TY. Musculoskeletal pain and sexual function in women. J Sex Med. 2010;7(2 Pt 1):645–653. | ||
Lewis RW, Fugl-Meyer KS, Bosch R, et al. Epidemiology/risk factors of sexual dysfunction. J Sex Med. 2004;1(1):35–39. | ||
Monga TN, Tan G, Ostermann HJ, Monga U, Grabois M. Sexuality and sexual adjustment of patients with chronic pain. Disabil Rehabil. 1998;20(9):317–329. | ||
Ambler N, Williams AC, Hill P, Gunary R, Cratchley G. Sexual difficulties of chronic pain patients. Clin J Pain. 2001;17(2):138–145. | ||
Yilmaz H, Yilmaz SD, Polat HA, Salli A, Erkin G, Ugurlu H. The effects of fibromyalgia syndrome on female sexuality: a controlled study. J Sex Med. 2012;9(3):779–785. | ||
Burri A, Lachance G, Williams FM. Prevalence and risk factors of sexual problems and sexual distress in a sample of women suffering from chronic widespread pain. J Sex Med. 2014;11(11):2772–2784. | ||
Lisboa LL, Sonehara E, Oliveira KC, Andrade SC, Azevedo GD. Kinesiotherapy effect on quality of life, sexual function and climacteric. Clinical nursing research symptoms in women with fibromyalgia. Rev Bras Rheumatol. 2015;55:209–215. | ||
Bazzichi L, Giacomelli C, Rossi A, et al. Fibromyalgia and sexual problems. Reumatismo. 2012;64(4):261–267. | ||
Poh LW, He HG, Chan WCS, et al. Experiences of patients with rheumatoid arthritis: a qualitative study. Clin Nurs Res. 2017;26(3):373–393. | ||
Glass JM. Fibromyalgia and cognition. J Clin Psychiatry. 2008;69 (Suppl 2):20–24. | ||
Galvez-Sánchez CM, Reyes Del Paso GA, Duschek S. Cognitive impairments in fibromyalgia syndrome: associations with positive and negative affect, Alexithymia, pain Catastrophizing and self-esteem. Front Psychol. 2018;9:377. | ||
Glass JM, Park DC, Minear M, Crofford LJ. Memory beliefs and function in fibromyalgia patients. J Psychosom Res. 2005;58(3):263–269. | ||
Dailey DL, Keffala VJ, Sluka KA. Do cognitive and physical fatigue tasks enhance pain, cognitive fatigue, and physical fatigue in people with fibromyalgia? Arthritis Care Res (Hoboken). 2015;67(2):288–296. | ||
Duschek S, Werner NS, Winkelmann A, Wankner S. Implicit memory function in fibromyalgia syndrome. Behav Med. 2013;39(1):11–16. | ||
Munguía-Izquierdo D, Legaz-Arrese A, Moliner-Urdiales D, Reverter-Masía J. Neuropsicología de los pacientes con síndrome de fibromialgia: relación con dolor y ansiedad [Neuropsychological performance in patients with fibromyalgia syndrome: relation to pain and anxiety]. Psicothema. 2008;20(3):427–431. Spanish. | ||
Reyes Del Paso GA, Pulgar Á, Duschek S, Garrido S. Cognitive impairment in fibromyalgia syndrome: the impact of cardiovascular regulation, pain, emotional disorders and medication. Eur J Pain. 2012;16(3):421–429. | ||
Peñacoba Puente C, Velasco Furlong L, Écija Gallardo C, Cigarán Méndez M, Bedmar Cruz D, Fernández-de-Las-Peñas C. Self-efficacy and affect as mediators between pain dimensions and emotional symptoms and functional limitation in women with fibromyalgia. Pain Manag Nurs. 2015;16(1):60–68. | ||
Hassett AL, Simonelli LE, Radvanski DC, Buyske S, Savage SV, Sigal LH. The relationship between affect balance style and clinical outcomes in fibromyalgia. Arthritis Rheum. 2008;59(6):833–840. | ||
Finan PH, Zautra AJ, Davis MC. Daily affect relations in fibromyalgia patients reveal positive affective disturbance. Psychosom Med. 2009;71(4):474–482. | ||
Malin K, Littlejohn GO. Stress modulates key psychological processes and characteristic symptoms in females with fibromyalgia. Clin Exp Rheumatol. 2013;31(6 Suppl 79):64–71. | ||
Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–1070. | ||
Glass JM. Review of cognitive dysfunction in fibromyalgia: a convergence on working memory and attentional control impairments. Rheum Dis Clin North Am. 2009;35(2):299–311. | ||
Kivimäki M, Leino-Arjas P, Virtanen M, et al. Work stress and incidence of newly diagnosed fibromyalgia: prospective cohort study. J Psychosom Res. 2004;57(5):417–422. | ||
Van Houdenhove B, Egle U, Luyten P. The role of life stress in fibromyalgia. Curr Rheumatol Rep. 2005;7(5):365–370. | ||
Ricci A, Bonini S, Continanza M, et al. Worry and anger rumination in fibromyalgia syndrome. Reumatismo. 2016;68(4):195–198. | ||
van Middendorp H, Lumley MA, Jacobs JW, van Doornen LJ, Bijlsma JW, Geenen R. Emotions and emotional approach and avoidance strategies in fibromyalgia. J Psychosom Res. 2008;64(2):159–167. | ||
Sayar K, Gulec H, Topbas M. Alexithymia and anger in patients with fibromyalgia. Clin Rheumatol. 2004;23(5):441–448. | ||
Baastrup S, Schultz R, Brødsgaard I, et al. A comparison of coping strategies in patients with fibromyalgia, chronic neuropathic pain, and pain-free controls. Scand J Psychol. 2016;57(6):516–522. | ||
Montoro CI, Reyes del Paso GA, Duschek S. Alexithymia in fibromyalgia syndrome. Pers Individ Dif. 2016;102:170–179. | ||
Ang DC, Choi H, Kroenke K, Wolfe F. Comorbid depression is an independent risk factor for mortality in patients with rheumatoid arthritis. J Rheumatol. 2005;32(6):1013–1019. | ||
Bazzichi L, Maser J, Piccinni A, et al. Quality of life in rheumatoid arthritis: impact of disability and lifetime depressive spectrum symptomatology. Clin Exp Rheumatol. 2005;23(6):783–788. | ||
Fietta P, Fietta P, Manganelli P. Fibromyalgia and psychiatric disorders. Acta Biomed. 2007;78(2):88–95. | ||
Uçar M, Sarp Ü, Karaaslan Ö, Gül AI, Tanik N, Arik HO. Health anxiety and depression in patients with fibromyalgia syndrome. J Int Med Res. 2015;43(5):679–685. | ||
Pando-Fernández MP. Fibromyalgia and psychotherapy. Rev Digit Med Psicosom Psicoter. 2011;1:1–42. | ||
Coppens E, Van Wambeke P, Morlion B, et al. Prevalence and impact of childhood adversities and post-traumatic stress disorder in women with fibromyalgia and chronic widespread pain. Eur J Pain. 2017;21(9):1582–1590. | ||
Galek A, Erbslöh-Möller B. Mental disorders in patients with fibromyalgia syndrome: screening in centers of different medical specialties. Schmerz Berl Ger. 2013;27:296–304. | ||
Steiner JL, Sm B, Slaven JE. The complex relationship between pain intensity and physical functioning in fibromyalgia: the mediating role of depression. J Appl Biobehav Res. 2017:1–12. | ||
Soriano-Maldonado A, Amris K, Ortega FB, et al. Association of different levels of depressive symptoms with symptomatology, overall disease severity, and quality of life in women with fibromyalgia. Qual Life Res. 2015;24(12):2951–2957. | ||
Alciati A, Sarzi-Puttini P, Batticciotto A, et al. Overactive lifestyle in patients with fibromyalgia as a core feature of bipolar spectrum disorder. Clin Exp Rheumatol. 2012;30(6 Suppl 74):122–128. | ||
Di Tommaso Morrison MC, Carinci F, Lessiani G, et al. Fibromyalgia and bipolar disorder: extent of comorbidity and therapeutic implications. J Biol Regul Homeost Agents. 2017;31(1):17–20. | ||
Thieme K, Turk DC, Flor H. Comorbid depression and anxiety in fibromyalgia syndrome: relationship to somatic and psychosocial variables. Psychosom Med. 2004;66(6):837–844. | ||
Staud R, Koo E, Robinson ME, Price DD. Spatial summation of mechanically evoked muscle pain and painful aftersensations in normal subjects and fibromyalgia patients. Pain. 2007;130(1–2):177–187. | ||
Kye SY, Park K. Suicidal ideation and suicidal attempts among adults with chronic diseases: a cross-sectional study. Compr Psychiatry. 2017;73:160–167. | ||
Kurth T, Scher AI. Suicide risk is elevated in migraineurs who have comorbid fibromyalgia. Neurology. 2015;85(12):1012–1013. | ||
Jimenez-Rodríguez I, García-Leiva JM, Jiménez-Rodríguez BM, Condés-Moreno E, Rico-Villademoros F, Calandre EP. Suicidal ideation and the risk of suicide in patients with fibromyalgia: a comparison with non-pain controls and patients suffering from low-back pain. Neuropsychiatr Dis Treat. 2014;10:625–630. | ||
Chen-Chia L, Chun-Hung T, Jiunn-Horng CH. A nationwide population-based cohort study. Medicine. 2016;95(44):e5187. | ||
Calandre EP, Navajas-Rojas MA, Ballesteros J, Garcia-Carrillo J, Garcia-Leiva JM, Rico-Villademoros F. Suicidal ideation in patients with fibromyalgia: a cross-sectional study. Pain Pract. 2015;15(2):168–174. | ||
Triñanes Y, González-Villar A, Gómez-Perretta C, Carrillo-de-La-Peña MT. Suicidality in chronic pain: predictors of suicidal ideation in fibromyalgia. Pain Pract. 2015;15(4):323–332. | ||
Calandre EP, Vilchez JS, Molina-Barea R, et al. Suicide attempts and risk of suicide in patients with fibromyalgia: a survey in Spanish patients. Rheumatology (Oxford). 2011;50(10):1889–1893. | ||
Dreyer L, Kendall S, Danneskiold-Samsøe B, Bartels EM, Bliddal H. Mortality in a cohort of Danish patients with fibromyalgia: increased frequency of suicide. Arthritis Rheum. 2010;62(10):3101–3108. | ||
Wolfe F, Hassett AL, Walitt B, Michaud K. Mortality in fibromyalgia: a study of 8,186 patients over thirty-five years. Arthritis Care Res. 2011;63(1):94–101. | ||
Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30(1):133–154. | ||
Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73(9):e1160–e1167. | ||
Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National comorbidity survey replication. J Psychiatr Res. 2009;43(5):526–531. | ||
Kleiman EM, Turner BJ, Chapman AL, Nock MK. Fatigue moderates the relationship between perceived stress and suicidal ideation: evidence from two high-resolution studies. J Clin Child Adolesc Psychol. 2018;47(1):116–130. | ||
Bolton JM, Walld R, Chateau D, Finlayson G, Sareen J. Risk of suicide and suicide attempts associated with physical disorders: a population-based, balancing score-matched analysis. Psychol Med. 2015;45(3):495–504. | ||
Hawton K, van Heeringen K. Suicide. The Lancet. 2009;373(9672):1372–1381. | ||
Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. | ||
Johannsson V. Does a fibromyalgia personality exist? J Musculoskel Pain. 1993;1(3–4):245–252. | ||
Uguz F, Ciçek E, Salli A, et al. Axis I and axis II psychiatric disorders in patients with fibromyalgia. Gen Hosp Psychiatry. 2010;32(1):105–107. | ||
Hellström O, Bullington J, Karlsson G, Lindqvist P, Mattsson B. A phenomenological study of fibromyalgia. Patient perspectives. Scandinavian J Primary Health Care. 2009;17(1):11–16. | ||
Fu T, Gamble H, Siddiqui U, Schwartz T. Psychiatric and personality disorder survey of patients with fibromyalgia. Annals Depres Anxiet. 2015;2(6):1064. | ||
Gumà-Uriel L, Peñarrubia-María MT, Cerdà-Lafont M, et al. Impact of IPDE-SQ personality disorders on the healthcare and societal costs of fibromyalgia patients: a cross-sectional study. BMC Fam Pract. 2016;17(1):61. | ||
Herken H, Gürsoy S, Yetkin OEoe, Virit O, Esgi K. Personality characteristics and depression level of the female patients with fibromyalgia syndrome. Int Med J. 2001;8:41–44. | ||
Sirois FM, Molnar DS. Perfectionism and maladaptive coping styles in patients with chronic fatigue syndrome, irritable bowel syndrome and fibromyalgia/arthritis and in healthy controls. Psychother Psychosom. 2014;83(6):384–385. | ||
Castelli L, Tesio V, Colonna F, et al. Alexithymia and psychological distress in fibromyalgia: prevalence and relation with quality of life. Clin Exp Rheumatol. 2012;30(6 Suppl 74):70–77. | ||
Vural M, Berkol TD, Erdogdu Z, Kucukserat B, Aksoy C. Evaluation of personality profile in patients with fibromyalgia syndrome and healthy controls. Mod Rheumatol. 2014;24(5):823–828. | ||
Montoro CI, Reyes del Paso GA. Personality and fibromyalgia: relationships with clinical, emotional, and functional variables. Pers Individ Dif. 2015;85:236–244. | ||
van Middendorp H, Kool MB, van Beugen S, Denollet J, Lumley MA, Geenen R. Prevalence and relevance of type D personality in fibromyalgia. Gen Hosp Psychiatry. 2016;39:66–72. | ||
Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med. 2005;67(1):89–97. | ||
Bucourt E, Martaillé V, Mulleman D, et al. Comparison of the big five personality traits in fibromyalgia and other rheumatic diseases. Joint Bone Spine. 2017;84(2):203–207. | ||
Torres X, Bailles E, Valdes M, et al. Personality does not distinguish people with fibromyalgia but identifies subgroups of patients. Gen Hosp Psychiatry. 2013;35(6):640–648. | ||
Elliott TR, Jackson WT, Layfield M, Kendall D. Personality disorders and response to outpatient treatment of chronic pain. J Clin Psychol Med Settings. 1996;3(3):219–234. | ||
Uomoto JM, Turner JA, Herron LD. Use of the MMPI and MCMI in predicting outcome of lumbar laminectomy. J Clin Psychol. 1988;44(2):191–197. | ||
Uguz F, Kucuk A, Cicek E, et al. Quality of life in rheumatological patients: the impact of personality disorders. Int J Psychiatry Med. 2015;49(3):199–207. | ||
Cloninger C. Personality and Psychopathology. Washington, DC: American Psychiatric Press, Inc; 1999. | ||
Gencay-Can A, Can SS. Temperament and character profile of patients with fibromyalgia. Rheumatol Int. 2012;32(12):3957–3961. | ||
Balbaloglu O, Tanik N, Alpayci M, Hakan AK, Karaahmet E, Inan LE. Paresthesia frequency in fibromyalgia and its effects on personality traits. Int J Rheum Dis. 2018;21(7):1343–1349. | ||
Garcia-Fontanals A, García-Blanco S, Portell M, et al. Cloninger’s psychobiological model of personality and psychological distress in fibromyalgia. Int J Rheum Dis. 2016;19(9):852–863. | ||
Yoon SJ, Jun CS, An HY, Kang HR, Jun TY. Patterns of temperament and character in patients with posttraumatic stress disorder and their association with symptom severity. Compr Psychiatry. 2009;50(3):226–231. | ||
Michielsen HJ, van Houdenhove B, Leirs I, Vandenbroeck A, Onghena P. Depression, attribution style and self-esteem in chronic fatigue syndrome and fibromyalgia patients: is there a link? Clin Rheumatol. 2006;25(2):183–188. | ||
Garaigordobil M. Fibromialgia: discapacidad funcional, autoestima Y perfil de personalidad [Fibromyalgia: functional disability, self-esteem and personality profile]. Inf Psicol. 2013;106:4–16. Spanish. | ||
Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. | ||
Bandura A. Self-efficacy: The Exercise of Control. New York: Freeman; 1997. | ||
Mannerkorpi K, Svantesson U, Broberg C. Relationships between Performance-based tests and patients’ ratings of activity limitations, self-efficacy, and pain in fibromyalgia. Arch Phys Med Rehabil. 2006;87(2):259–264. | ||
Rasmussen MU, Amris K, Rydahl-Hansen S, et al. Are the changes in observed functioning after multi-disciplinary rehabilitation of patients with fibromyalgia associated with changes in pain self-efficacy? Disabil Rehabil. 2017;39(17):1744–1752. | ||
Bandura A, O’Leary A, Taylor CB, Gauthier J, Gossard D. Perceived self-efficacy and pain control: opioid and nonopioid mechanisms. J Pers Soc Psychol. 1987;53(3):563–571. | ||
Vong SK, Cheing GL, Chan CC, Chan F, Leung AS. Measurement structure of the pain self-efficacy questionnaire in a sample of Chinese patients with chronic pain. Clin Rehabil. 2009;23(11):1034–1043. | ||
Denison E, Asenlöf P, Lindberg P. Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain. 2004;111(3):245–252. | ||
Baptista AS, Jones A, Jones A, Jones A. Effectiveness of dance in patients with fibromyalgia: a randomized, single-blind, controlled study. J Natour Clin Exp Rheumatol. 2012;30(6 Suppl 74):18–23. | ||
Bojner Horwitz E, Kowalski J, Theorell T, Anderberg UM. Dance/movement therapy in fibromyalgia patients: changes in self-figure Drawings and their relation to verbal self-rating scales. Arts Psychother. 2006;33(1):11–25. | ||
Van Houdenhove B, Neerinckx E, Onghena P, Vingerhoets A, Lysens R, Vertommen H. Daily hassles reported by chronic fatigue syndrome and fibromyalgia patients in tertiary care: a controlled quantitative and qualitative study. Psychother Psychosom. 2002;71(4):207–213. | ||
Asbring P. Chronic illness – a disruption in life: identity-transformation among women with chronic fatigue syndrome and fibromyalgia. J Adv Nurs. 2001;34(3):312–319. | ||
Grogan S. Body image and health: contemporary perspectives. J Health Psychol. 2006;11(4):523–530. | ||
Lotze M, Moseley GL. Role of distorted body image in pain. Curr Rheumatol Rep. 2007;9(6):488–496. | ||
Boyington JE, Schoster B, Callahan LF. Comparisons of body image perceptions of a sample of black and white women with rheumatoid arthritis and fibromyalgia in the US. Open Rheumatol J. 2015;9(1):1–7. | ||
Neumann L, Lerner E, Glazer Y, Bolotin A, Shefer A, Buskila D. A cross-sectional study of the relationship between body mass index and clinical characteristics, tenderness measures, quality of life, and physical functioning in fibromyalgia patients. Clin Rheumatol. 2008;27(12):1543–1547. | ||
Kim CH, Luedtke CA, Vincent A, Thompson JM, Oh TH. Association of body mass index with symptom severity and quality of life in patients with fibromyalgia. Arthritis Care Res (Hoboken). 2012;64(2):222–228. | ||
Okifuji A, Bradshaw DH, Olson C. Evaluating obesity in fibromyalgia: neuroendocrine biomarkers, symptoms, and functions. Clin Rheumatol. 2009;28(4):475–478. | ||
Lempp HK, Hatch SL, Carville SF, Choy EH. Patients’ experiences of living with and receiving treatment for fibromyalgia syndrome: a qualitative study. BMC Musculoskelet Disord. 2009;10(1):124. | ||
Arnold LM, Crofford LJ, Mease PJ, et al. Patient perspectives on the impact of fibromyalgia. Patient Educ Couns. 2008;73(1):114–120. | ||
Söderberg S, Strand M, Haapala M, Lundman B. Living with a woman with fibromyalgia from the perspective of the husband. J Adv Nurs. 2003;42(2):143–150. | ||
Thorne SE, Harris SR, Mahoney K, Con A, McGuinness L. The context of health care communication in chronic illness. Patient Educ Couns. 2004;54(3):299–306. | ||
Skuladottir H, Halldorsdottir S. The quest for well-being: self-identified needs of women in chronic pain. Scand J Caring Sci. 2011;25(1):81–91. | ||
West C, Stewart L, Foster K, Usher K. The meaning of resilience to persons living with chronic pain: an interpretive qualitative inquiry. J Clin Nurs. 2012;21(9–10):1284–1292. | ||
Juuso P, Skär L, Olsson M, Söderberg S, et al. Living with a double burden: meanings of pain for women with fibromyalgia. Int J Qual Stud Health Wellbeing. 2011;6(3):7184. | ||
Sim J, Madden S. Illness experience in fibromyalgia syndrome: a metasynthesis of qualitative studies. Soc Sci Med. 2008;67(1):57–67. | ||
Mengshoel AM, Sim J, Ahlsen B, Madden S. Diagnostic experience of patients with fibromyalgia: a meta-ethnography. Chronic Illn. 2018;14(3)194–211. | ||
Briones-Vozmediano E, Vives-Cases C, Ronda-Pérez E, et al. Patients’ and professionals’ views on managing fibromyalgia. Pain Res Manag. 2013;18(1):19–24. | ||
Armentor JL. Living with a contested, stigmatized illness: experiences of managing relationships among women with fibromyalgia. Qual Health Res. 2017;27(4):462–473. | ||
Söderberg S, Lundman B, Norberg A. The meaning of fatigue and tiredness as narrated by women with fibromyalgia and healthy women. J Clin Nurs. 2002;11(2):247–255. | ||
Åsbring P. Chronic illness – a disruption in life: identity-transformation among women with chronic fatigue syndrome and fibromyalgia. J Adv Nurs. 2001;34(3):312–319. | ||
Söderberg S, Lundman B. Transitions experienced by women with fibromyalgia. Health Care Women Int. 2001;22(7):617–631. | ||
Devins G. Enhancing personal control and minimizing illness intrusiveness. In: Kutner N, Cardenas D, Bower J, editors. Maximizing Rehabilitation in Chronic Renal Disease. New York: PMA Publishing; 1989:109–136. | ||
Devins GM. Psychologically meaningful activity, illness intrusiveness, and quality of life in rheumatic diseases. Arthritis Rheum. 2006;55(2):172–174. | ||
Álvarez-Gallardo IC, Bidonde J, Busch A, et al. Therapeutic validity of exercise interventions in the management of fibromyalgia. J Sports Med Phys Fitness. Epub 2018 Oct 1. | ||
González E, Elorza J, Failde I. Comorbilidad psiquiátrica Y Fibromialgia. SU efecto sobre La calidad de vida de Los pacientes [Psychiatric comorbidity and Fibromyalgia and Its effect on the quality of life of patients]. Actas Esp Psiquiatr. 2010;38:295–300. Spanish. | ||
Assumpção A, Pagano T, Matsutani LA, Ferreira EA, Pereira CA, Marques AP. Quality of life and discriminating power of two questionnaires in fibromyalgia patients: fibromyalgia impact Questionnaire and medical outcomes study 36-Item short-form health survey. Rev Bras Fisioter. 2010;14(4):284–289. | ||
Carville SF, Arendt-Nielsen L, Bliddal H, et al; EULAR. EULAR evidence-based recommendations for the management of fibromyalgia syndrome. Ann Rheum Dis. 2008;67(4):536–541. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
