Back to Journals » Clinical Ophthalmology » Volume 14
Predictability of Residual Postoperative Astigmatism After Implantation of a Toric Intraocular Lens Using Two Different Calculators
Authors Pantanelli SM , Kansara N , Smits G
Received 9 August 2020
Accepted for publication 30 September 2020
Published 29 October 2020 Volume 2020:14 Pages 3627—3634
DOI https://doi.org/10.2147/OPTH.S276285
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Seth M Pantanelli,1 Neal Kansara,1 Gerard Smits2
1Department of Ophthalmology, Penn State College of Medicine, Hershey, PA, USA; 2Computer and Statistical Consultants Incorporated, Santa Barbara, CA, USA
Correspondence: Seth M Pantanelli
Department of Ophthalmology, Penn State College of Medicine, 500 University Drive; HU19, Hershey, PA 17033-0850, USA
Tel +1 717-531-5690
Fax +1 717-531-5009
Email [email protected]
Purpose: To compare predictability of postoperative refractive astigmatism (RA) using the Emmetropic Verifying Optical (EVO) Toric Formula v2.0 to one that accounts only for anterior corneal astigmatism.
Methods: This is a secondary analysis of de-identified data from a clinical trial including 9 sites across the United States. Preoperative biometry was used to predict postoperative RA with the implanted toric IOL using legacy enVista and EVO online calculators. The RA prediction error was computed between back-calculated postoperative RA and predicted residual RA. Outcome measures included vector (centroid) and arithmetic mean RA prediction error.
Results: Comparison of calculators was based on 109 eyes, 97 (89%) of which were implanted with a toric IOL with an effective astigmatism power of 1.4 D or less. Centroid of the RA prediction errors was 0.37 D @ 178 and 0.17 D @ 090 for the legacy and EVO calculators, respectively (p < 0.0001). The proportion of eyes with an absolute RA prediction error ≤ 0.5 was 47.3% and 49.1% (p = 0.78), while the proportion of eyes ≤ 1.0 D was 82.7% and 89.1% (p = 0.03). Differences in the proportions ≤ 0.5 D existed for WTR (p = 0.015) but not ATR (p = 0.75) eyes. The proportion in which orientation of the predicted RA (ATR, WTR, or oblique) matched the actual RA was 62% and 78% for legacy and EVO calculators, respectively (p = 0.0029).
Conclusion: The EVO Toric Formula v2.0 out-performed the legacy calculator with regards to predictions in eyes with low astigmatism.
Keywords: cataract, toric, intraocular lens power, astigmatism, calculators, EVO
Plain Language Summary
Cataract surgery involves removal of the cloudy lens from the eye and replacement with an artificial one. Surgeons choose the power of this artificial lens by taking measurements of the shape of the eye and entering them into a formula. When the lens power is chosen appropriately, it may reduce the need for glasses after surgery. The surgeon’s ability to correctly choose the power of this lens depends on accuracy of the measurements and the formula used.
Astigmatism is a defect in the curvature of the eye that results in distorted images. Toric intraocular lenses can be used to correct this. Historically, all of the astigmatism in an eye was assumed to come from the front surface of the eye. It is now understood that other internal interfaces also contribute to total astigmatism. This study sought to investigate the performance of two formulas used for lens power calculations, namely one that accounts for astigmatism measured at the very front of the eye and a second that accounts for additional internal contributors to total astigmatism.
Results from this study showed that using the new formula resulted in less prediction error than when the older formula was used. Using the new formula to estimate and correct patients’ astigmatism is likely to result in fewer patients needing glasses after cataract surgery. It is recommended that surgeons use a modern formula that takes into account all contributors to astigmatism when choosing the power of toric intraocular lenses.
Introduction
Nearly 40% of eyes have clinically significant astigmatism >0.5 D,1 and its correction has become a common goal of patients seeking spectacle independence after cataract surgery. The most effective treatment option is usually through use of a toric intraocular lens (IOL).2 For surgeons, the preoperative planning involves reliance upon various calculators for choosing the astigmatic power and axis of alignment of the toric IOL. Historically, these calculators relied upon the assumption that most refractive astigmatism came from the anterior cornea. Outcomes based on these assumptions were fair, with multiple authors reporting mean refractive astigmatism between 0.4 and 0.6 D and proportions with less than 0.5 D residual astigmatism between 50% and 70%.3,4
As our understanding of the contribution of astigmatism from the posterior cornea evolved,5 methods were developed to incorporate its effect. For example, the Baylor toric nomogram adjusts the measured keratometric astigmatism (KA) to account for the posterior corneal astigmatism (PCA) contribution.6 The Barrett toric calculator (BTC) is another popular formula that uses a proprietary algorithm to not only account for empirically derived PCA but also adjusts the toric power based on the estimated effective lens position (ELP).7 Several studies have demonstrated the superiority of the BTC over legacy methods that only account for KA. In one such study, Abulafia et al reported centroid errors of predicted astigmatism of ≈ 0.55 D when using two different legacy calculators, compared with only 0.02 D with the BTC.8
The enVista Toric Calculator (Bausch & Lomb, Bridgewater, NJ) is a proprietary legacy calculator based upon the vector addition of KA and surgically induced astigmatism (SIA). It does not take into account effective lens position (ELP) of the toric IOL when predicting postoperative residual astigmatism. On the other hand, the Emmetropic Verifying Optical (EVO) formula9 is a new thick lens formula that takes into account the optical dimensions of the eye and can handle different IOL geometries and powers. Its equivalence to the Barrett Universal II with regards to spherical equivalent (SE) outcomes has been recently validated in a large retrospective analysis of over 13,000 eyes.10 The EVO Toric Formula v2.0 adds astigmatism correction capability to the original EVO and combines theoretical posterior corneal astigmatism prediction with thick lens modeling for different types of toric IOLs. A recent study by Kane et al demonstrated near equivalence of the BTC and EVO Toric formulas,11 but the study made no comparisons to legacy calculators as a point of reference. The Kane study also only studied a single IOL [Alcon Acrysof Toric (SN6ATx)], and there are no studies evaluating the EVO Toric Formula v2.0 on other IOL platforms. For example, the lowest powered enVista toric IOL (MX60ET125, Bausch & Lomb) corrects approximately 0.9 D of astigmatism at the corneal plane, and steps up at different intervals than the Alcon Acrysof Toric IOL (SN6ATx); it is unclear whether a difference between legacy and EVO Toric calculators can still be appreciated when lower levels of astigmatism correction are sought. Thus, the purpose of this study was to investigate the relative predictability of residual refractive astigmatism (RA) using legacy enVista Toric12 and Emmetropic Verifying Optical (EVO)9 Toric Formula v2.0 IOL calculators.
Patients and Methods
This was a secondary analysis of de-identified data from a prospective multi-center clinical trial that was designed to evaluate the safety and effectiveness of a one-piece acrylic toric intraocular lens (enVista Toric MX60T, Bausch & Lomb, Bridgewater, NJ). The original study design as well as the description of pre-surgical and surgical technique have been previously published.13 Keratometric power measurements were taken using an automated optical biometer (IOLMaster, Carl Zeiss Meditec) and consistency and regularity of the astigmatism was confirmed using corneal topography. Visual acuities and refractions were tested at 4 m using the standard Early Treatment Diabetic Retinopathy Study chart at 85 cd/m2 illumination. All refractions were conducted using 0.25 D steps with a Jackson cross cylinder method for cylinder refinement. The dataset included 112 eyes from 112 subjects with predicted postoperative astigmatism between 0.90 and 2.40 D. During the study, investigators were required to use the legacy enVista toric calculator to calculate the recommended toric IOL cylinder power and axis and predicted postoperative RA. The primary incision was constructed along the steep keratometric axis, and surgery was completed using a 2.6 mm incision for non-wound assist, in-the-bag placement of the IOL. Actual axis of alignment and postoperative keratometry data were also available in addition to the manifest refraction. The original study was approved by a central Institutional Review Board (The IRB Company, Buena Park, CA); subsequent IRB approval was not required for the present study.
Pre- and postoperative keratometry data were entered into Warren Hill’s surgically induced astigmatism (SIA) Calculator,14 revealing a SIA vector mean (centroid) of 0.25 D @ 39 degrees for the study population. Using this magnitude, and the knowledge that the primary incision was placed along the steep axis, the predicted residual RA for the implanted IOL was calculated with the enVista legacy and EVO Toric Formula v2.0. To compensate for the fact that the two calculators’ recommended axis of alignment differed from the actual axis of alignment at the time of surgery, the residual RA predictions from these calculators were compared to theoretically back-calculated postoperative RAs adjusted using the “remove and replace” method previously described by Hill et al.15 Thus, the RA to which these calculator’s predictions were compared was based upon the vector sum of the actual postoperative RA and the difference between the actual and recommended toric IOL powers and orientations (Formula 1).
Back-calculated and predicted RA from the two calculators were converted to the spectacle plane. Residual astigmatism prediction error, defined as the difference between the back-calculated and predicted RAs, was calculated for each calculator (Formula 2).
This was done by converting all calculated and predicted RA vectors to Cartesian coordinates and subtracting corresponding x and y components, as previously described by Holladay.16 The paired x and y differences were then converted back to polar coordinates to create a clinically meaningful RA prediction error vector. Primary endpoints included the arithmetic and vector (centroid) means of the RA prediction error. Secondary endpoints included proportion of eyes with a RA prediction error magnitude less than 0.5, 0.75, or 1.0 diopters (D), and proportion of eyes in which the back-calculated RA matched the predicted RA with respect to astigmatism orientation [against-the rule (ATR), oblique, or with-the-rule (WTR)]. ATR astigmatism was defined as having KA oriented within 30 degrees of the 0–180 meridian, and WTR astigmatism was defined as having KA oriented within 30 degrees of 90.
Statistical analysis was performed using SAS Software v9.4 (SAS Institute Inc., Cary, NC). Differences between RA prediction error centroids were evaluated by splitting them into x- and y-components for each eye and comparing the paired differences between calculators using a Hotelling’s T-squared test.17 Comparison of the RA prediction error arithmetic mean magnitudes (without respect to axis) were made using a repeated measures ANOVA. The proportion of eyes with a RA prediction error magnitude less than 0.5, 0.75, or 1.0 D and proportion of eyes in which the astigmatism orientation from calculated and predicted RA matched were all compared using generalized estimating equation methodology.18 Results were considered significant at a p-value ≤ 0.05.
Results
The original dataset included 112 eyes from 112 patients. Three eyes were excluded based on a missing anterior chamber depth (1) or postoperative refraction (2), resulting in 109 eyes available for analysis. The demographics for these eyes are displayed in Table 1. The magnitude of KA was not normally distributed, but instead was concentrated towards lower magnitudes, as would be expected in any random sampling of eyes from the population. The orientation of the preoperative KA was as follows: 67 (61.5%) ATR, 38 (34.9%) WTR, and 4 (3.7%) oblique. Of eyes that received a toric IOL, 79 (72.5%) received a MX60T125, 18 (16.5%) received an MX60T200, and 12 (11%) received a MX60T275. These lenses have cylinder powers of 1.25, 2.0 and 2.75 D at the IOL plane and contribute approximately 0.9, 1.40, and 1.93 D of astigmatism correction at the corneal plane, respectively.
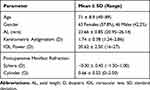 |
Table 1 Demographics |
The RA prediction error arithmetic mean magnitudes and centroids for the calculators are displayed in Table 2 and Figure 1. When the entire sample was considered, the RA prediction error arithmetic mean magnitude was lower for the EVO calculator, but this difference did not reach significance (p = 0.10). However, the RA prediction error centroid for EVO was lower than that of the legacy calculator (p ≤ 0.0001). The RA prediction error centroid was oriented ATR with the legacy calculator and WTR for EVO. The proportion of eyes that had an arithmetic RA prediction error magnitude less than or equal to 0.5, 0.75, and 1.0 D are displayed in Figure 2. The EVO had improved proportions within target at all three cut-offs, but this difference was only significant for the proportion within 1.0 D (p = 0.03) when the entire dataset was considered. The proportion of eyes in which the orientation of the predicted RA (ATR, WTR, or oblique) matched the actual RA was 62% and 78% for the legacy and EVO calculators, respectively (p = 0.0029).
 |
Table 2 Residual Astigmatism Prediction Errors (Arithmetic and Centroid) by Method of Calculation (n=109) |
 |
Figure 1 Residual astigmatism prediction error centroid magnitude by method of calculation. |
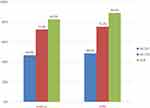 |
Figure 2 Proportion of eyes with arithmetic residual astigmatism prediction error within 0.5, 0.75, and 1.00 diopters (D). |
Table 3 displays the RA prediction error arithmetic means and centroids for the ATR (n = 67) and WTR (n = 38) sub-groups. Double angle plots of the RA prediction error for each eye are also displayed in Figure 3. RA prediction error arithmetic means for the legacy calculator were higher in WTR than ATR eyes, and this difference approached statistical significance (p = 0.08). Conversely, the arithmetic means for the two different subgroups were similar with the EVO calculator (p = 0.55). The legacy toric calculator produced RA prediction error centroids oriented ATR for both sub-groups, while EVO’s was oriented WTR. The RA prediction error centroid for the legacy calculator was higher in WTR than in ATR eyes (p = 0.0061), but this was not the case for the EVO calculator (p = 0.596). Comparing sub-groups across methods, the RA prediction error centroid for the legacy calculator was higher in both WTR (p < 0.0001) and ATR (p < 0.0001) eyes than with EVO.
 |
Table 3 Residual Astigmatism Prediction Errors by Method of Calculation in Eyes with Against- and with-the-Rule Astigmatism |
Table 4 displays the RA prediction error for the two calculators, stratified by the toricity of the IOL implanted. Irrespective of toricity, the EVO calculator produced smaller RA prediction error centroids than the legacy calculator. This difference was significant in all three IOL groups (x-component p< 0.0001). Interestingly, there was a trend toward smaller standard deviations as the toricity of the IOL increased, regardless of the calculator used.
 |
Table 4 Residual Astigmatism Prediction Errors by Method of Calculation and Intraocular Lens Toricity |
Discussion
As our understanding of contributions to corneal astigmatism has increased, so has the number of toric nomograms and calculators available. This complicates the choice for surgeons of which work best. By examining precisely which concepts are incorporated into each, we come away with a greater appreciation for why some calculators perform better than others. This increased understanding may also give surgeons the confidence to move from a calculator of habit to one that incorporates the newest concepts and improves results.
The enVista toric calculator, like the Acrysof iQ Toric (Alcon, Fort Worth, TX) and original Holladay Toric Calculators, may be considered a legacy calculator as total ocular astigmatism is calculated from anterior keratometry and SIA only. Furthermore, the legacy calculators make no determination on the relationship between effective lens position and effective astigmatism from the toric IOL at the cornea plane. It is thus not surprising that the present study found that the enVista toric calculator resulted in a relatively high RA prediction error centroid magnitude, and that this centroid had an ATR orientation (0.37 @ 179). Note that the RA prediction error vector in the present study is consistent with previously published work from Abulafia et al (0.55 @ 180) on similar legacy calculators.8,19 The higher RA prediction error vector magnitude and ATR orientation associated with these legacy calculators stem from the now well-established contribution of the posterior cornea. The posterior cornea is known to have its steep axis of curvature oriented vertically in 85–90% of cases, resulting in an optical contribution of ≈ 0.3 D oriented horizontally.5
The findings in the present study suggest that the EVO Toric Formula v2.0, which incorporates an empirically estimated posterior corneal astigmatism and effective lens position, performs better than the enVista legacy calculator, which relies only upon anterior corneal astigmatism. Comparison of these two calculators has not been previously reported, yet the results are not entirely surprising, and are consistent with findings in the existing literature. For example, a recent study by Kane et al comparing 6 different modern calculators found that the Barrett and EVO Toric Formulas were nearly equivalent, with 59.9% and 58.9% of eyes, respectively, having a RA prediction error ≤0.5 D.11 Similar to the RA prediction error centroid reported in the present work (0.17 ± 0.67 D x 090), Kane also reported RA prediction error centroids for the Barrett and EVO Formulas of 0.10 ± 0.64 D x 111 and 0.16 ± 0.63 D x 100.11 We thus now have evidence that the EVO Toric Formula v2.0 is not only superior to legacy formulas but is also equivalent to many of the modern toric calculators of present.
It is worth noting that 90% of the eyes in the present study were implanted with a toric IOL with an effective astigmatism power of 1.4 D or less, and no eye had keratometric astigmatism magnitude greater than 2.8 D. This is a dataset with particularly low astigmatism magnitude. Furthermore, nearly 2/3 of these eyes had preoperative ATR keratometric astigmatism. We know from the results of the present work and others that the performance of modern calculators is best highlighted in eyes with higher-magnitudes, and in those with WTR rather than ATR astigmatism.6 For example, the “Net Astigmatism” predictions from legacy and modern toric calculators might differ by only 0.3 D in an eye with 1 D of ATR astigmatism, but 1.25 D or more in an eye with 4.0 D of WTR astigmatism. In short, the performance of the EVO Toric Formula v2.0 in eyes with low astigmatism is good and better than that of legacy calculators, but one might expect these differences to be further highlighted in a population that includes higher astigmatism, and a greater proportion with WTR astigmatism.
As mentioned in the results, one additional finding was the trend toward smaller standard deviations in the RA prediction error with increasing IOL toricity. We hypothesize that this is due to the increased variability in axis determination on behalf of the biometer and the investigator performing postoperative manifest refractions when the astigmatism magnitude is low. For example, an optical biometer might register the axis of astigmatism to within 15 degrees when the magnitude is 1.0 D, but would likely register the same to within 5 degrees when the magnitude is 5.0 D. A commonly held belief among surgeons is that increases in prediction error with increasing magnitudes of astigmatism are due to the fact that axial misalignments with IOLs containing higher toricities cause proportionately higher refractive errors. However, in the present study, it is interesting to note that there was no significant increase in the RA prediction error with increasing toricity of the IOL.
The present study has several strengths, which include a relatively large sample size (109 versus 61,19 62,20 and 4621) compared to many published works in this domain. It also includes only one eye from each subject (avoiding paired organ biases) and is also the first study to report upon performance of the EVO Toric Formula v2.0 on an IOL platform other than the Acrysof IQ (Alcon, Fort Worth, TX). On the other hand, limitations of the present work include the relatively high standard deviation of the RA prediction error vector (≈ 0.66 D) in the present study compared to that reported in some other works (≈ 0.33 D).19 This might be due to variability in surgical technique, axis measurements in eyes with lower magnitudes of astigmatism, and manifest refractions, since the dataset used here came from a multi-center clinical trial. Other works report on outcomes from a single surgeon and include a larger number of eyes with greater keratometric astigmatism. Analysis of data in the present work involved using Hill’s “remove and replace” method,15 which does not take into account ELP of the toric IOL. This may have resulted in an under-representation of the EVO Toric Formula v2.0 performance, which takes into account ELP. Other limitations of this study include the absence of lens thickness (optional factor for both BTC and EVO) and the fact that the dataset included lower-powered torics only. As discussed above, evaluation with a dataset that includes higher-powered torics would have likely further differentiated EVO’s performance from that of the legacy calculator. While the methodology for retrospective analysis of toric outcomes has been well established, a prospective comparative case series would be the best test of these calculators’ relative performance.
Funding
Public and Private Support: Author S.M.P. received remuneration from Bausch & Lomb for data analysis and manuscript preparation related to the present study.
Disclosure
Author S.M.P. serves as an advisory board member, consultant, and Medical Monitor for Carl Zeiss Meditec, and as a consultant for Bausch & Lomb, and reports personal fees from Bausch & Lomb, during the conduct of the study, and personal fees from Carl Zeiss Meditec, outside the submitted work. Author G.S. serves as a consultant for both Carl Zeiss Meditec and Bausch & Lomb, outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
1. Ferrer-Blasco T, Montes-Mico R, Peixoto-de-Matos SC, Gonzalez-Meijome JM, Cervino A. Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35(1):70–75. doi:10.1016/j.jcrs.2008.09.027
2. Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016;123(2):275–286. doi:10.1016/j.ophtha.2015.10.002
3. Ahmed II, Rocha G, Slomovic AR, et al. Visual function and patient experience after bilateral implantation of toric intraocular lenses. J Cataract Refract Surg. 2010;36(4):609–616. doi:10.1016/j.jcrs.2009.10.044
4. Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM. The AcrySof toric intraocular lens in subjects with cataracts and corneal astigmatism: a randomized, subject-masked, parallel-group, 1-year study. Ophthalmology. 2010;117(11):2104–2111. doi:10.1016/j.ophtha.2010.07.033
5. Koch DD, Ali SF, Weikert MP, Shirayama M, Jenkins R, Wang L. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38(12):2080–2087. doi:10.1016/j.jcrs.2012.08.036
6. Koch DD, Jenkins RB, Weikert MP, Yeu E, Wang L. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. J Cataract Refract Surg. 2013;39(12):1803–1809. doi:10.1016/j.jcrs.2013.06.027
7. Barrett G. Barrett toric calculator. Available from: https://ascrs.org/tools/barrett-toric-calculator.
8. Abulafia A, Hill WE, Franchina M, Barrett GD. Comparison of methods to predict residual astigmatism after intraocular lens implantation. J Refract Surg. 2015;31(10):699–707. doi:10.3928/1081597X-20150928-03
9. Yeo T-K. Emmetropic verifying optical (EVO) formula. Available from: http://www.evoiolcalculator.com.
10. Melles RB, Kane JX, Olsen T, Chang WJ. Update on intraocular lens calculation formulas. Ophthalmology. 2019;126(9):1334–1335. doi:10.1016/j.ophtha.2019.04.011
11. Kane JX, Connell B. A comparison of the accuracy of 6 modern toric intraocular lens formulas. Ophthalmology. 2020.
12. Lomb B. enVista toric calculator. Available from: http://envista.toriccalculator.com.
13. Packer M, Williams JI, Feinerman G, Hope RS. Prospective multicenter clinical trial to evaluate the safety and effectiveness of a new glistening-free one-piece acrylic toric intraocular lens. Clin Ophthalmol. 2018;12:1031–1039. doi:10.2147/OPTH.S167726
14. Hill W. SIA calculator. Available from: http://www.sia-calculator.com/.
15. Hill W, Osher R, Cooke D, et al. Simulation of toric intraocular lens results: manual keratometry versus dual-zone automated keratometry from an integrated biometer. J Cataract Refract Surg. 2011;37(12):2181–2187. doi:10.1016/j.jcrs.2011.06.028
16. Holladay JT, Moran JR, Kezirian GM. Analysis of aggregate surgically induced refractive change, prediction error, and intraocular astigmatism. J Cataract Refract Surg. 2001;27(1):61–79. doi:10.1016/S0886-3350(00)00796-3
17. Naeser K. Assessment and statistics of surgically induced astigmatism. Acta Ophthalmol. 2008;86(3):349. doi:10.1111/j.1755-3768.2008.01287.x
18. Agresti A. An Introduction to Categorical Data Analysis.
19. Abulafia A, Koch DD, Wang L, et al. New regression formula for toric intraocular lens calculations. J Cataract Refract Surg. 2016;42(5):663–671. doi:10.1016/j.jcrs.2016.02.038
20. Savini G, Naeser K, Schiano-Lomoriello D, Ducoli P. Optimized keratometry and total corneal astigmatism for toric intraocular lens calculation. J Cataract Refract Surg. 2017;43(9):1140–1148. doi:10.1016/j.jcrs.2017.06.040
21. Yeu E, Cheung AY, Potvin R. Clinical outcomes of toric intraocular lenses: differences in expected outcomes when using a calculator that considers effective lens position and the posterior cornea vs one that does not. Clin Ophthalmol. 2020;14:815–822. doi:10.2147/OPTH.S247800
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

