Back to Journals » Risk Management and Healthcare Policy » Volume 13
Potential Impacts of Meteorological Variables on Acute Ischemic Stroke Onset
Authors Qi X, Wang Z, Xia X, Xue J, Gu Y, Han S, Wang L, Li X , Leng SX
Received 12 March 2020
Accepted for publication 27 May 2020
Published 19 June 2020 Volume 2020:13 Pages 615—621
DOI https://doi.org/10.2147/RMHP.S253559
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Xuemei Qi,1 Zhongyan Wang,2 Xiaoshuang Xia,1 Juanjuan Xue,1 Yumeng Gu,1 Suqin Han,3 Lin Wang,2 Xin Li,1,* Sean X Leng4,*
1Department of Neurology, The Second Hospital of Tianjin Medical University, Tianjin, People’s Republic of China; 2Department of Geriatrics, The Second Hospital of Tianjin Medical University, Tianjin, People’s Republic of China; 3Tianjin Environmental Meteorology Center, Tianjin 300074, People’s Republic of China; 4Division of Geriatric Medicine and Gerontology, School of Medicine, Johns Hopkins University, Baltimore, MD, USA
*These authors contributed equally to this work
Correspondence: Xin Li
Department of Neurology, The Second Hospital of Tianjin Medical University, No. 23, PingJiang Road, Tianjin 300211, People’s Republic of China
Tel +86 22 8832 8514
Fax +86 22 2830 9286
Email [email protected]
Sean X Leng
Division of Geriatric Medicine and Gerontology, Johns Hopkins University School of Medicine, 5501 Hopkins Bayview Circle, Baltimore, MD 21224, USA
Tel/ Fax +1 41 0550 2494
Email [email protected]
Purpose: The effects of meteorological parameters on stroke occurrence remain debated. The aim of the study was to assess the association between meteorological parameters and ischemic stroke onset in cold seasons in Tianjin.
Patients and Methods: Patients with acute ischemic stroke (946) were identified by standard sampling from one stroke unit in the Second Hospital of Tianjin Medical University, Tianjin, China, from 10/1/2014 to 4/30/2019. Generalized linear Poisson regression models were used to explore the effect of meteorological parameters (air temperature, barometric pressure, and relative humidity) on daily ischemic stroke onset after adjusting for air pollutants, day of week, and public holiday.
Results: The results showed that ischemic stroke onset was positively associated with the diurnal variation of temperature (β coefficient: 0.020, 95% CI [0.001, 0.038] p< 0.05). Significant positive correlation between ischemic stroke onset and barometric pressure (mean, minimum) was found (β coefficient: 0.010, 95% CI [0.001,0.019] p< 0.05; 0.010, 95% CI [0.001,0.019] p< 0.05). The subgroup analysis considering age and gender difference showed that the older and the female were more vulnerable to weather conditions.
Conclusion: Our study demonstrated that there was a measurable effect of weather parameters on daily ischemic stroke onset in colder seasons, suggesting that meteorological variables may, at least in part, play as risk factors for ischemic stroke onset, especially for the aging and female population.
Keywords: cold temperature, air pressure, ischemic stroke
Introduction
Stroke has been the leading cause of disability and mortality worldwide and posing heavy medical and economic burdens in many countries including China.1,2 Studies showed that there were regional differences in stroke incidence in China and the highest morbidity was recorded in northern China, including Tianjin.3 So more work should be done for better prevention and management of stroke in Tianjin. It is well established that some traditional cerebrovascular risk factors, such as hypertension, high cholesterol level, tobacco use, alcohol use and obesity, increased stroke risk.4,5 Changes in external stimuli may help explain why stroke is more likely to occur in particular regions at particular times.1 And there is an increasing concern regarding environmental factors such as temperature, barometric pressure, and humidity on stroke occurrence.
The associations between meteorological variables and stroke onset have been examined widely. Both immediate and delayed effects of weather conditions on stroke occurrence were revealed.6–9 However, existing studies often reported discordant effects of these meteorological parameters on ischemic stroke occurrence. For example, conclusions on the temperature and barometric pressure were inconsistent. Some studies showed high values resulted in a higher risk of ischemic stroke,10,11 some concluded no associations between these weather conditions and ischemic stroke morbidity,8,12,13 whereas some others revealed that low values resulted in higher risk of ischemic stroke.6,9,14 So the relationship between meteorological parameters and stroke is still confusing and controversial. Most of the previous studies explored the association between meteorological variables and ischemic stroke admission instead of the stroke onset time, which would lead to misclassification of time and influence the estimates of adverse effects for meteorological variables. More efforts should be made to enhance a better understanding of the relationship between weather conditions and stroke onset, which may provide new insights into the health effects of meteorological variables and help make public health strategies to avoid hazards induced by adverse environmental conditions. In the clinical work, we found that hospital admissions of ischemic stroke were larger during cold seasons in Tianjin. So the main goal of our study was to explore the association between meteorological variables and acute ischemic stroke onset in cold seasons of Tianjin.
Patients and Methods
Clinical Data
The study population was the patients admitted to the stroke unit of the Second Hospital of Tianjin Medical University (Tianjin, China) with an admission diagnosis of ischemic stroke (ICD code I63) during cold seasons between October 1, 2014 and April 30, 2019 (n=1056). Patients who presented acute neurological deficits due to a vascular cause were admitted in the hospital and brain imaging of either MRI or CT was performed after admission (in most cases within 24 h) on all patients with the clinical diagnosis of stroke. The stroke onset time was reported by the patients and/or caregivers. 110 patients were excluded because of incomplete clinical data. 946 patients with acute cerebral infarction were included in the analysis. Clinical data (smoking, alcohol drinking, presence of risk factor history including stroke history, hypertension, diabetes mellitus, hyperlipidemia, hyperhomocysteinemia, atrial fibrillation, coronary artery disease, lung diseases, and infectious diseases), high-sensitivity c-reactive protein (hsCRP) level and National Institutes of Health Stroke Scale (NIHSS) score at admission from each patient were reviewed and verified by a neurologist before being recorded on a computer database. No protected health information was collected as data.
Meteorological Observations
Tianjin is located in northern China and has clearly four seasons, with a cold, windy, dry winter and a hot, humid summer. Meteorological data were obtained from the database of Tianjin Meteorological Bureau using a weather station providing data representative of the urban area in Tianjin. Observations were from the Tianjin Urban Climate Monitoring Station with an altitude of 2.2m, located in 11712E, 3904N. Meteorological data were collected over 1184 days, from September 28, 2014, to April 30, 2019, which was selected based on the colder temperature and variations of barometric meteorological variables in the area of Tianjin. Meteorological variables included daily measurements of temperature (T) (mean, maximum, minimum, diurnal variation), barometric pressure (mean, maximum, minimum, diurnal variation), and relative humidity (RH). The concentration of air pollutants also has an impact on the onset of cerebrovascular disease and was adjusted as a confounding factor for meteorological variables in previous studies.15,16 Here we used air quantity index (AQI) as a measure of air quality, which was calculated by the concentration of PM2.5, PM10, SO2, NO2, O3, and CO.
Statistical Analysis
Continuous variables were described with mean ± standard deviation (SD) or median and interquartile range (IQR). Categorical variables were presented as numbers and percentages. In the study period of 1181 days, the maximum number of ischemic strokes on a single day was 7. Daily numbers of ischemic stroke onset were modeled using generalized linear Poisson regression models to study the association between stroke onset and meteorological variables including air temperature (mean, maximum, minimum, diurnal variation), barometric pressure (mean, maximum, minimum, diurnal variation), and relative humidity.6,9,14 Each meteorological variable was modeled separately after adjusting for day of week, public holiday (binary variable) and AQI, removing the confounding effect of those factors on stroke onset. Modeling was also repeated in the subgroup analysis (<75 years vs. ≥75years; male vs. female). Values with a two-tailed significance level less than 0.05 were considered as statistically significant and the corresponding 95% confidence interval (CI) was used to describe the effect estimates. All analysis was performed by SPSS 25.0 statistic software (SPSS Inc., Chicago, IL, USA).
Results
Baseline Characteristics of Study Subjects
The baseline characteristics are described in Table 1. A total of 946 patients were enrolled in the study, composed of 558 (59.0%) male patients and 388 (41.0%) female patients. The mean age was 70.4±11.6 years old, and there were 553 (58.5%) patients <75 years old and 393 (41.5%) patients ≥75 years old. There were 343 (36.3%) patients with smoking and 208 (22.0%) with alcohol drinking. Among those patients there were 882 (93.2%) with the following medical history (stroke history [336, 35.5%], hypertension [659, 69.7%], diabetes mellitus [305, 32.2%], hyperlipidemia [220, 23.3%], hyperhomocysteinemia [364, 38.5%], atrial fibrillation [115, 12.2%], coronary artery disease [300, 31.7%], lung diseases, [109, 11.5%], infectious diseases [120, 12.7%]). HsCRP level at admission was 3.2 (IQR, 1.4–8.1) mg/L. NIHSS score was 3 (IQR, 2–6).
 |
Table 1 Baseline Characteristics of Study Subjects |
Description of Meteorological Variables
Days from October to April were the cold period with increased meteorological factors variation in Tianjin, China. The meteorological measurements are shown in Table 2. The daily mean, minimum, maximum temperature, and diurnal variation in Tianjin was 7.2±7.4 (°C), 3.1±6.8 (°C), 11.6±8.3 (°C) and 8.6±3.6 (°C) respectively. The daily mean minimum, maximum barometric pressure and diurnal variation was 1023.0±7.5 (hPa), 1020.1±7.8 (hPa), 1026.1±7.4 (hPa) and 6.1±2.9 (hPa) respectively. The daily mean relative humidity was 44.1±18.4 (%). There was a statistically significant association between daily mean barometric pressure and mean air temperature. Increased temperature was related to decreased air pressure (R = −0.765; P < 0.01) and increased relative humidity (R = 0.120; P < 0.01). And increased air pressure was related to decreased relative humidity (R = −0.176; P < 0.01).
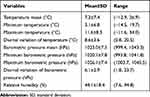 |
Table 2 Descriptive Statistics of Meteorological Variables |
Associations Between Meteorological Variables and Ischemic Stroke Onset
The diurnal variation of temperature was positively associated with ischemic stroke onset. Every 1°C increase in the diurnal variation of temperature was associated with a 0.020 ([95% CI: 0.001, 0.038], p<0.05) increase in ischemic stroke onset. The mean, minimum, and maximum temperature was negatively associated with ischemic stroke onset, but showed no statistical significance. There was a positive association between barometric pressure (mean, minimum, maximum, diurnal variation of barometric) and ischemic stroke onset, in which only the mean, minimum, maximum barometric pressure reached statistically significant. And 1hPa increase in mean barometric pressure was related to 0.010 ([95% CI: 0.001, 0.019], p<0.05) increase in ischemic stroke onset. There was no statistically significant association between relative humidity and ischemic stroke onset (Table 3).
 |
Table 3 Association Analysis Between the Meteorological Variables and Ischemic Stroke Hospitalization |
Table 3 also showed that the associations between meteorological variables and ischemic stroke onset varied by gender and age. Diurnal variation of temperature and barometric pressure and mean, minimum, maximum barometric pressure showed greater statistical association with ischemic stroke onset in female patients, however, showed no statistical association in male patients. For a 1°C increase in diurnal variation of temperature, we observed a significant increase of daily ischemic stroke onset 0.041 ([95% CI: 0.012, 0.069]; p<0.01) in female patients compared with 0.005 ([95% CI: −0.019, 0.029]; p>0.05) in male patients. Mean, minimum, maximum barometric pressure, and diurnal variation of barometric pressure also showed greater statistical association with ischemic stroke onset in female patients. Diurnal variation of temperature and mean, minimum barometric pressure and diurnal variation of barometric pressure also showed better statistical association with ischemic stroke onset in patients≥75 years old (diurnal variation of temperature: 0.016 [95% CI: 0.005, 0.028], p<0.05; mean barometric pressure: 0.012 [95% CI: 0.003, 0.020], p<0.05; minimum barometric pressure: 0.014 [95% CI: 0.001, 0.027], p<0.05; diurnal variation of barometric pressure: 0.017 [95% CI: 0.004, 0.027], p<0.05), but there were no significant associations in the patients<75 years old.
The estimation of potential delayed effects of mean temperature on ischemic stroke onset is summarized in Table 4. Mean temperature of the day before stroke onset time was negatively associated with stroke onset and the association of mean temperature two days before stroke onset showed statistical significance among all patients and remained significant among the female and the elderly in the subgroup analysis.
 |
Table 4 Delayed Effect of Mean Temperature on Ischemic Stroke Hospitalization |
Discussion
In this study, we found that short-term exposure to higher diurnal variation of temperature and barometric pressure and higher biometric pressure in cold seasons was associated with increased cerebral infarction onset in Tianjin after adjusting for day of week, public holiday and air pollutants. In subgroup analysis, the associations were more evident in the elderly and the female, but did not reach statistically significant in male patients and those less than 75 years old.
In previous studies, meteorological factors, such as temperature, barometric pressure were linked to altered incidence of cerebrovascular disease, but findings have been inconsistent. The differences lie in whether it is positively related, negatively related, or unrelated and exist in the effect of a unit change of meteorological values.8,12,17–19 And most of these studies investigated the effects of meteorological variables based on stroke hospitalization instead of stroke onset time. In our present study, we analyzed data in cold seasons and found that the increased diurnal variation of temperature and barometric pressure and higher biometric pressure were related to increased ischemic stroke onset in urban Tianjin, and the trend was in line with the findings of some previous studies.10,13,14,20–22 People may have difficulties with thermoregulation when the changes in temperature are sudden and dramatic.23 Temperature changes could influence blood pressure, cholesterol level, inflammatory response, and immune function, which may trigger cerebrovascular disease.17 Barometric pressure may directly influence vessel walls by triggering endogenous inflammatory and changing endothelial function,9,24,25 and may also contribute to plaque rupture by exerting stress on atherosclerotic plaques.26 On the contrary, some previous studies found that decreased air pressure was associated with ischemic stroke hospitalization.6,9,11 So the underlying mechanism remains obscure, and needs further researches. Moreover, in our study we mainly explored the effect of weather conditions on stroke onset in cold seasons, which was different from these studies that analyzed data all year round and based on stroke admission time.
It is reported that there is a delayed effect of ambient temperature on stroke incidence,9,11,20 and a potential delayed (2 days) effect of daily mean temperature on ischemic stroke onset was also observed in the study. Studies also found that relative humidity can predict stroke admission.9,17,21 However, our results showed no statistical association between relative humidity and ischemic stroke onset. The pathogenic complexity of ischemic stroke should be considered when interpreting the results, since it may underrepresent the effects of these meteorological factors. The inconsistency may also result from different characteristics of various studies, such as different population susceptibility, climates and geographical region, study design, study period, statistical methods, and different confounding factors.
The subgroup analysis demonstrated that the elderly have a higher risk of ischemic stroke during days with higher temperature and barometric air pressure variation and days with higher barometric air pressure compared with the younger group, which could be explained by the declining thermoregulatory function and the higher prevalence of chronic health conditions in aging adults.27 The results concerning gender differences showed that the female group was more vulnerable to meteorological factors probably due to the gender differences in hormones and thermoregulatory function.28 Men were more susceptible to high temperatures, but in cold seasons women had a higher risk of cerebrovascular events than men.22,29 High levels of estrogen in women can increase expression of alpha2C-adrenoceptors in smooth muscle cells which may contribute to the blood pressure changes related to meteorological factors.30
This study has several strengths. We analyzed the clinical data over a multi-year span and provided comprehensive estimates after adjusting for several confounding factors. Besides, the estimates were based on stroke onset time instead of the admission time, which avoided some misclassification of time. However, there are still some limitations in the study. Firstly, the small sample size with 946 patients could weaken the power to evaluate the influences of meteorological variables on ischemic stroke onset. A larger multicenter study including more patients would better explain the association between weather factors and ischemic stroke onset. Secondly, the measure of temperature in the study was outdoor temperature, which may be not corresponding to the temperature that the individual was exposed to. Thirdly, although we adjusted air pollution, day of week, and public holiday in the analysis, some other potential confounding factors may not be addressed.
Conclusion
There are few studies on the relationship between meteorological factors and ischemic stroke onset. Our results suggest that higher variation of temperature and barometric pressure as well as higher barometric pressure can be used to predict the acute ischemic stroke onset in cold seasons thus evaluate the workload change of a hospital. The elderly and female people are more vulnerable to external meteorological factors. The clinical bases of these observations merit further investigation.
Data Sharing Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Acknowledgments
This work was supported by Major Social Science Program of Tianjin Municipal Education Commission (2017JWZD36) and Key Technology Research and Development Program of Science & Technology of Tianjin (18ZXDBSY00210).
Author Contributions
Sean X. Leng and Xin Li are the co-corresponding authors. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res. 2017;120(3):439–448. doi:10.1161/circresaha.116.308413
2. Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: results from a nationwide population-based survey of 480 687 adults. Circulation. 2017;135(8):759–771. doi:10.1161/circulationaha.116.025250
3. Jia Q, Liu LP, Wang YJ. Stroke in China. Clin Exp Pharmacol Physiol. 2010;37(2):259–264. doi:10.1111/j.1440-1681.2009.05290.x
4. Grysiewicz RA, Thomas K, Pandey DK. Epidemiology of ischemic and hemorrhagic stroke: incidence, prevalence, mortality, and risk factors. Neurol Clin. 2008;26(4):871–895, vii. doi:10.1016/j.ncl.2008.07.003
5. Poorthuis MH, Algra AM, Algra A, Kappelle LJ, Klijn CJ. Female- and male-specific risk factors for stroke: a systematic review and meta-analysis. JAMA Neurol. 2017;74(1):75–81. doi:10.1001/jamaneurol.2016.3482
6. Morabito M, Crisci A, Vallorani R, Modesti PA, Gensini GF, Orlandini S. Innovative approaches helpful to enhance knowledge on weather-related stroke events over a wide geographical area and a large population. Stroke. 2011;42(3):593–600. doi:10.1161/strokeaha.110.602037
7. Basu R, Pearson D, Malig B, Broadwin R, Green R. The effect of high ambient temperature on emergency room visits. Epidemiology. 2012;23(6):813–820. doi:10.1097/EDE.0b013e31826b7f97
8. Ma P, Zhou J, Wang S, et al. Differences of hemorrhagic and ischemic strokes in age spectra and responses to climatic thermal conditions. Sci Total Environ. 2018;644:1573–1579. doi:10.1016/j.scitotenv.2018.07.080
9. Guan W, Clay SJ, Sloan GJ, Pretlow LG. Effects of barometric pressure and temperature on acute ischemic stroke hospitalization in Augusta, GA. Transl Stroke Res. 2018. doi:10.1007/s12975-018-0640-0
10. Lee HC, Hu CJ, Chen CS, Lin HC. Seasonal variation in ischemic stroke incidence and association with climate: a six-year population-based study. Chronobiol Int. 2008;25(6):938–949. doi:10.1080/07420520802551469
11. Dawson J, Weir C, Wright F, et al. Associations between meteorological variables and acute stroke hospital admissions in the west of Scotland. Acta Neurol Scand. 2008;117(2):85–89. doi:10.1111/j.1600-0404.2007.00916.x
12. Cowperthwaite MC, Burnett MG. An analysis of admissions from 155 United States hospitals to determine the influence of weather on stroke incidence. J Clin Neurosci. 2011;18(5):618–623. doi:10.1016/j.jocn.2010.08.035
13. Magalhaes R, Silva MC, Correia M, Bailey T. Are stroke occurrence and outcome related to weather parameters? Results from a population-based study in northern Portugal. Cerebrovasc Dis. 2011;32(6):542–551. doi:10.1159/000331473
14. Hori A, Hashizume M, Tsuda Y, Tsukahara T, Nomiyama T. Effects of weather variability and air pollutants on emergency admissions for cardiovascular and cerebrovascular diseases. Int J Environ Health Res. 2012;22(5):416–430. doi:10.1080/09603123.2011.650155
15. Chung JW, Bang OY, Ahn K, et al. Air pollution is associated with ischemic stroke via cardiogenic embolism. Stroke. 2017;48(1):17–23. doi:10.1161/strokeaha.116.015428
16. Tian Y, Liu H, Zhao Z, et al. Association between ambient air pollution and daily hospital admissions for ischemic stroke: a nationwide time-series analysis. PLoS Med. 2018;15(10):e1002668. doi:10.1371/journal.pmed.1002668
17. Tian Y, Liu H, Si Y, et al. Association between temperature variability and daily hospital admissions for cause-specific cardiovascular disease in urban China: a national time-series study. PLoS Med. 2019;16(1):e1002738. doi:10.1371/journal.pmed.1002738
18. Cevik Y, Dogan NO, Das M, Ahmedali A, Kul S, Bayram H. The association between weather conditions and stroke admissions in Turkey. Int J Biometeorol. 2015;59(7):899–905. doi:10.1007/s00484-014-0890-9
19. Giua A, Abbas MA, Murgia N, Corea F. Climate and stroke: a controversial association. Int J Biometeorol. 2010;54(1):1–3. doi:10.1007/s00484-009-0253-0
20. Mostofsky E, Wilker EH, Schwartz J, et al. Short-term changes in ambient temperature and risk of ischemic stroke. Cerebrovasc Dis Extra. 2014;4(1):9–18. doi:10.1159/000357352
21. Cao Y, Wang X, Zheng D, et al. Air pressure, humidity and stroke occurrence: a systematic review and meta-analysis. Int J Environ Res Public Health. 2016;13(7):675. doi:10.3390/ijerph13070675
22. Tamasauskiene L, Rastenyte D, Radisauskas R, et al. Relationship of meteorological factors and acute stroke events in Kaunas (Lithuania) in 2000–2010. Environ Sci Pollut Res Int. 2017;24(10):9286–9293. doi:10.1007/s11356-017-8590-8
23. Martinez-Nicolas A, Meyer M, Hunkler S, et al. Daytime variation in ambient temperature affects skin temperatures and blood pressure: ambulatory winter/summer comparison in healthy young women. Physiol Behav. 2015;149:203–211. doi:10.1016/j.physbeh.2015.06.014
24. Jimenez-Conde J, Ois A, Gomis M, et al. Weather as a trigger of stroke. Daily meteorological factors and incidence of stroke subtypes. Cerebrovasc Dis. 2008;26(4):348–354. doi:10.1159/000151637
25. Buxton N, Liu C, Dasic D, Moody P, Hope DT. Relationship of aneurysmal subarachnoid hemorrhage to changes in atmospheric pressure: results of a prospective study. J Neurosurg. 2001;95(3):391–392. doi:10.3171/jns.2001.95.3.0391
26. Houck PD, Lethen JE, Riggs MW, Gantt DS, Dehmer GJ. Relation of atmospheric pressure changes and the occurrences of acute myocardial infarction and stroke. Am J Cardiol. 2005;96(1):45–51. doi:10.1016/j.amjcard.2005.02.042
27. Gronlund CJ, Sullivan KP, Kefelegn Y, Cameron L, O’Neill MS. Climate change and temperature extremes: a review of heat- and cold-related morbidity and mortality concerns of municipalities. Maturitas. 2018;114:54–59. doi:10.1016/j.maturitas.2018.06.002
28. Karjalainen S. Thermal comfort and gender: a literature review. Indoor Air. 2012;22(2):96–109. doi:10.1111/j.1600-0668.2011.00747.x
29. Kazman JB, Purvis DL, Heled Y, et al. Women and exertional heat illness: identification of gender specific risk factors. US Army Med Dep J. 2015;58–66.
30. Eid AH, Maiti K, Mitra S, et al. Estrogen increases smooth muscle expression of alpha2C-adrenoceptors and cold-induced constriction of cutaneous arteries. Am J Physiol Heart Circ Physiol. 2007;293(3):H1955–H1961. doi:10.1152/ajpheart.00306.2007
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
